Abstract
Purpose
The Asia-Pacific Burden of Respiratory Diseases (APBORD) study is a cross-sectional, observational one which has used a standard protocol to examine the disease and economic burden of allergic rhinitis (AR), asthma, chronic obstructive pulmonary disorder (COPD), and rhinosinusitis across the Asia-Pacific region. Here, we report on symptoms, healthcare resource use, work impairment, and associated costs in Korea.
Methods
Consecutive participants aged ≥18 years with a primary diagnosis of asthma, AR, COPD, or rhinosinusitis were enrolled. Participants and their treating physician completed a survey detailing respiratory symptoms, healthcare resource use, and work productivity and activity impairment. Costs included direct medical cost and indirect cost associated with lost work productivity.
Results
The study enrolled 999 patients. Patients were often diagnosed with multiple respiratory disorders (42.8%), with asthma/AR and AR/rhinosinusitis the most frequently diagnosed combinations. Cough or coughing up phlegm was the primary reason for the medical visit in patients with a primary diagnosis of asthma and COPD, whereas nasal symptoms (watery runny nose, blocked nose, and congestion) were the main reasons in those with AR and rhinosinusitis. The mean annual cost for patients with a respiratory disease was US$8,853 (SD 11,245) per patient. Lost productivity due to presenteeism was the biggest contributor to costs.
Chronic respiratory disease accounts for 4 million deaths annually, 4% of the global burden of disease, and 8.3% of chronic disease burden.1 Chronic obstructive pulmonary disorder (COPD) is one of the main causes of mortality in Korea.2 The prevalence of asthma, allergic rhinitis (AR), and rhinosinusitis is also increasing and has become the major health priority in Korea.3456 These preventable chronic respiratory diseases have a major adverse impact on quality of life, disability, and productivity, resulting in an increased socioeconomic burden.
Several recent retrospective analyses have used in Korean national health insurance databases to estimate the economic burden of asthma, AR, and COPD.7891011 These studies have provided an immediate insight into the economic burden to the Korean healthcare system; however, there is a lack of data assessing the broader impact of respiratory disease on patients (e.g., symptoms and impact on work productivity). Furthermore, there is limited data exploring the overall disease burden of multiple respiratory diseases using a standardised approach. A comprehensive understanding of the overall disease burden is important for identifying key signaling symptoms for respiratory disorders and for identifying cost-effective treatment strategies to minimize their impact and to appropriately allocate healthcare resources.
The Asia-Pacific Burden of Respiratory Diseases (APBORD) study is a cross-sectional, observational one which has used a standard protocol to examine the disease and economic burden of AR, asthma, COPD, and rhinosinusitis across the Asia-Pacific redion.1213 Here, we report the burden of respiratory diseases, including symptoms, healthcare resource use (HCRU), work impairment, and associated costs in Korea.
This study formed part of the large multi-country, cross-sectional, observational study of adult patients receiving care for respiratory disease across 6 countries in the Asia-Pacific region (India, Korea, Malaysia, Singapore, Taiwan, and Thailand). The study consisted of site-based surveys administered to patients and physicians presenting with a primary diagnosis of respiratory disease during a routine visit to a healthcare provider. In Korea, subjects were recruited from 2 hospitals and 6 clinics between November 2012 and February 2013. The study was approved by Institutional Review Boards at Seoul National University Medical Center and Konkuk University Medical Center.
Patients presenting consecutively at each study site were assessed by the physician (respiratory specialist or primary care physician) during a routine consultation. The physician ascertained that the primary reason for the patient's visit was to receive care for respiratory disease. All patients receiving care for respiratory disease were screened for eligibility to participate in the study. Eligibility criteria included consecutive patients aged ≥18 years receiving care for a primary diagnosis of asthma, AR, COPD, or rhinosinusitis. Subjects were excluded if they had participated in any interventional clinical study within the 12 weeks prior to entering the current study. A patient could only participate in the study once, and no follow-up visits were recorded. Eligible patients were invited to participate in the study, and informed consent was obtained from each patient.
