Abstract
Purpose
Seasonal variations in asthma-related hospitalizations and emergency department visits have long been recognized. This study aimed to investigate the seasonal patterns of asthma in children and adolescents who presented at emergency departments in Korea.
Methods
We analyzed the National Emergency Department Information System records from 117 emergency departments in Korea that comprised all of the patients with asthma who were aged 3-18 years and who presented at the emergency departments from 2007 to 2012. The children and adolescents were divided into 3 groups based on their ages, namely, 3-6 years, 7-12 years, and 13-18 years. The data were tabulated, and graphs were created to show the seasonal trends in the monthly numbers of emergency department visits as a consequence of asthma.
Results
A total of 41,128 subjects were identified, and the male-to-female ratio was 1:0.5. General ward admissions comprised 42.6% (n=17,524 patients) of the emergency department visits, and intensive care unit admissions comprised 0.8% (n=335 patients) of the emergency department visits. The monthly numbers of emergency department visits for asthma varied according to the season, with high peaks during fall, which was from September to November, and low levels in summer, which was from June to August.
Asthma is a chronic disease that is associated with reversible respiratory obstruction, hypersensitivity caused by multiple stimuli, and chronic inflammation.1 Clinically, it manifests as the deterioration and resolution of respiratory symptoms. Factors involved in the expression of asthma symptoms and exacerbations include allergens, respiratory infections, and environmental pollutants. In addition, a number of psychological and societal factors can contribute to asthma exacerbations.2
The findings from previous studies have shown definite seasonal changes in relation to asthma symptoms in children and adults. In particular, a number of studies have reported that the numbers of children and adolescents who present at emergency departments (EDs) and are hospitalized because of asthma exacerbations dramatically increase during fall.3456 Preventing exacerbations of asthma symptoms based on investigations of factors associated with these seasonal variations might improve the management of the disease. Furthermore, asthma exacerbations in children and adolescents that require ED visits or hospitalization can lead to absences from school, reductions in the quality of patients' lives, and serious social and economic burdens.7
Although self-management and outpatient care can be undertaken when asthma symptoms become exacerbated, seriously ill patients present at EDs and may require hospitalization. Thus, data about asthmatic patients who present at EDs can be valuable and may enable us to understand reasons for asthma symptom exacerbations.589 Therefore, this study aimed to investigate the seasonal patterns of asthma in children and adolescents who presented at EDs throughout Korea by reviewing their ED data.
This study involved children and adolescents who were aged from 3 to 18 years and who presented at 117 EDs in Korea during the 6-year period from January 2007 until December 2012. The study participants involved patients who had diagnosis codes of J45 and J46, which corresponded to asthma, when they visited the ED or were hospitalized as a result of their ED visits. A retrospective analysis of the National Emergency Department Information System data was conducted to assess the monthly distributions of patients with asthma who presented at the EDs. The children and adolescents were divided into three age groups, namely, 3-6 years, 7-12 years, and 13-18 years. General ward (GW) hospitalizations and intensive care unit (ICU) hospitalizations were analyzed and compared in terms of sex and age.
All of the analyses were conducted using SAS version 9.2 (SAS Institute Inc., Cary, NC, USA). A statistically significant difference was defined as a P value of ≤0.05. Initially, the numbers of ED visits were compared in terms of the calendar month using an analysis of variance, and this analysis concentrated on the highest of the 2 or 3 distinct peaks in the ED visits for asthma that occurred each year. Subsequently, the categorical data were sorted according to age and region, and they were analyzed using the chi-square test to compare the seasonal trends.
The number of asthmatic patients who were younger than 18 years and were diagnosed with asthma after they presented at the EDs was 41,128, and the male-to-female ratio was 1:0.5; hence, there was a higher level of morbidity among males. Of the patients who visited the EDs, 54.4% (22,364 subjects) were 3-6 years of age, 35.4% (14,570 subjects) were 7-12 years of ages, and 10.2% (4,194 subjects) were 13-18 years of age (Table).
