INTRODUCTION
EVIDENCE OF THE IMPACT OF PRENATAL MATERNAL DISTRESS ON ALLERGIC DISEASES IN THEIR OFFSPRING
Table
Published cohort or registry studies examining the association between prenatal maternal distress and allergic diseases in offspring
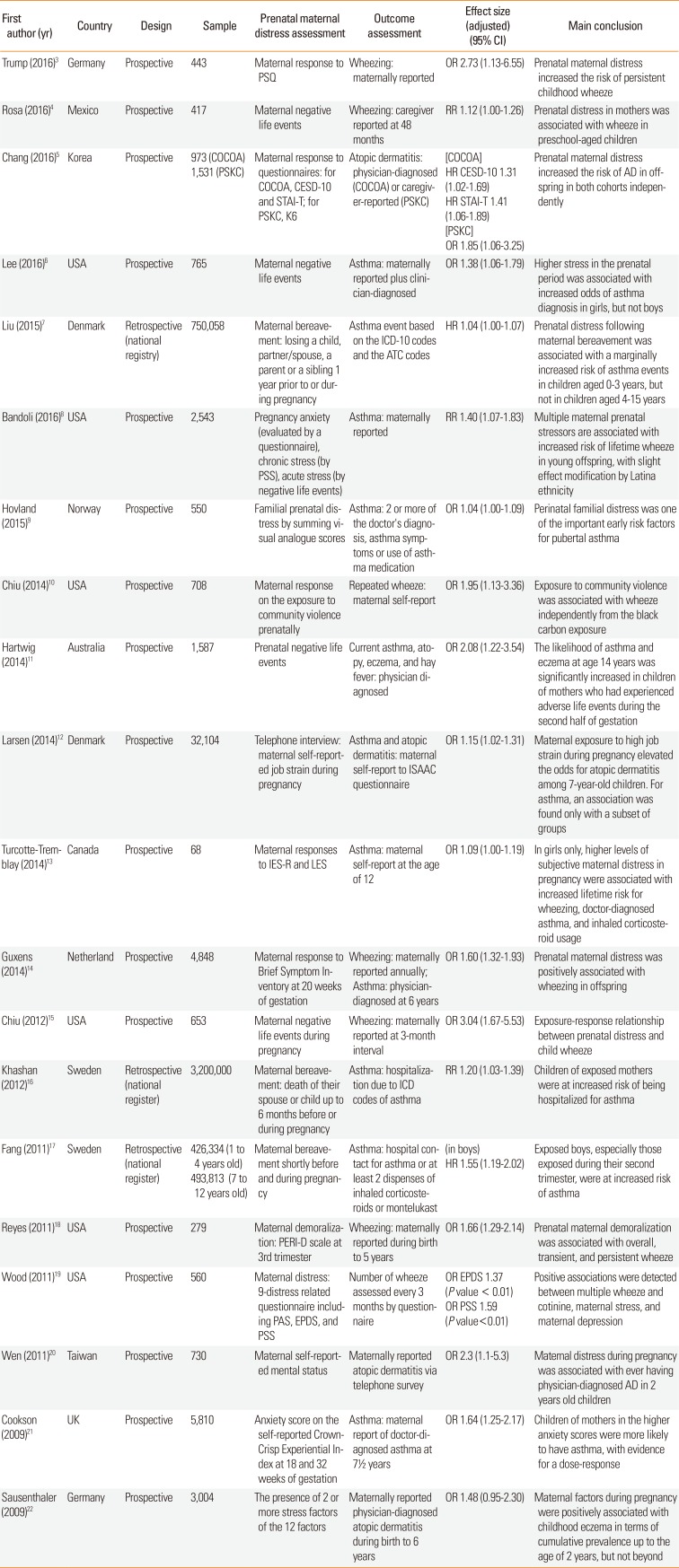
| First author (yr) | Country | Design | Sample | Prenatal maternal distress assessment | Outcome assessment | Effect size (adjusted) (95% CI) | Main conclusion |
|---|---|---|---|---|---|---|---|
| Trump (2016)3 | Germany | Prospective | 443 | Maternal response to PSQ | Wheezing: maternally reported | OR 2.73 (1.13–6.55) | Prenatal maternal distress increased the risk of persistent childhood wheeze |
| Rosa (2016)4 | Mexico | Prospective | 417 | Maternal negative life events | Wheezing: caregiver reported at 48 months | RR 1.12 (1.00–1.26) | Prenatal distress in mothers was associated with wheeze in preschool-aged children |
| Chang (2016)5 | Korea | Prospective |
973 (COCOA) 1,531 (PSKC) |
Maternal response to questionnaires: for COCOA, CESD-10 and STAI-T; for PSKC, K6 | Atopic dermatitis: physician-diagnosed (COCOA) or caregiver-reported (PSKC) |
[COCOA] HR CESD-10 1.31 (1.02–1.69) HR STAI-T 1.41 (1.06–1.89) [PSKC] OR 1.85 (1.06-3.25) |
Prenatal maternal distress increased the risk of AD in off-spring in both cohorts independently |
| Lee (2016)6 | USA | Prospective | 765 | Maternal negative life events | Asthma: maternally reported plus clinician-diagnosed | OR 1.38 (1.06–1.79) | Higher stress in the prenatal period was associated with increased odds of asthma diagnosis in girls, but not boys |
| Liu (2015)7 | Denmark | Retrospective (national registry) | 750,058 | Maternal bereave- ment: losing a child, partner/spouse, a parent or a sibling 1 year prior to or during pregnancy | Asthma event based on the ICD-10 codes and the ATC codes | HR 1.04 (1.00–1.07) | Prenatal distress following maternal bereavement was associated with a marginally increased risk of asthma events in children aged 0-3 years, but not in children aged 4-15 years |
| Bandoli (2016)8 | USA | Prospective | 2,543 | Pregnancy anxiety (evaluated by a questionnaire), chronic stress (by PSS), acute stress (by negative life events) | Asthma: maternally reported | RR 1.40 (1.07–1.83) | Multiple maternal prenatal stressors are associated with increased risk of lifetime wheeze in young offspring, with slight effect modification by Latina ethnicity |
| Hovland (2015)9 | Norway | Prospective | 550 | Familial prenatal distress by summing visual analogue scores | Asthma: 2 or more of the doctor's diagnosis, asthma symptoms or use of asth- ma medication | OR 1.04 (1.00+1.09) | Perinatal familial distress was one of the important early risk factors for pubertal asthma |