During the study visit, physicians completed the Screening and Consent Log as well as the Physician Survey. The Consent Log captured the basic demographics and respiratory diagnosis of each eligible patient, and information on whether an eligible patient consented to participate in the study. The Physician survey comprised questions regarding to the patient's respiratory diagnosis. Physicians indicated which of the 4 diseases was the primary diagnosis and whether the patient had any other of the 4 diseases in addition to the primary diagnosis. Physicians also recorded medication use 4 weeks prior to the study visit and medications prescribed at the current visit.
The diagnosis of respiratory disease was defined by ICD-10 classifications.14 This excluded some infectious and parasitic diseases that may affect the respiratory system (e.g., tuberculosis) as well as neoplasms of the respiratory system. Diagnosis was made by the attending physician using criteria based on international guidelines for asthma, AR, COPD, and rhinosinusitis.15161718 The physician was required to indicate the clinical criteria for the diagnosis from a list of disease criteria adapted from these clinical practice guidelines for any patients with a new diagnosis of any of the 4 diseases. The patients' clinical management and physicians' usual diagnostic practices were not intended to be influenced by participation in the study; however, some patients may have been diagnosed using a more rigorous and standardized approach than prior to commencement of the study. No attempts were made to independently verify or confirm the patient's diagnosis, and no follow-up diagnostic tests were conducted.
Consenting patients completed the Patient Survey which included questions regarding to general demographics, respiratory symptoms, HCRU, and work productivity. Patients listed their respiratory-related symptoms at the current visit and identified their main symptoms leading to the current visit. HCRU included the number of visits to a general practitioner (GP), medical specialist, alternative and traditional medicine practitioner, pharmacist, emergency department, and hospital admissions in previous 4 weeks.
Work productivity was assessed using the Work Productivity and Activity Impairment-Specific Health Problem (WPAI-SHP) questionnaire.19 The WPAI-SHP measures amounts of absenteeism (work time lost) and presenteeism (lost on-the-job productivity) as well as daily activity impairment attributable to a specific health problem. The recall period in this questionnaire is 7 days.
A broad societal perspective was adopted for cost analysis. The costs were collected based on government and patient costs. Unit costs were sourced from Health Insurance Review and Assessment (HIRA) and Korean Statistical Information Service (KOSIS). Average costs were calculated using the unit cost of the healthcare resource use item multiplied by reported HCRU in previous 4 weeks plus the current visit to the GP or specialist. For each medication class, one medication representative of the most commonly prescribed medication for respiratory disease was identified. The Dosing and duration of medication use was according to therapeutic guidelines.12 Lost productivity costs were calculated by multiplying the overall productivity lost from the WPAI questionnaire by the average monthly wage (estimated at KRW 3,259,799 from ILO Global Wage Database 2012). Four-week costs were multiplied by 2 to estimate annual costs. Costs were presented in USD using the exchange rate for September 15, 2014: 1 USD=1,040.20 KRW.
Statistical analyses were performed using SAS® for Windows, version 9.3 (SAS Institute Inc., Cary, NC, USA). The demographics and clinical characteristics of the patients were described using mean (SD) for continuous variables and number (percentage) for categorical variables. The percentage and 95% confidence intervals of the patient with each disease entity was calculated using the exact (Clopper-Pearson) method.
A total of 4,439 patients were diagnosed with a respiratory disease and subsequently screened across 2 hospitals and 6 clinics in Korea. Of these, 4,439 patients 1,779 (40.1%) were considered eligible after screening, with 999 (56.2%) patients consenting and being enrolled in the study.
The mean (SD) age of the enrolled patients was 48.2 (SD 17.28) years, 58.4% of whom were female (Table). There were 50.6% of patients employed full-time or part-time. Sixty-four percent of the patients had never smoked. Of patients who had ever smoked, 39.3% were current smokers.
The most frequent primary diagnosis was AR (55.7%, 95%CI: 52.5%, 58.8%), followed by asthma (31.8%, 95%CI: 29.0%, 34.8%), rhinosinusitis (6.9%, 95%CI: 5.4%, 8.7%), and COPD (5.6%, 95%CI: 4.3%, 7.2%). Patients were frequently diagnosed with multiple respiratory diseases (Fig. 1). Overall, 428 (42.8%) of patients were diagnosed with a combination of the 4 diseases of interest. In particular, a large percentage of patients were diagnosed with a combination of one or more of the 4 diseases of interest (74.3%). The most common combination was AR plus asthma, with or without other conditions (232 patients, 23.2% of the total patients enrolled) and AR plus rhinosinusitis, with or without other conditions, (154 patients, 15.4% of the total patients enrolled).
