Abstract
Purpose
Chronic urticaria (CU) has a substantial impact on the quality of life. Little clinical data on the prognosis of CU has been reported. This study aimed to investigate the control status and remission rate of CU and to explore potential predictors of good responses to the treatment during a 6-month treatment period.
Methods
A total of 75 patients with chronic spontaneous urticaria (CSU) were enrolled from 3 university hospitals in Korea. Urticaria control state was classified into 2 groups: group I (remission and well-controlled) and group II (partly and uncontrolled). CU-specific quality of life (CU-QoL) and the urticaria activity score (UAS) were measured before and after the treatment. Autologous serum skin test (ASST), and anti-nuclear and anti-thyroid antibodies were measured at the enrollment into the study. Aspirin intolerance was confirmed by an oral provocation test.
Results
Of 59 patients completing the study, 21 (35.6%) arrived at well-controlled status and only 2 (3.4%) achieved remission, whereas 26 (44.1%) remained at partly controlled status and 10 (16.9%) were at uncontrolled status. Mean changes in CU-QoL (36.5±2.7 vs 20.6±4.3, P=0.017) and UAS (-7.9±0.8 vs -3.0±1.0, P=0.001) were significantly different between groups I and II. The presence of serum autoantibodies and aspirin intolerance had no influence on the control of urticaria in this study. However, ASST positivity was identified as a significant predictor of CU control in multivariate analysis (OR=6.106, P=0.017).
Conclusions
The proportion of CSU patients that achieved remission or a well-controlled state was 39% for the 6 months of stepwise treatment. Longer observations are necessary to assess the exact prognosis of CSU. ASST results may be a useful parameter for predicting a better response to treatment and both UAS and CU-QoL are helpful to monitor therapeutic response.
Chronic urticaria (CU) is a common skin disorder defined by recurrent wheals and itching for at least 6 weeks. Previous studies have revealed a point prevalence of 0.1%-1.0% in the general population.12 CU has major detrimental effects on the quality of life, with frequent sleep deprivation and psychiatric comorbidity.3 It also has a large impact on society in terms of direct and indirect health care costs, as well as reduced performance at work and in personal life.3
Regarding the pharmacological treatment of CU, recent guidelines recommended a stepwise approach;45 however, previous results on the prognosis of CU are variable. CU has generally been recognized as a non-life-threatening and transiently symptomatic disease, with an average duration of 2 to 5 years.6 Although few studies have evaluated the duration of CU, in 70% of patients, it persists for 1 year.78 In fact, more than 11% of CU patients have urticaria symptoms for more than 5 years.7 However, it is likely to occur longer in more severe cases.9 Factors predicting therapeutic response and disease severity are limited. Genetic factors related to mast cell activation and the overproduction of histamine and leukotriene have been suggested to contribute to disease development and clinical heterogeneity.10 Angioedema, severe CU, and anti-thyroid antibodies have recently been identified as being associated with longer disease duration.911 In addition, since the correlation between a positive autologous serum skin test (ASST) and the presence of anti-FcɛRIα and anti-IgE antibodies was reported,12 investigators have attempted to demonstrate the utility of ASST as a biomarker for identifying a distinct subgroup of CU patients or for predicting treatment responses. However, to date, the association between ASST positivity and clinical course of CU has been inconclusive.513 This study was designed to evaluate the prognosis of a 6-month stepwise treatment and to determine predictors for control status in patients with CU.
We performed a prospective observational study on 75 CSU patients (24 males and 51 females, age 19-69 years, mean age 40.5 years) who were followed in the outpatient Allergy Clinic of 3 university hospitals, including Ajou University Hospital, Severance Hospital, and Wonju Severance Christian Hospital in South Korea from November 2011 to March 2013. Inclusion criteria were patients aged ≥19 years and having almost daily urticaria symptoms, such as wheals and itching, for at least 6 weeks. Patients with other chronic skin diseases and those with clinical evidence of urticarial vasculitis or inducible (physical stimuli or cholinergic or exercise) urticaria were excluded. Each patient submitted a written informed consent form at the time of enrollment, and the Institutional Review Board approved the study. A stepwise treatment according to the recent guidelines4 was applied to all subjects. Our study protocol, including how to assess urticaria control and to apply stepwise treatment, was reviewed and accepted by all investigators before starting this study. Investigators determined the first treatment step for each subject based on their medication history and current urticaria severity. Step I and II treatments correspond to up to 2 and 4 tablets of non-sedating antihistamines, respectively. The addition of leukotriene receptor antagonist to 4 antihistamine tablets was the step III treatment. Immunosuppressive agents, including cyclosporine and oral corticosteroids, were regarded as the step IV treatment.