The numbers of patients who visited EDs tended to increase annually, and were as follows: 5,534 in 2007, 5,521 in 2008, 7,862 in 2009, 7,358 in 2010, 8,563 in 2011, and 6,290 in 2012, and the highest number of patients visited EDs in 2011 (Table).
ED examinations were followed by GW hospitalizations for 17,524 patients, which represented 42.6% of the total number of ED visits. The numbers of GW hospitalizations were 2,522, 2,265, 3,572, 3,036, 3,852, and 2,277 for 2007, 2008, 2009, 2010, 2011, and 2012, respectively. In 2011, the largest number of patients presented at the EDs and were hospitalized on GWs. The difference in the annual patient GW hospitalization rate was statistically significant (OR=0.96, 95% CI=[0.94-0.97]) (Table). The GW hospitalization rates were 48.4% for the 3-6 years age group, 36.9% for the 7-12 years age group, and 31.5% for the 13-18 years age group; therefore, the hospitalization rates declined as the patients' ages increased (7-12 years age group: OR=0.62, 95% CI=[0.60-0.65]; 13-18 years age group: OR=0.49, 95% CI=[0.46-0.53]) (Table). The GW hospitalization rates were 40.9% for the male patients and 45.7% for the female patients; therefore, the GW hospitalization rate was higher for the female patients (OR=1.21, 95% CI=[1.16-1.26]) (Table).
ED examinations were followed by ICU hospitalizations for 335 patients, which represented 0.8% of the total number of ED visits and 1.9% of the GW hospitalized patients. Thirty-four, 43, 117, 57, 52, and 32 patients were hospitalized in ICUs in 2007, 2008, 2009, 2010, 2011, and 2012, respectively. The number of patients who were hospitalized in ICUs was larger in 2009 than in 2011, although, in 2011, that of patients who visited EDs was highest, and the higher rate of ICU hospitalization was statistically significant (OR=2.45, 95% CI=[1.66-3.59]) (Table).
The 13-18 years age group showed a significantly higher ICU hospitalization rate compared to the other age groups (1.5%; OR=1.68, 95% CI=[1.25-2.26]). There was no difference between the sexes in the ICU hospitalization rate (Table).
Two patient deaths were reported in 2012, and these comprised a 3-year-old girl with asthma who had a tracheostomy and secondary pulmonary arterial hypertension, and a 13-year-old boy who did not have any comorbidities. Both were dead on arrival at the EDs.
The highest proportion of the patients (37.6%) visited the EDs from 18:00 to 00:00, 22.3% of the patients visited the EDs from 12:00 to 18:00, 21.7% of the patients visited the EDs from 00:00 to 06:00, and 18.4% of the patients visited the EDs from 06:00 to 12:00.
On average, 571 pediatric and adolescent asthmatic patients presented at the EDs each month, and the monthly distribution was not uniform during the year (P=0.001) (Fig. 1). The average numbers of patients who presented at the EDs from September to November each year were higher than the average numbers of patients who presented at the EDs during the rest of the year, and the numbers of patients who presented at the EDs each year were at their highest during September or October, when there were 2-fold increases in the numbers compared to the annual averages. The numbers of patients who presented at the EDs each year were at their lowest from June to August, and these numbers were 45% lower than the annual averages. The numbers of patients who presented at the EDs each year increased slightly in spring, that is, from March to May.
The distribution of the ED visits was independent of age (χ2=57.82, P=0.001) (Fig. 2). The monthly distribution of the ED visits was independent of the region (χ2=468.30, P=0.001) (Fig. 3). Regardless of age and region, the numbers of patients who presented at the EDs each year from September to November were larger compared to the rest of the year (Figs. 2 and 3).
The monthly numbers of GW hospitalizations following ED examinations peaked during fall of each year, which was consistent with the numbers of patients who presented at the EDs at these times (Fig. 4). The monthly numbers of ICU hospitalizations following ED examinations were at their highest in September 2007 and September 2011, and, in particular, 2009 had the highest number of ICU hospitalizations following ED examinations from October until December. Increases in the numbers of ICU-hospitalized patients were apparent in December 2007, December 2008, and December 2010 (Fig. 5).