To identify the main symptoms associated with each disease, patients were asked to report which symptom was their main reason for their current visit and to list all their current symptoms at the current visit (Fig. 2). Cough or coughing up phlegm was the most frequently reported main reason for the hospital visit for patients diagnosed with COPD (47.5%), and asthma (33.7%). For patients with a primary diagnosis of rhinosinusitis, blocked nose or congestion (21.7%) and cough or coughing up phlegm (20.3%) were the most frequently reported main reasons for the hospital visit. For patients with a primary diagnosis of AR, watery, runny nose (24.0%), and blocked nose and congestion (23.3%) were the most common main reasons.
Enrolled patients reported their HCRU associated with their main respiratory symptom in the 4 weeks prior to the hospital visit (Fig. 3). A larger percentage of patients with a primary diagnosis of AR and rhinosinusitis reported GP and specialist visits than those with asthma and COPD. A larger percentage of patients visited specialists than GP (rhinosinusitis 68.1% vs 23.2%, AR 65.9% vs 24.1%, asthma 44.2% vs 19.1%, and COPD 32.5% vs 10.0%). Few patients reported hospital admission or emergency department attendance for all the 4 diseases.
Medication use was high, with 70.4% of the patients prescribed medicines in the 4 weeks prior to the current visit and 98.3% prescribed medicine at the visit (Fig. 4). Patients with a primary diagnosis of COPD reported the highest previous medication use (87.5%), followed by those with asthma (80.2%), AR (64.0%), and rhinosinusitis (62.3%). The most frequently used medication was fixed-dose combination inhalers for asthma and inhaled anticholinergics for COPD. Patients with AR and rhinosinusitis most frequently used antihistamines.
Patients completed the WPAI questionnaire to assess the impact of AR, asthma, COPD, and rhinosinusitis on activity impairment and work productivity loss (Fig. 5). Across all conditions, presenteeism (percentage impairment at work) was a more significant contributor to the productivity loss reported than absenteeism (percentage work time missed). On average, patients with AR (39.5%, SD 28.74) or rhinosinusitis (38.7%, SD 28.93) reported higher productivity loss than those with a primary diagnosis of asthma (32.6%, SD 30.05) and COPD (15.4%, SD 23.30). Activity impairment was similarly impacted across all conditions.
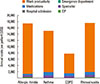
Total costs by primary diagnosis are presented in Fig. 6. Overall, the mean annual cost for patients with a respiratory disease was US$8,853 (SD 11,245) per capita. For patients who reported impairment at work as a result of the disease, the mean annual cost was US$16,367 (SD 11,999) with productivity loss of the highest cost component being US$14,859 (SD 11,947). Patients with a primary diagnosis of rhinosinusitis and asthma had the highest direct medical costs. Medication use was the main driver of direct medical costs for patients with a primary diagnosis of asthma (58.0% of direct medical costs), COPD (57.4%), rhinosinusitis (49.5%), and AR (40.5%). The main driver of direct non-medical costs was specialist visits for all 4 diseases (AR, 42.9%; COPD, 39.9%; rhinosinusitis, 38.7%; and asthma, 34.3%).
This study investigated the disease burden of 4 highly prevalent respiratory diseases in Korea using a standard protocol. Results of this study demonstrate that patients are frequently diagnosed with multiple respiratory disorders. The mean annual cost for patients with a respiratory disease was US$8,853, with lost productivity being the main contributor to overall costs.
Previous research has shown that patients with concomitant respiratory disease have greater morbidity and health care resource use.20 The present study found that patients were frequently diagnosed with multiple respiratory disorders (42.8%), with asthma/AR and AR/rhinosinusitis being the most frequently diagnosed combinations. This finding is consistent with those of previous studies showing that AR is strongly associated with the development of asthma and rhinosinusitis.521 Early identification of patients with concomitant respiratory disease can lead to improvement in patient outcomes. Kim et al.22 found that following continual treatment, patients with asthma and concomitant rhinosinusitis had similar lung function and HCRU as those with asthma only. Therefore, it is important to identify symptoms that indicate the potential presence of multiple respiratory disorders.