CU disease activity was assessed using the urticaria activity score (UAS), which scores wheals according to quantity, distribution range, mean diameter, and duration, in conjunction with pruritus according to the intensity within the last week for outpatient clinic visits, yielding a total score of 0-15.14
Urticaria control state was classified into 4 categories according to our previous report: remission, well-controlled, partly controlled, and uncontrolled.15 Remission was defined as the absence of urticaria symptoms for at least 4 weeks without any medication. Patients who had no wheals or itching when taking medication, but whose symptoms returned when they discontinued their medication, were deemed to have well-controlled CU. Patients whose urticaria symptoms were reduced from the previous visit, but not completely controlled, were classified as partly controlled CU. Patients whose disease could not be controlled by medication were deemed to have uncontrolled CU.
The EAACI/GA2LEN/EDF/WAO guideline for the management of urticaria recommends re-evaluation of the necessity for continued or alternative treatment every 3-6 months because of fluctuating disease activity of CU.16 Therefore, we assessed urticaria control state and UAS at the initial visit and in the first, third, and sixth months after treatment, in total 4 times during the study period. However, patients were able to see investigators, whenever they wanted to discuss changes in their urticaria symptoms.
Antihistamines were withdrawn at least 5 days before blood sampling. An intradermal autologous serum skin test (ASST) was performed according to the method described in the EAACI/GA2LEN task force consensus report.17 A positive result was defined as a serum-induced wheal after 30 minutes with a diameter of at least 1.5 mm greater than that induced by saline.
Patients with aspirin intolerant chronic urticaria (AICU) was defined as those who had a definite history of urticaria/angioedema development after the ingestion of aspirin and/or non-steroidal anti-inflammatory drugs (NSAIDs) and those who showed positive respones to the oral aspirin challenge test, as previously described.18 The appearance of urticaria within 4 hours without any change in FEV1 was considered a positive result.
Atopy was defined as a positive skin test response to at least 1 common inhalant allergen, including pollens, animal dander, mold, and house dust mites (Allergopharma, Reinbek, Germany).
Total IgE levels were measured using the ImmunoCAP system (Thermo-Fisher, Uppsala, Sweden) according to the manufacturer's instructions. ANA was detected using HEp-2 cells and an indirect fluorescent antibody technique (Fluoro HEPANA test; Medical & Biological Laboratories, Nagoya, Japan). Anti-thyroglobulin and thyroid microsomal antibodies were detected by radioimmunoassay (BRAHMS Aktiengesellschaft, Hennigsdorf, Germany). Serum CRP (IBL-America, MN, USA) concentrations were measured by ELISA using commercially available reagents.
Data for continuous variables are shown as means±standard deviation (SD). Prevalence rates are shown as percentages. We used the full analysis set (FAS), which includes all patients who received at least 1 dose of the assigned treatment, to describe the study populations included in the urticaria control analysis. Student's t test and ANOVA were used for between-group comparisons of continuous variables. Categorical variables were compared using Pearson's χ2 test. Mann-Whitney U and Fisher's exact tests were applied for continuous and categorical variables in comparison between patients with ASST positivity and negativity, respectively. Logistic regression was used to examine the effects of various factors on remission or well-controlled CU. The generalized estimating equation was used for examining the impact of the treatment step on urticaria control over the study period. The UAS and CU-QoL of the patients over the study period were examined by repeated-measures ANOVA according to the ASST results. We used the generalized estimating equation to evaluate the influence of baseline ASST results on urticaria control considering treatment step and duration as covariates. A P value of <0.05 was considered to indicate significance. All statistical analyses were performed using SPSS for Windows version 19.0 (SPSS, Chicago, IL, USA).