To manage the chronic nature of asthma, preventative therapies are essential to prevent asthma exacerbations. A recent review that summarized studies of asthma exacerbations reported that asthma symptoms tend to occur at the beginning of fall in children and in winter in adults, and that worsening asthma symptoms are more frequently observed in male patients before puberty and after puberty in female patients.10 Hence, adults experience asthma exacerbations more frequently and seriously in women, and they lead to longer periods of hospitalization for women compared to men.
Our findings showed that the ratio of male-to-female asthmatic patients was 1:0.5. Our findings also showed that a larger number of male patients who were in the 13-18 years age group visited EDs, and that the male-to-female ratio for ED visits by this age group was 1:0.5 (data not shown); thus, these results differ from other studies. In addition, a higher rate of GW hospitalizations was observed for the female patients in this study. Reviews of the international literature have shown that the sex ratio of asthma exacerbation tends to shift at the age of 13 years or in the 11-17 years age group.1112 Furthermore, among adolescent patients who were in the 7th to 12th grades of school in the USA, female patients exhibited more serious symptoms.13
Although differences between the sexes in asthma prevalence and exacerbation are not fully understood, it is thought that girls have larger central airways than boys, then, after the growth spurt the males' airways become larger than the females' airways,14 which leads to a relatively higher risk of asthma for females.15 More females than males experience asthma exacerbations after the age of 15 years,34 which could be the consequence of a hormonal effect.16
In 2010, a nationwide cross-sectional survey of Korean children revealed that asthma prevalence rates were 12.4% for boys and 8.0% for girls aged 6-7 years and 8.9% for boys and 7.7% for girls aged 13-14 years.17 This study also showed higher prevalence rates among male Korean children and adolescents. Data from the National Statistical Office18 show that the male-to-female ratios are 106:100 or 112:100 for people who are younger than 18 years of age.
In the present study, the largest number of patients who visited the EDs was in the 3-6 years age group, and this group had the highest rate of GW hospitalization following ED visits (48.4%). Younger children tend to present at EDs with asthma symptoms more often, because very young children tend to have smaller airways compared to older children, and rapid postnatal growth leads to changes in the morphology and reactivity of their airways, which results in frequent ED visits for lower respiratory tract illnesses.17 Furthermore, hospitalization criteria become more stringent as patients' ages increase.3 In addition, young children have the higher rates of ED visits and hospitalizations because they can readily transit to life-threatening statuses as a consequence of the respiratory distress caused by pulmonary inflammation.19
In our study, the rate of ICU hospitalization after visits to the ED was highest in the 13-18 years age group. In the USA, the prevalence of ICU hospitalization after visits to the ED was highest among children aged between 11 and 17 years, and asthma maintenance treatment was often not successful, which led to high mortality levels in this age group.12 It was thought that this was caused by adolescent patients experiencing difficulties in maintaining asthma control, because they have to recognize and treat their asthma exacerbations themselves.12
Viral infection is a major factor that is involved in asthma exacerbations among children and adults, and the correlation between asthma exacerbations and viral respiratory inflammation is stronger in children (85%) than in adults (55%).20 The type of respiratory virus that is associated with asthma attacks varies depending on patient age. Many studies have reported that rhinoviruses (RVs) and the influenza virus (IFV) are major causes of asthma attacks among children and adults, and that the respiratory syncytial virus (RSV) and parainfluenza virus (PIV) are dominant causes of asthma attacks among very young children.21 Findings from a previous study have shown a strong positive correlation between the seasonal distribution of respiratory viral infections and hospitalizations as a consequence of asthma, and that this is more frequently observed in children.22 Johnson et al.22 reported that RV infections were observed most frequently among children who were aged from 9 to 11 years and who experienced asthma exacerbations, and that RV infections were particularly frequent during spring and fall. They also reported that the pattern of RV detection was consistent with the increased hospitalization rates for asthma during spring and fall.