In our study, cough or coughing up phlegm was the primary reason for the medical visit for patients with a primary diagnosis of asthma or COPD, whereas nasal symptoms (watery runny nose, blocked nose, and congestion) were the main reasons in those with AR or rhinosinusitis. Interestingly, a large percentage of patients with rhinosinusitis also reported cough or coughing up phlegm as a main symptom. For patients with AR, the presence of cough may reflect a concomitant respiratory condition, such as asthma and rhinosinusitis. A larger number of patients with asthma or rhinosinusitis present with cough and their frequent association with AR, which suggests that patients with AR presenting with cough should be investigated comprehensively for other serious disorders, especially asthma and rhinosinusitis.
Globally, COPD and asthma have been established as significant contributors to the burden of disease.1 This study found that the economic burden of AR and rhinosinusitis was as great as that of asthma and COPD. Considering the high prevalence of AR and rhinosinusitis in Korea46 and the high frequency with which healthcare providers attended AR patients (approximately half of patients in the current sample had a primary diagnosis of AR), the economic burden of AR in Korea is substantial.
The primary driver of costs for all 4 diseases was indirect costs due to work productivity loss. Previous retrospective cost studies of respiratory diseases in Korea only included lost work productivity from absenteeism due to medical visits and hospitalization.7891011 Subsequently, indirect costs due to work productivity loss were found to be a less significant contributor to overall costs. The current study interviewed patients directly to assess lost work productivity using the WPAI. Presenteeism was shown to be a far bigger contributor factor to lost work productivity than absenteeism from work. WPAI scores were similar between previous studies in the US and European populations.232425 Therefore, medical interventions that prevent lost work productivity would greatly reduce the economic impact of respiratory disease.
Interestingly, patients with a primary diagnosis of COPD had relatively lower costs compared to the other respiratory diseases included in this analysis. There are several potential reasons for this finding. On average, patients with COPD were older and more likely to retire. Therefore, COPD has a less impact on indirect costs associated with lost work productivity. Furthermore, the present study only recruited patients visiting specialists and GPs. Patients with severe COPD are more likely to be managed in hospitals rather than in outpatient departments or clinics. Previous research found that direct healthcare costs were approximately 3 times higher in high-grade COPD compared to milder COPD, with inpatient hospital services being the main driver of costs.9 Finally, evidence suggests that COPD is underdiagnosed and undertreated in Korea.2 Therefore, some patients with COPD may not have been identified for inclusion in this study.
The most significant contributors to direct medical costs were medications and specialist visits for all 4 respiratory diseases. Hospitalization was very infrequent and thus did not contribute significantly to direct medical costs in this study. Similar findings of more frequent medication and outpatient services but low inpatient hospital costs have previously been observed in retrospective cost analyses for AR and asthma.7891011 Furthermore, a previous survey reported that a vast majority of allergic patients in Korea are treated by otolaryngologists rather than GPs.26 Previous studies demonstrated that proper management and high medication use are associated with a reduction in exacerbation requiring hospitalizations and overall direct medical costs.2728 The overall results of APBORD documented that hospitalization was a main driver of costs across the Asia-Pacific region. This suggests that management of patients in Korea can reduce acute exacerbations requiring hospitalizations.
A limitation to the current analysis is that the impacts of respiratory illness on a person's inability to care for family, loss of income, psychological factors, and quality of life were not included. Such intangible costs have been shown to considerably add to the economic burden of respiratory disease.10 This study recruited adult patients presenting to primary care physicians and specialist medical practices in urban settings of convenience; it was not the intention of the study to obtain prevalence estimates that are generalizable to the entire population of the country. As such, study participants may not be entirely representative of the broader population with respiratory disease. Furthermore, only adult patients were recruited from urban center, and results may not be generalizable to either patients under 18 years of age or to rural populations.