| Chiu (2014)10 | USA | Prospective | 708 | Maternal response on the exposure to community violence prenatally | Repeated wheeze: maternal self-report | OR 1.95 (1.13–3.36) | Exposure to community violence was associated with wheeze independently from the black carbon exposure |
| Hartwig (2014)11 | Australia | Prospective | 1,587 | Prenatal negative life events | Current asthma, atopy, eczema, and hay fever: physician diagnosed | OR 2.08 (1.22–3.54) | The likelihood of asthma and eczema at age 14 years was significantly increased in children of mothers who had experienced adverse life events during the second half of gestation |
| Larsen (2014)12 | Denmark | Prospective | 32,104 | Telephone interview: maternal self-reported job strain during pregnancy | Asthma and atopic dermatitis: maternal self-report to ISAAC questionnaire | OR 1.15 (1.02–1.31) | Maternal exposure to high job strain during pregnancy elevated the odds for atopic dermatitis among 7-year-old children. For asthma, an association was found only with a subset of groups |
| Turcotte-Tremblay (2014)13 | Canada | Prospective | 68 | Maternal responses to IES-R and LES | Asthma: maternal self-report at the age of 12 | OR 1.09 (1.00–1.19) | In girls only, higher levels of subjective maternal distress in pregnancy were associated with increased lifetime risk for wheezing, doctor-diagnosed asthma, and inhaled corticosteroid usage |
| Guxens (2014)14 | Netherland | Prospective | 4,848 | Maternal response to Brief Symptom Inventory at 20 weeks of gestation | Wheezing: maternally reported annually; Asthma: physician-diagnosed at 6 years | OR 1.60 (1.32–1.93) | Prenatal maternal distress was positively associated with wheezing in offspring |
| Chiu (2012)15 | USA | Prospective | 653 | Maternal negative life events during pregnancy | Wheezing: maternally reported at 3-month interval | OR 3.04 (1.67–5.53) | Exposure-response relationship between prenatal distress and child wheeze |
| Khashan (2012)16 | Sweden | Retrospective (national register) | 3,200,000 | Maternal bereavement: death of their spouse or child up to 6 months before or during pregnancy | Asthma: hospitalization due to ICD codes of asthma | RR 1.20 (1.03–1.39) | Children of exposed mothers were at increased risk of being hospitalized for asthma |
| Fang (2011)17 | Sweden | Retrospective (national register) |
426,334 (1 to 4 years old) 493,813 (7 to 12 years old) |
Maternal bereavement shortly before and during pregnancy |
Asthma: hospital contact for asthma or at least 2 dispenses of inhaled corticosteroids or montelukast |