In the temperate zone of the northern hemisphere, the RV detection rate is at its highest in September, and the lower rates of detection occur in April and May; however, RVs are detected throughout the year.23 Although the RV is considered a major infectious cause of childhood asthma and it is associated with dramatic increases in asthma attacks during fall when school starts in a number of nations,23 the Korean trend relating to RV infections does not show a uniform pattern, which is unlike international trends. Reports from the Korea Centers for Disease Control and Prevention2425 indicate that RV infections increase from March to April and from September to October, but RV detections in fall are not that high. RV infections occur throughout the year and the seasonal prevalence of RV is not uniform. Furthermore, the detection rates vary every year, and they even showed peaks during the summers of 2007 and 2008. In addition, the findings from respiratory viral examinations of patients who were aged from 2 to 13 years and were hospitalized because of asthma exacerbations, revealed that RSV had the highest detection rate (31%), followed by IFV (17.2%) and RV (12%).26 Studies of asthma exacerbations21 indicate that RV is detected more often in asthmatic and healthy individuals in spring than in fall, and that the respiratory virus activity levels can vary depending on the season, year, and the contributing factors because the results can vary depending on the patient group, the method of sample collection, and the examination methods.
In this study, larger numbers of asthma patients visited the EDs in more recent years compared to 6 years ago; however, the increase was not uniform, and the numbers of patients visiting the EDs were largest during fall (Fig. 1). In Korea, an H1N1 virus pandemic occurred between October and December in 2009,27 and the nationwide outbreaks of mycoplasma infections ococcurred during fall in 2007 and 2011.28 These outbreaks may have been the consequences of the impacts of the respiratory infections that were prevalent during fall in 2007, 2009, and 2011 (Fig. 1).
A retrospective study of a cohort of children who were younger than 15 years that was undertaken over 20 years in the USA showed that during the IFV seasons, asthma patients' ED visits increased compared to the periods before the IFV seasons.29 During the H1N1 virus pandemic that occurred from September to October 2009, asthmatic patients who were infected with the H1N1 virus exhibited more serious respiratory symptoms than those who were infected with other viruses or were not infected with other viruses.30 Based on this finding, we theorized that the peak in asthma exacerbations that we observed from October to December 2009 was a consequence of the impact of H1N1 virus infections. In this study, ICU hospitalizations as a consequence of asthma in October 2009 showed an approximately 7-fold increase above the monthly average, which was consistent with the number of children who had H1N1 virus infections, were younger than 18 years of age, and were hospitalized in the ICUs in October 2009.31
Since the mechanism underlying the exacerbations of asthma symptoms involves multiple factors in addition to respiratory infection, it is difficult to explain the mechanism based on a single factor. Seasonal climate changes are involved in asthma exacerbations during fall; hence, asthma symptoms increase when the temperature is low or when it declines dramatically.3233 A study in West India, where the dry and rainy seasons are distinct, concluded that asthma was worse in the rainy season, and this was related to temperature and pressure changes.8 Another study reported that visits at the ED increased at night when the atmospheric pressure, temperature, or humidity were high and then suddenly decreased, and that asthma exacerbations often occurred during spring and fall when unstable atmospheric changes are frequent.9
A 20-year study undertaken in Finland evaluated asthmatic patients who were younger than 15 years reported that the highest hospitalization rates were in the fall and in May.6 The same authors suggested that the high hospitalization rates in May might be associated with the presence of high concentrations of birch pollen. However, these findings are controversial, because the findings from another study did not determine a correlation between asthma exacerbations and the birch pollen in adult patients.34 They also pointed out that the spread of PIV, which often occurs during early spring in Finland, might be associated with the high hospitalization rates in May. Although the hospitalization rates were not as high those that occurred during fall, that study also showed increases in ED visits and hospitalizations during spring, suggesting that the impact of PIV often peaks in spring.34