In summary, this study provides an insight into the identification and economic burden of respiratory disease in Korea. Timely identification of symptoms is important in implementing effective disease management, especially in patients with multiple respiratory diseases. A future goal for disease management should not only be to reduce direct healthcare costs, such as hospitalisations, but also to prevent work productivity loss.
Figures and Tables
Fig. 2
Main reasons for medical visits and all current symptoms reported by primary diagnosis. COPD, chronic obstructive pulmonary disease.

Fig. 3
Percentage of patients with HCRU in the previous 4 weeks by primary diagnoses. Numbers above columns are the mean number of visits for patients that reported at least one visit. COPD, chronic obstructive pulmonary disease; GP, general practitioner/primary care physician.

Fig. 4
History of medication use for respiratory disease and medications prescribed at the medical visit by primary diagnoses. COPD, chronic obstructive pulmonary disease.

Fig. 5
Mean WPAI scores by primary diagnoses. COPD, chronic obstructive pulmonary disease; WPAI, work productivity and impairment.

Fig. 6
Annual direct and indirect costs for the study population by primary diagnoses. Work productivity costs calculated only for patients that reported impairment at work as a result of the disease. COPD, chronic obstructive pulmonary disease; GP, general practitioner/primary care physician.
Table
Patient demographics by primary diagnoses and practice types

ACKNOWLEDGMENTS
The authors would like to thank Geunhee Yi and Jiyun Lee, both from MSD Korea, for their assistance. Geunhee Yi assisted with review of this manuscript while Jiyun Lee provided project management services during the study duration.
This work was supported by Merck and Co. Shalini Bagga, Shiva Shajjan and Rab Faruqi were employees of Merck and Co. at the time of the study. Santwona Baidya provided consulting services for conduct of this research and manuscript preparation.
References
1. World Health Organization. Global surveillance, prevention and control of chronic respiratory diseases: a comprehensive approach. Geneva: World Health Organization;2007.
2. Yoo KH, Kim YS, Sheen SS, Park JH, Hwang YI, Kim SH, et al. Prevalence of chronic obstructive pulmonary disease in Korea: the fourth Korean National Health and Nutrition Examination Survey, 2008. Respirology. 2011; 16:659–665.
3. Song WJ, Kang MG, Chang YS, Cho SH. Epidemiology of adult asthma in Asia: toward a better understanding. Asia Pac Allergy. 2014; 4:75–85.
4. Rhee CS, Wee JH, Ahn JC, Lee WH, Tan KL, Ahn S, et al. Prevalence, risk factors and comorbidities of allergic rhinitis in South Korea: the Fifth Korea National Health and Nutrition Examination Survey. Am J Rhinol Allergy. 2014; 28:e107–e114.
5. Park HS, Choi GS, Cho JS, Kim YY. Epidemiology and current status of allergic rhinitis, asthma, and associated allergic diseases in Korea: ARIA Asia-Pacific workshop report. Asian Pac J Allergy Immunol. 2009; 27:167–171.
6. Kim YS, Kim NH, Seong SY, Kim KR, Lee GB, Kim KS. Prevalence and risk factors of chronic rhinosinusitis in Korea. Am J Rhinol Allergy. 2011; 25:117–121.
7. Lee YH, Yoon SJ, Kim EJ, Kim YA, Seo HY, Oh IH. Economic burden of asthma in Korea. Allergy Asthma Proc. 2011; 32:35–40.
8. Kim SY, Yoon SJ, Jo MW, Kim EJ, Kim HJ, Oh IH. Economic burden of allergic rhinitis in Korea. Am J Rhinol Allergy. 2010; 24:e110–e113.
9. Kim J, Rhee CK, Yoo KH, Kim YS, Lee SW, Park YB, et al. The health care burden of high grade chronic obstructive pulmonary disease in Korea: analysis of the Korean Health Insurance Review and Assessment Service data. Int J Chron Obstruct Pulmon Dis. 2013; 8:561–568.
10. Kim CY, Park HW, Ko SK, Chang SI, Moon HB, Kim YY, et al. The financial burden of asthma: a nationwide comprehensive survey conducted in the republic of Korea. Allergy Asthma Immunol Res. 2011; 3:34–38.
