Abstract
The basophil activation test (BAT) has been suggested as a complementary method for diagnosing drug allergies. The aim of this study was to evaluate the clinical utility of this test in patients with drug-induced anaphylaxis. In total, 19 patients, all of whom had a history of moderate to severe anaphylaxis, were enrolled. None of the causative drugs had available in vitro tests or reliable skin tests; these drugs included, among others, first and second-generation cephalosporins, H2 blockers, and muscle relaxants. The BAT yielded positive results in 57.9% of the cases, which was similar those results of skin prick and intradermal tests (42.1% and 57.9%, respectively). When basophils were double labelled with CD63 and CD203c, both of which are basophil activation markers, the positive rate was increased from 57.9% to 73.7%. Therefore, the results of this study confirm that the BAT is a quick, reliable, and safe diagnostic tool for patients with drug-induced anaphylaxis.
Anaphylaxis is a severe and life-threatening hypersensitivity reaction, and its occurrence rate appears to be increasing.12 Antibiotics, especially β-lactams, nonsteroidal anti-inflammatory drugs (NSAIDs), and chemotherapeutic agents are often implicated in drug reactions;23 however, any medication or biological agent can potentially trigger anaphylaxis. For the assessment of drug-induced anaphylaxis, most physicians rely on a patient's clinical history and correlate the timing of symptoms with exposure. In vitro testing for drug allergy is necessary to determine the exact cause of the reaction, and to reduce the risk of re-exposure and prevent the unnecessary withdrawal of medications. Diagnostic tools have primarily focused on IgE-mediated anaphylaxis, and skin prick tests (SPTs), intradermal drug tests (IDTs), and drug-specific IgE testing have all been implemented.4 However, with the exception of several β-lactam antibiotics, pure reagents for in vivo or in vitro tests for most medications are not commercially available.
The basophil activation test (BAT) is a flow cytometry-based assay in which the expression of activation markers on the surface of basophils is measured following stimulation with an allergen. The BAT has been validated in IgE-mediated conditions, including food allergies, venom hypersensitivity, and pollen allergies.56 In terms of drug allergies, the BAT may be useful for confirming clinical suspicions without performing dangerous drug challenge tests in cases where no alternative tests are available.
The aim of this study was to evaluate the usefulness of BATs in patients with drug-induced anaphylaxis, in whom in vivo tests were considered highly risky, or when commercial antigens were not available.
Patients who had been referred for diagnostic evaluation after experiencing a drug-induced hypersensitivity reaction were included in the study. In this study, anaphylaxis was defined based on the criteria proposed at the second anaphylaxis symposium.17 SPTs and IDTs were performed using a culprit drug in all patients, and all procedures followed the criteria of the European Network for Drug Allergy.8 In certain cases, oral challenge tests were performed with associated drugs, but not with the suspected drug to ensure that they were tolerated, thus restricting causality to the suspected drug. Clinical characteristics and demographic data were collected for each patient. Serum total IgE was measured, and specific IgE was determined using immunoCAP assays (Thermo Fisher Scientific Inc., Waltham, MA, USA) when available. SPTs were performed for common inhalant allergens (Allergopharma, Germany), and atopy was defined as a positive SPT result. The study was approved by the Hallym University Sacred Heart Hospital Ethics Committee, and written informed consent was obtained from each subject.
Blood samples were drawn from the patients at least 2 weeks post-hypersensitivity reaction. BATs were performed as previously described.9 Blood was collected in an EDTA tube, and red blood cells were lysed using ammonium chloride lysis buffer within 3 hours of sampling. After washing and re-suspending the cells in PBS with 0.1% human serum albumin, the cells (200 µL) were stimulated (30 minutes, 37℃) with buffer containing a positive control (anti-IgE 1 µg/mL; KPL, Gaithersburd, MD, USA, A23187 3 µM; Sigma, St. Louis, MO, USA), a negative control (without any treatment), or serial dilutions of the drug (approximately, 8-10 dilution steps). Cells were then stained with 2 µL of a mixture containing anti-human CD123-FITC, anti-human HLA-DR-APC, anti-human CD63-PE-conjugated antibodies (BD, Biosciences, San Jose, CA, USA), and anti-CD203c-PE-conjugated antibodies (Beckman Coulter, Marseille Cedex, France) for 40 minutes at room temperature. Basophil activation was evaluated by flow cytometric analysis (FACSCalibur; BD, Immunocytometry Systems, San Jose, CA, USA). Results are expressed as the percentage of CD63+ or CD203c+ basophils; a stimulation index (SI) ≥2 and an absolute activated basophil percentage ≥5 were considered positive BAT responses.