The seasonal release of pollen is a factor that is involved in asthma exacerbations, and it shows regional variations. The findings from a recent domestic study have shown that each season is associated with distinctive peaks of different types of pollen,35 but it is difficult to conclude that pollen is associated with the exacerbations of asthma symptoms that occur during fall. The findings of a recent study have shown that the seasonal peak in hospitalizations for asthma has a higher correlation with respiratory viruses and that it is not associated with the pollen count.22 Viral infections themselves can induce and exacerbate bronchial asthma, and they may exacerbate asthma by interacting with other factors that are known to exacerbate asthma and increase allergen levels.36
Previous studies showed that there are significant correlations between air pollution and asthma exacerbations in children but not in adults.37 It is possible that the results differed because of the characteristics of the study participants, the timing and duration of the study, the definition of an acute exacerbation, and variations in the analytical methods used.38
This study has some limitations. First, since this study focused on patients who were hospitalized through EDs or were discharged after ED treatment, it did not include those who were treated in outpatient clinics or those who were hospitalized through outpatient clinics; hence, it did not reflect the total number of hospitalized asthmatic patients. Second, no data were available that determined whether all of the patients who presented at the EDs had experienced asthma exacerbations, and detailed clinical reports and examination results were lacking for these patients.
This study analyzed large data sets that comprised data that were collected from children and adolescents who visited EDs throughout Korea over a 6-year period as opposed to a 1-year period; thus, the data are extremely representative of the nation. In addition, this study incorporated the time periods during which the H1N1 viral and mycoplasma infections peaked, which enabled comparisons of their potential impacts. By comparing the GW and ICU hospitalization rates, we were able to investigate the impacts of age and sex on the severity of asthma.
Therefore, if we can understand risk factors underlying GW and ICU hospitalizations for asthma exacerbations, we can establish efficient strategies for their prevention and treatment. Furthermore, the patterns of asthma can help identify factors that exacerbate asthma and assist in monitoring those patients who are at high risk during the season when asthma exacerbations are predicted.
Figures and Tables
Fig. 1
Monthly asthma-related emergency department visits at ages between 3 and 18 years, by year from 2007 to 2012.

Fig. 2
Monthly asthma-related emergency department visits at ages between 3 and 18 years, by age from 2007 to 2012.

Fig. 3
Monthly asthma-related emergency department visits at ages between 3 and 18 years, by region from 2007 to 2012.

Fig. 4
Monthly general ward hospitalizations as a result of the emergency department examinations for asthma at ages between 3 and 18 years, from 2007 to 2012.
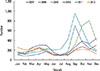
Fig. 5
Monthly intensive care unit hospitalizations as a result of the emergency department examinations for asthma at ages between 3 and 18 years, from 2007 to 2012.

Table
Trends in emergency department visits, general ward hospitalizations, and intensive care unit hospitalizations for childhood asthma by year, age, and sex, from 2007 until 2012

References
1. Busse WW, Lemanske RF Jr. Asthma. N Engl J Med. 2001; 344:350–362.
2. Kimes D, Ullah A, Levine E, Nelson R, Timmins S, Weiss S, et al. Relationships between pediatric asthma and socioeconomic/urban variables in Baltimore, Maryland. Health Place. 2004; 10:141–152.
3. Kimbell-Dunn M, Pearce N, Beasley R. Seasonal variation in asthma hospitalizations and death rates in New Zealand. Respirology. 2000; 5:241–246.
4. Fleming DM, Cross KW, Sunderland R, Ross AM. Comparison of the seasonal patterns of asthma identified in general practitioner episodes, hospital admissions, and deaths. Thorax. 2000; 55:662–665.
5. Kimes D, Levine E, Timmins S, Weiss SR, Bollinger ME, Blaisdell C. Temporal dynamics of emergency department and hospital admissions of pediatric asthmatics. Environ Res. 2004; 94:7–17.
