Atopic dermatitis (AD) is a common chronic relapsing inflammatory skin disease which is characterized by itching, dry skin, and inflammation, as well as exudation, and frequently associated with a personal or familial history of allergic diseases.1 Hypersensitivity reaction to environmental agents has been suggested to be the pathogenetic mechanism responsible for the development and maintenance of chronic skin inflammation in AD patients.1 However, the pathogenetic mechanism underlying AD seems to be more complexly associated with genetic abnormalities, environmental triggering factors, skin barrier defects, and immune dysfunction. In addition, the precise pathogenetic mechanism underlying AD is not yet completely understood.1
Obesity is medical status in which excess body fat has accumulated to the extent that it may have a negative effect on health, leading to reduced life expectancy and/or increased health problems.23 People are considered obese when their body mass index (BMI), a measurement obtained by dividing a person's weight by the square of the person's height, is over 30 kg/m2, with the range 25-30 kg/m2 defined as overweight. Obesity increases the likelihood of various diseases, including heart disease, type 2 diabetes, obstructive sleep apnea, certain types of cancer, and osteoarthritis.2 Obesity is most commonly caused by a combination of excessive food energy intake, lack of physical activity, environmental, and genetic susceptibility.2
In this issue, an analysis of cross-sectional nation-wide survey of 5,202 Korean young adults aged 19-40 years showed that obesity was positively related to the presence of AD in women and that unmarried status was more frequently observed in AD patients compared to subjects without AD in both females and males.4
A recently published meta-analysis of epidemiological studies on the association between AD and obesity showed that obesity is associated with an increased prevalence of AD in children and adults from studies of North America and Asia.5 The positive association between AD and obesity can be interpreted by 2 ways in a pathogenetic view point. First, obesity causes AD by providing chronic inflammatory status and this status induce immune dysfunction and hypersensitivity, and subsequently lead to AD. Secondly, sedentary life-style and/or bad diet habits induce both AD and obesity and an association between AD and obesity, is an epiphenomenon. In a recent case-control study from Chinese adults, the prevalence of obesity was 6.7% in healthy controls and 15.6% in patients with AD (P=0.02).6 This data can be used as a statistical evidence for a significant association between obesity and AD. However, the data also suggests that obesity is not present in 84.4% of AD and cannot work as a causal factor in the majority of patients with AD. Thus, a careful interpretation of the currently available epidemiological reports and clinical experience indicates that the association between AD and obesity is an epiphenomenon.
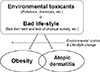
The main purpose of epidemiological analysis on a certain disease is exploring the real cause and mechanism responsible for the disease development to archive the prevention and cure of the disease. The significant epidemiological association between obesity and AD suggests that common etiological factors might play roles in the development of both obesity and AD. The question on the real cause and pathogenetic mechanism underlying allergic disease can obtain a clue to answer by searching attributing factors associated with the dramatic rapid increase in the prevalence of allergic diseases, including asthma, allergic rhinitis, AD, and food allergy in the last few decades.78 Many investigators have suggested that environmental toxicants, prolonged stay indoors, sedentary work, inadequate physical activity, and stressful life-style might responsible for both 'allergy epidemics and obesity'.79 The significant association between obesity and AD also supports that environmental factors and life-style responsible for the development of obesity, including bad diet habit and lack of physical activity, could also responsible for the development of AD (Fig. 1).
Another interesting finding from epidemiological analysis on the association between allergic diseases and obesity using Korea National Health and Nutritional Examination Survey is that obesity is a significant risk factor for both asthma and AD in women but not in man.49 It is of interest to note that in many studies cited above, the relationship between obesity and atopy is predominant in women, mostly post-pubertal.3 Obesity can influence sex hormones by increasing the plasma concentration of 17-beta estradiol because aromatase (an enzyme contributing to the transformation of androgens to estrogens) is present at a high concentration in the fat. Estrogens are known to have pro-inflammatory properties on immune cells in experimental conditions.3 These suggest a possibility that pro-inflammatory status stimulated by increased plasma concentrations of estrogens could promote the development of AD and asthma in obese women. However, the contribution of obesity and estrogen to the development of AD and asthma should be further studied.