11. Kim C, Yoo KH, Rhee CK, Yoon HK, Kim YS, Lee SW, et al. Health care use and economic burden of patients with diagnosed chronic obstructive pulmonary disease in Korea. Int J Tuberc Lung Dis. 2014; 18:737–743.
12. Wang DY, Ghoshal AG, Muttalif AR, Lin HC, Thanaviratananich S, Bagga S, et al. Quality of life and economic burden of respiratory disease in Asia-Pacific—Asia-Pacific Burden of Respiratory Diseases (APBORD) study. Value Health Reg Issues. 2016; 9:72–77.
13. Cho SH, Lin HC, Ghoshal A, Muttalif A, Thanaviratananich S, Bagga S, et al. Respiratory disease in the Asia-Pacific region: cough as a key symptom. Allergy Asthma Proc. 2016; 37:131–140.
14. World Health Organization. International statistical classification of diseases and related health problems. 10th rev. ed. Geneva: World Health Organization;2010.
15. Global Initiatives for Asthma. Global strategy for asthma management and prevention (2011 update). [place unknown]: Global Initiatives for Asthma;2011.
16. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for the diagnosis, management, and prevention of chronic obstructive pulmonary disease. [place unknown]: Global Initiative for Chronic Obstructive Lung Disease;2010.
17. Fokkens W, Lund V, Mullol J. European Position Paper on Rhinosinusitis and Nasal Polyps group. European Position Paper on Rhinosinusitis and Nasal Polyps 2007. Rhinol Suppl. 2007; 1–136.
18. Bousquet J, Khaltaev N, Cruz AA, Denburg J, Fokkens WJ, Togias A, et al. Allergic Rhinitis and its Impact on Asthma (ARIA) 2008 update (in collaboration with the World Health Organization, GA(2) LEN and AllerGen). Allergy. 2008; 63:Suppl 86. 8–160.
19. Reilly MC, Zbrozek AS, Dukes EM. The validity and reproducibility of a work productivity and activity impairment instrument. Pharmacoeconomics. 1993; 4:353–365.
20. Bousquet J, Gaugris S, Kocevar VS, Zhang Q, Yin DD, Polos PG, et al. Increased risk of asthma attacks and emergency visits among asthma patients with allergic rhinitis: a subgroup analysis of the improving asthma control trial. Clin Exp Allergy. 2005; 35:723–727.
21. Berrettini S, Carabelli A, Sellari-Franceschini S, Bruschini L, Abruzzese A, Quartieri F, et al. Perennial allergic rhinitis and chronic sinusitis: correlation with rhinologic risk factors. Allergy. 1999; 54:242–248.
22. Kim MH, Jung JW, Cho SH, Min KU, Kang HR. The impact of sinusitis on the long-term clinical outcomes of asthma. Asia Pac Allergy. 2014; 4:222–229.
23. Reilly MC, Tanner A, Meltzer EO. Work, classroom and activity impairment instruments: validation studies in allergic rhinitis. Clin Drug Investig. 1996; 11:278–288.
24. Fletcher MJ, Upton J, Taylor-Fishwick J, Buist SA, Jenkins C, Hutton J, et al. COPD uncovered: an international survey on the impact of chronic obstructive pulmonary disease [COPD] on a working age population. BMC Public Health. 2011; 11:612.
25. Demoly P, Gueron B, Annunziata K, Adamek L, Walters RD. Update on asthma control in five European countries: results of a 2008 survey. Eur Respir Rev. 2010; 19:150–157.
26. Allergies in Asia-Pacific. Allergies in Asia-Pacific™: a landmark survey of nasal allergy sufferers: findings for Korea [Internet]. Seoul: Allergies in Asia-Pacific;2014. cited 2015 Jan 7. Available from: http://www.allergiesinasiapacific.com./pdfs/Korea_FINAL%20100603.pdf.
27. Wouters EF. Economic analysis of the confronting COPD survey: an overview of results. Respir Med. 2003; 97:Suppl C. S3–S14.
28. Bahadori K, Doyle-Waters MM, Marra C, Lynd L, Alasaly K, Swiston J, et al. Economic burden of asthma: a systematic review. BMC Pulm Med. 2009; 9:24.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download