All statistical analyses were performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Because the number of subjects was small, continuous variables were analyzed using the Mann-Whitey U test, and categorical variables were analyzed using Fisher's exact test. A Spearman's rank-order correlation test was used to analyze changes in the basophil surface expression of CD63 and CD203c. A P value <0.05 was considered significant.
The demographic and clinical characteristics of the study subjects are shown in Tables 1 and 2. Nineteen patients, 9 men and 10 women, ranging in age from 21 to 70 years, were enrolled. Twelve patients (63.2%) had a history of an allergic reaction to the same culprit drug, and 5 experienced severe anaphylaxis. Cephalosporin antibiotics were involved in 8 patients, ranitidine in 3, eperisone in 2, and streptomycin, insulin, propofol, paclitaxel, tridol, and glimepiride in 1 patient each. The immunoCAP assays of penicilloyl G, penicilloyl V, amoxicilloyl, ampicilloyl, and cefaclor were performed in patients with cephalosporin antibiotics (Patient 1-8), however, only 1 patient (Patient 7) showed a positive result of cefaclor immunoCAP assay (9.96 KU/L, class 3).
Eleven of 19 (57.9%) patients showed an upregulation of basophil cell surface CD203c and CD63 in response to drug stimulation. The basophils of 14 patients (73.7%) showed an upregulation of 1 marker (CD63 or CD203c). There was a significant positive correlation between the degrees of CD63 and CD203c upregulation (P=0.008); however, the positive rates of the 2 markers were not significantly correlated (P=0.181). Five patients showed negative responses to both CD63 and CD203c, and the other 6 patients showed discordant testing results (Table 2). Fourteen patients (73.7%) had positive responses to either the SPT or the IDT. Eight of 18 patients (42.1%) had positive responses to the SPT, and 11 of 14 patients (57.9%), excluding the 5 patients with severe anaphylaxis responses, had positive IDT responses.
The results of BATs and skin tests were not correlated in this study (P=0.530). All 3 patients with ranitidine-induced anaphylaxis (Patient 10-12 in Table 2) had severe reactions and positive SPTs results but no response to the BAT. One patient with cefaclor hypersensitivity (Patient 5) reacted positively only to the BAT and not to the SPT or to cefaclor-specific IgE. Each patient with eperisone- or propofol-induced anaphylaxis (Patient 13, Patient 16) had a negative response to the SPT, but the basophil expression of both CD203c and CD63 was upregulated.
For the diagnosis of drug-induced anaphylaxis, BATs yielded positive results in 57.9% of the cases, which was comparable to SPT and IDT rates (42.1% and 57.9%, respectively). The IDT was a sensitive diagnostic method in this study; however, 5 patients were excluded from IDTs due to concerns over systemic hypersensitivity reactions, and the culprit drug in 2 of these patients was confirmed by the BAT. Therefore, the BAT is a useful tool for the diagnosis of drug-induced anaphylaxis, particularly in cases where anaphylaxis is caused by new or unrecognised drugs or in situations where physicians are unable to measure drug-specific IgE or to perform IDTs.
In this study, basophils were double labelled with 2 activation markers, CD63 and CD203c. When both markers were combined, the positive testing rate increased to from 57.9% to 73.7%. When the SI was calculated using either CD63 or CD203c, the positive rate of each marker was the same in our patients; however, discordances between the BAT results for the 2 markers were found in some patients, suggesting that the BAT may yield false positives or that basophil activation markers of CD63 and CD203c may have intra-individual variability. Although both CD63 and CD203c have been validated as acceptable markers for the BAT, recent studies have reported that these markers are differentially expressed in various allergic conditions.10 In a comparative study of the sensitivity of CD63 and CD203c in IgE-mediated amoxicillin allergies, CD203c sensitivity is superior to CD63.11 In contrast, patients with non-allergic NSAID hypersensitivity upregulate CD63 expression more frequently than CD203c expression.12 In this study, basophils of patients with cefaclor-induced anaphylaxis upregulated CD203c, but not CD63. However, other drugs, including tridol and glimepiride, resulted in only CD63 upregulation, suggesting that different drugs regulate the expression of different markers.
Three patients (with reactions to cefaclor, eperisone, or propofol) had positive results only to the BAT; in these cases, both CD63 and CD203c were upregulated. The skin test results of these patients may have been false negatives, or another mechanism, such as non-IgE mediated or direct basophil activation, may have been involved. In contrast, 3 cases had positive results only to the SPT, but not to the BAT, suggesting that these patients may react to ranitidine metabolites. Previous case reports have documented the positive results of skin tests to ranitidine and, as was the case with this study, the detection rate of serum specific IgE was relatively low compared to other skin tests.131415 Taken together, these results suggest that ranitidine metabolites conjugated to body proteins may be involved in IgE-mediated reactions, even though the antigenic determinant of ranitidine remains unknown.