The patients with AD have been reported to experience significant amounts of physical and psychological stresses. AD can affect sleep, mood, and quality of life.1011 Patients with AD show significantly higher levels of suicidal ideation, anxiety, and depression compared to healthy subjects (Fig. 2). These can result in psychosocial difficulties affecting personal relationships.1011 AD causes a significant burden on the patient, family, and society.10 However, the degree and amount of social impact of AD except for medical costs cannot be easily estimated by statistical methods. There have been few reports on married status and AD in epidemiological studies. In the report of this issue, unmarried status was significantly frequently observed in AD patients compared to subjects without AD in both females and males by analyzing the cross-sectional nation-wide survey of 5,202 young Korean adults aged 19-40 years (P<0.001).4 This result provides objective evidence that AD has a significant social impact. Further studies of AD as a significant social problem are warranted.
Currently, AD is a significant medicosocial problem in many developed countries.1 AD has numerous different aspects in the view point of pathogenesis and treatment, including genetic disorders, environmental factors skin diseases, immune disorders, allergic diseases, and life-style changes.1 Currently, physicians mainly focus on the temporary alleviation of clinical symptoms of AD by medications. The majority of physicians are focusing on the skin and the immune system for the treatment and prevention of AD because these approaches are easy and practical. However, these approaches are frequently disappointing to both patients and physicians in the aspect of treatment outcome. Furthermore, the unmet medical needs from patients and their families wanting the cure of AD are resulting in significant socio-economic burdens in many countries.1 New therapeutic approaches to AD as life-style disease and/or environmental disease can provide new strategies for the prevention and treatment of AD by modifying of life-style and living environment, although these approaches might be more difficult than current approaches with medical treatment. Future development of new strategies for causal treatment and prevention of allergic diseases will ultimately solve medicosocial problems associated with current epidemics of allergic diseases.
Figures and Tables
ACKNOWLEDGMENTS
This work was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean Government (MSIP) (No. 2014R1A2A1A11049386).
References
1. Nahm DH. Personalized Immunomodulatory Therapy for Atopic Dermatitis: an Allergist's View. Ann Dermatol. 2015; 27:355–363.
2. Kopelman PG. Obesity as a medical problem. Nature. 2000; 404:635–643.
3. Boulet LP. Obesity and atopy. Clin Exp Allergy. 2015; 45:75–86.
4. Lee JH, Han KD, Jung HM, Youn YH, Lee JY, Park YG, et al. Association between obesity, abdominal obesity, and adiposity and the prevalence of atopic dermatitis in young Korean adults: the Korea national health and nutrition examination survey 2008-2010. Allergy Asthma Immunol Res. 2016; 8:107–114.
5. Zhang A, Silverberg JI. Association of atopic dermatitis with being overweight and obese: a systematic review and metaanalysis. J Am Acad Dermatol. 2015; 72:606–616.
6. Luo X, Xiang J, Dong X, Cai F, Suo J, Wang Z, et al. Association between obesity and atopic disorders in Chinese adults: an individually matched case-control study. BMC Public Health. 2013; 13:12.
7. Platts-Mills TA. The allergy epidemics: 1870-2010. J Allergy Clin Immunol. 2015; 136:3–13.
8. Gorgievska-Sukarovska B, Lipozencić J, Susac A. Obesity and allergic diseases. Acta Dermatovenerol Croat. 2008; 16:231–235.
9. Jeon JY, Ha KH, Kim DJ. New risk factors for obesity and diabetes: Environmental chemicals. J Diabetes Investig. 2015; 6:109–111.
10. Carroll CL, Balkrishnan R, Feldman SR, Fleischer AB Jr, Manuel JC. The burden of atopic dermatitis: impact on the patient, family, and society. Pediatr Dermatol. 2005; 22:192–199.
11. Noh HM, Cho JJ, Park YS, Kim JH. The relationship between suicidal behaviors and atopic dermatitis in Korean adolescents. J Health Psychol. 2015; [Epub ahead of print].




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download