(in boys) HR 1.55 (1.19–2.02) |
Exposed boys, especially those exposed during their second trimester, were at increased risk of asthma |
| Reyes (2011)18 | USA | Prospective | 279 | Maternal demoralization: PERI-D scale at 3rd trimester | Wheezing: maternally reported during birth to 5 years | OR 1.66 (1.29–2.14) | Prenatal maternal demoralization was associated with overall, transient, and persistent wheeze |
| Wood (2011)19 | USA | Prospective | 560 | Maternal distress: 9-distress related questionnaire including PAS, EPDS, and PSS | Number of wheeze assessed every 3 months by questionnaire |
OR EPDS 1.37 (P value < 0.01) OR PSS 1.59 (P value<0.01) |
Positive associations were detected between multiple wheeze and cotinine, maternal stress, and maternal depression |
| Wen (2011)20 | Taiwan | Prospective | 730 | Maternal self-reported mental status | Maternally reported atopic dermatitis via telephone survey | OR 2.3 (1.1–5.3) | Maternal distress during pregnancy was associated with ever having physician-diagnosed AD in 2 years old children |
| Cookson (2009)21 | UK | Prospective | 5,810 | Anxiety score on the self-reported Crown-Crisp Experiential Index at 18 and 32 weeks of gestation | Asthma: maternal report of doctor-diagnosed asthma at 7½ years | OR 1.64 (1.25–2.17) | Children of mothers in the higher anxiety scores were more likely to have asthma, with evidence for a dose-response |
| Sausenthaler (2009)22 | Germany | Prospective | 3,004 | The presence of 2 or more stress factors of the 12 factors | Maternally reported physician-diagnosed atopic dermatitis during birth to 6 years | OR 1.48 (0.95–2.30) | Maternal factors during pregnancy were positively associated with childhood eczema in terms of cumulative prevalence up to the age of 2 years, but not beyond |
AD, atopic dermatitis; ATC, Anatomical Therapeutic Chemical Classification; CESD-10, the 10 item Center for Epidemiologic Studies Depression Scale; CI, confidence interval; COCOA, the COhort for Childhood Origin of Asthma and allergic diseases; EPDS, Edinburgh Postnatal Depression Scale; HR, hazard ratio; ICD-10, International Classification of Diseases, Tenth Edition; IES-R, Impact of Event Scale-Revised; ISAAC, International Study of Asthma and Allergies in Childhood; LES, Life Experiences Survey; OR, odds ratio; PAS, Pregnancy Anxiety Scale; PERI-D, psychiatric epidemiology research interview-demoralization, PSKC, Panel Study on Korean Children; PSQ, Perceived Stress Questionnaire; PSS, Perceived Stress Scale; RR, relative risk; STAI-T, State Trait Anxiety Inventory-Trait scale.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download