In conclusion, the BAT is particularly useful in patients with life-threatening anaphylaxis, in whom a drug provocation test is not advisable, and when other diagnostic tools are not possible. Although BAT has a false-negative risk due to the type of drug or drug metabolite, the diagnostic yield was increased in this study by the simultaneous measurement of CD63 and CD203c. In actual practice, the BAT can serve as a quick, reliable, and safe diagnostic tool.
Figures and Tables
Table 1
Demographic features and clinical characteristics

Values are given as number (%), unless otherwise indicated.
*The severity of anaphylaxis was graded as mild, moderate, or severe, using a previously established grading system. Mild reactions were defined by presentation of only cutaneous symptoms. Moderate symptoms were exhibited when respiratory, cardiovascular, or gastrointestinal involvement was apparent; whereas hypotension, hypoxia, loss of consciousness, or confusion was considered to reflect severe anaphylaxis (reference 7).
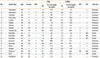
Table 2
Individual results of basophil activation, skin tests, and anaphylaxis severity
References
1. Muraro A, Roberts G, Worm M, Bilò MB, Brockow K, Fernández Rivas M, et al. Anaphylaxis: guidelines from the European Academy of Allergy and Clinical Immunology. Allergy. 2014; 69:1026–1045.
2. Ye YM, Kim MK, Kang HR, Kim TB, Sohn SW, Koh YI, et al. Predictors of the severity and serious outcomes of anaphylaxis in korean adults: a multicenter retrospective case study. Allergy Asthma Immunol Res. 2015; 7:22–29.
3. Romano A, Warrington R. Antibiotic allergy. Immunol Allergy Clin North Am. 2014; 34:489–506.
4. Uyttebroek AP, Sabato V, Bridts CH, Ebo DG. In vitro diagnosis of immediate IgE-mediated drug hypersensitivity: warnings and (unmet) needs. Immunol Allergy Clin North Am. 2014; 34:681–689.
5. Ebo DG, Sainte-Laudy J, Bridts CH, Mertens CH, Hagendorens MM, Schuerwegh AJ, et al. Flow-assisted allergy diagnosis: current applications and future perspectives. Allergy. 2006; 61:1028–1039.
6. Hoffmann HJ, Santos AF, Mayorga C, Nopp A, Eberlein B, Ferrer M, et al. The clinical utility of basophil activation testing in diagnosis and monitoring of allergic disease. Allergy. 2015; 70:1393–1405.
7. Brown SG. Clinical features and severity grading of anaphylaxis. J Allergy Clin Immunol. 2004; 114:371–376.
8. Brockow K, Garvey LH, Aberer W, Atanaskovic-Markovic M, Barbaud A, Bilo MB, et al. Skin test concentrations for systemically administered drugs -- an ENDA/EAACI Drug Allergy Interest Group position paper. Allergy. 2013; 68:702–712.
9. Ebo DG, Bridts CH, Hagendorens MM, Aerts NE, De Clerck LS, Stevens WJ. Basophil activation test by flow cytometry: present and future applications in allergology. Cytometry B Clin Cytom. 2008; 74:201–210.
10. Leysen J, Sabato V, Verweij MM, De Knop KJ, Bridts CH, De Clerck LS, et al. The basophil activation test in the diagnosis of immediate drug hypersensitivity. Expert Rev Clin Immunol. 2011; 7:349–355.
11. Abuaf N, Rostane H, Rajoely B, Gaouar H, Autegarden JE, Leynadier F, et al. Comparison of two basophil activation markers CD63 and CD203c in the diagnosis of amoxicillin allergy. Clin Exp Allergy. 2008; 38:921–928.
12. Abuaf N, Rostane H, Barbara J, Toly-Ndour C, Gaouar H, Mathelier-Fusade P, et al. Comparison of CD63 Upregulation Induced by NSAIDs on Basophils and Monocytes in Patients with NSAID Hypersensitivity. J Allergy (Cairo). 2012; 2012:580873.
13. Jin HJ, Kim JE, Ye YM, Chang YS, Park HS. Ranitidine-induced anaphylaxis with detection of serum specific IgE to ranitidine and human serum albumin conjugates. Ann Allergy Asthma Immunol. 2012; 108:210–212.
14. Koh YI, Park HS, Choi IS. Ranitidine-induced anaphylaxis: detection of serum specific IgE antibody. Allergy. 2006; 61:269–270.
15. Aouam K, Bouida W, Ben Fredj N, Chaabane A, Boubaker H, Boukef R, et al. Severe ranitidine-induced anaphylaxis: a case report and literature review. J Clin Pharm Ther. 2012; 37:494–496.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download