6. Harju T, Keistinen T, Tuuponen T, Kivelä SL. Seasonal variation in childhood asthma hospitalisations in Finland, 1972-1992. Eur J Pediatr. 1997; 156:436–439.
7. Masoli M, Fabian D, Holt S, Beasley R. Global Initiative for Asthma (GINA) Program. The global burden of asthma: executive summary of the GINA Dissemination Committee report. Allergy. 2004; 59:469–478.
8. Ivey MA, Simeon DT, Monteil MA. Climatic variables are associated with seasonal acute asthma admissions to accident and emergency room facilities in Trinidad, West Indies. Clin Exp Allergy. 2003; 33:1526–1530.
9. Hashimoto M, Fukuda T, Shimizu T, Watanabe S, Watanuki S, Eto Y, et al. Influence of climate factors on emergency visits for childhood asthma attack. Pediatr Int. 2004; 46:48–52.
10. Sears MR. Epidemiology of asthma exacerbations. J Allergy Clin Immunol. 2008; 122:662–668.
11. Johnston NW, Sears MR. Asthma exacerbations. 1: epidemiology. Thorax. 2006; 61:722–728.
12. Akinbami LJ, Moorman JE, Garbe PL, Sondik EJ. Status of childhood asthma in the United States, 1980-2007. Pediatrics. 2009; 123:Suppl 3. S131–S145.
13. Fagan JK, Scheff PA, Hryhorczuk D, Ramakrishnan V, Ross M, Persky V. Prevalence of asthma and other allergic diseases in an adolescent population: association with gender and race. Ann Allergy Asthma Immunol. 2001; 86:177–184.
14. Brooks LJ, Byard PJ, Helms RC, Fouke JM, Strohl KP. Relationship between lung volume and tracheal area as assessed by acoustic reflection. J Appl Physiol (1985). 1988; 64:1050–1054.
15. Chen Y, Stewart P, Johansen H, McRae L, Taylor G. Sex difference in hospitalization due to asthma in relation to age. J Clin Epidemiol. 2003; 56:180–187.
16. Troisi RJ, Speizer FE, Willett WC, Trichopoulos D, Rosner B. Menopause, postmenopausal estrogen preparations, and the risk of adult-onset asthma. A prospective cohort study. Am J Respir Crit Care Med. 1995; 152:1183–1188.
17. Ahn K, Kim J, Kwon HJ, Chae Y, Hahm MI, Lee KJ, et al. The prevalence of symptoms of asthma, allergic rhinoconjunctivitis, and eczema in Korean children: nationwide cross-sectional survey using complex sampling design. J Korean Med Assoc. 2011; 54:769–778.
18. Statistics Korea. Sex ratio of age groups [Internet]. Daejeon: Statistics Korea;2015. cited 2015 Aug 1. Available from: http://www.index.go.kr/potal/stts/idxMain/selectPoSttsIdxSearch.do?idx_cd=2917&clas_div=&idx_sys_cd=544&idx_clas_cd=1.
19. Taussig LM, Wright AL, Holberg CJ, Halonen M, Morgan WJ, Martinez FD. Tucson children's respiratory study: 1980 to present. J Allergy Clin Immunol. 2003; 111:661–675.
20. Tan WC. Viruses in asthma exacerbations. Curr Opin Pulm Med. 2005; 11:21–26.
21. Khetsuriani N, Kazerouni NN, Erdman DD, Lu X, Redd SC, Anderson LJ, et al. Prevalence of viral respiratory tract infections in children with asthma. J Allergy Clin Immunol. 2007; 119:314–321.
22. Johnston SL, Pattemore PK, Sanderson G, Smith S, Campbell MJ, Josephs LK, et al. The relationship between upper respiratory infections and hospital admissions for asthma: a time-trend analysis. Am J Respir Crit Care Med. 1996; 154:654–660.
23. Miller EK, Williams JV. Rhinoviruses. In : Kliegman RM, Stanton BF, St Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. 19th ed. Philadelphia (PA): Elsevier/Saunders;2011. p. 1133–1134.
24. Korean Centers for Disease Control and Prevention. The prevalence of the respiratory viruses in the patients with acute respiratory infections, 2012 [Internet]. Cheongwon: Korean Centers for Disease Control and Prevention;2013. cited 2015 Aug 1. Available from: http://www.cdc.go.kr/CDC/info/CdcKrInfo0301.jsp?menuIds=HOME001-MNU1132-MNU1138-MNU0037-MNU1380&fid=31&q_type=title&q_value=%EB%B0%94%EC%9D%B4%EB%9F%AC%EC%8A%A4&cid=21323&pageNum=1.
25. Korean Centers for Disease Control and Prevention. Weakly occurrence of acute respiratory tract infection with 8 respiratory viruses in Korea patients [Internet]. Cheongwon: Korean Centers for Disease Control and Prevention;2013. cited 2015 Aug 1. Available from: http://www.cdc.go.kr/CDC/info/CdcKrInfo0502.jsp?menuIds=HOME001-MNU1175-MNU0048-MNU0050&fid=477&q_type=&q_value=&cid=19952&pageNum=1.
26. Roh EJ, Jin YM, Chung EH, Rheem I, Kim JK. The prevalence of respiratory viral infection in exacerbation of asthma in hospitalized children. Korean J Asthma Allergy Clin Immunol. 2007; 27:241–247.
27. Kang SH, Choi HM, Lee EH. Positive rates of 2009 novel influenza A (H1N1) was high in school-aged individuals: significance in pandemic control. J Korean Med Sci. 2012; 27:332–334.
28. Kim EK, Youn YS, Rhim JW, Shin MS, Kang JH, Lee KY. Epidemiological comparison of three Mycoplasma pneumoniae pneumonia epidemics in a single hospital over 10 years. Korean J Pediatr. 2015; 58:172–177.
29. Neuzil KM, Wright PF, Mitchel EF Jr, Griffin MR. The burden of influenza illness in children with asthma and other chronic medical conditions. J Pediatr. 2000; 137:856–864.
30. Kloepfer KM, Olenec JP, Lee WM, Liu G, Vrtis RF, Roberg KA, et al. Increased H1N1 infection rate in children with asthma. Am J Respir Crit Care Med. 2012; 185:1275–1279.
31. Shin SY, Kim JH, Kim HS, Kang YA, Lee HG, Kim JS, et al. Clinical characteristics of Korean pediatric patients critically ill with influenza A (H1N1) virus. Pediatr Pulmonol. 2010; 45:1014–1020.
32. Celenza A, Fothergill J, Kupek E, Shaw RJ. Thunderstorm associated asthma: a detailed analysis of environmental factors. BMJ. 1996; 312:604–607.
33. Larsson K, Ohlsén P, Larsson L, Malmberg P, Rydström PO, Ulriksen H. High prevalence of asthma in cross country skiers. BMJ. 1993; 307:1326–1329.
34. Rossi OV, Kinnula VL, Tienari J, Huhti E. Association of severe asthma attacks with weather, pollen, and air pollutants. Thorax. 1993; 48:244–248.
35. Oh JW, Lee HB, Kang IJ, Kim SW, Park KS, Kook MH, et al. The revised edition of Korean calendar for allergenic pollens. Allergy Asthma Immunol Res. 2012; 4:5–11.
36. Green RM, Custovic A, Sanderson G, Hunter J, Johnston SL, Woodcock A. Synergism between allergens and viruses and risk of hospital admission with asthma: case-control study. BMJ. 2002; 324:763.
37. Sun HL, Chou MC, Lue KH. The relationship of air pollution to ED visits for asthma differ between children and adults. Am J Emerg Med. 2006; 24:709–713.
38. Kim SH, Son JY, Lee JT, Kim TB, Park HW, Lee JH, et al. Effect of air pollution on acute exacerbation of adult asthma in Seoul, Korea: a case-crossover study. Korean J Med. 2010; 78:450–456.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download