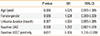
Among a total of 80 patients, 59 patients completed this 6-month prospective observational study. Of the 21 patients who were withdrawn from the study due to follow-up loss (n=14) and withdrawal of consent (n=2), with the exception of those who did not take medication during the study period (n=5), 16 were included in the statistical analysis. The baseline characteristics of 75 study patients whose urticaria control was evaluated at least once in the study period are shown in Table 1. The mean age of the patients was 40.5 years, 51 patients (68%) were female, and 21.9% of the 80 patients had aspirin intolerance. The mean duration of their urticaria symptoms was 37.9 months, and half of the patients had uncontrolled urticaria at the time of enrollment (Table 1). Of the 63 patients whose IgG autoantibodies, including anti-thyroid (thyroglobulin and microsomal) and anti-nuclear antibodies, were measured, 21 (33.3%) exhibited a positive result indicating the presence of any of these 3 autoantibodies. There was no significant difference in urticaria duration (median, minimum-maximum) before the enrollment according to the presence of angioedema (13, 2-360 vs 12, 2-120 months, P=0.445), anti-thyroid antibodies (13, 2-240 vs 12, 2-360 months, P=0.840), and a positive ASST (6, 2-108 vs 13, 2-360 months, P=0.122). In 25.4% of patients exhibiting positive ASST results, serum CRP (0.12±0.33 vs 0.60±0.99 mg/mL, P=0.037) was significantly lower, while peripheral basophil levels (0.82±1.24 vs 0.28±0.57%, P=0.020) were significantly higher than in those with negative ASST results (Table 1). In addition, the frequency of serum autoantibodies tended to be increased in patients with positive ASST results (9/17, 52.9%) than in those with negative ASST results (10/38, 26.3%), although statistical significance (P=0.071) was not reached.
After 6 months of prospective observation, 2 (3.4%) and 21 (35.6%) of the 59 patients were determined to have their urticaria in remission and well-controlled states, respectively (Fig. 1). On the contrary, 16.9% of the patients remained at uncontrolled state even with the same stepwise treatment. The mean time to first well-controlled month was 4.4 months. There were no significant differences in demographics and clinical parameters among the 4 CU control statuses (Table 2). Two patients who achieved remission within 6 months had taken antihistamine monotherapy, while 60% of patients with uncontrolled CU had maintained at least step III treatment, including leukotriene antagonists and/or cyclosporine. In addition, 43.2% of the patients continuously advanced a treatment step during the study period. However, 29.7% of the patients maintained the treatment step at the beginning of the study, and 27.0% were able to step down over 6 months.
The initial treatment steps of the patients were not different between groups I and II (Fig. 2) Approximately half of patients in either group did not have any maintenance treatment for CU at the enrollment, while 17.4% of group I and 16.7% of group II had been taking oral corticosteroids for more than 2 weeks. These results may reflect the lack of awareness about that CU is a chronic disease whose aim of treatment is a complete symptom control. None of the patients were taking cyclosporine at the time of enrollment.
Urticaria control state was classified into 2 groups: group I (remission and well-controlled) and group II (partly and uncontrolled). The baseline positive rate of ASST was significantly higher in group I compared to group II (41.2% vs 11.8%, P=0.028). Other parameters, including age, urticaria duration, gender, atopy rate, aspirin intolerance, baseline UAS, and CUQoL were not different between the 2 groups (Table 2). The frequency (2.1±3.1 vs 0.7±1.8, P=0.034) and total dose (21.7±14.2 vs 5.1±43.1 mg of prednisolone equivalent dose, P=0.045) of oral corticosteroid use for controlling urticaria exacerbation was significantly higher in group II compared to group I. However, the overall changes in treatment steps, as well as dosages of antihistamines, leukotriene antagonist, and cyclosporine, were not significantly different between the 2 groups. The generalized estimating equation revealed that changes in the proportion of patients having the step IV treatment over the study period had no significant influence on the determination of the 2 groups (Fig. 2, P=0.155).
Table 3 summarizes the independent predictors of urticaria control in the study subjects. A significant association between ASST positivity and a better prognosis of CU was reproduced by a multivariate analysis after the adjustment for age, gender, baseline UAS and urticaria duration (Table 3). Changes from baseline in CU-QoL after the 6-month treatment were significantly greater in group I compared to group II (29.9±17.3 vs 14.1±23.0, P=0.007). The UAS changed significantly in group I from the baseline to the end of the study than in group II (-7.9±3.8 vs -3.0±5.8, P=0.001, Fig. 3).
In addition, the mean scores of the UAS and CU-QoL for the overall study period differed between patients with positive and negative ASST results (Fig. 4). The mean UAS of the patients decreased steeply after the first month of treatment and was maintained over time in both the positive and negative ASST groups. In patients with positive ASST results, the decrease in the mean UAS seemed to be remarkable, but was not significantly different from those with negative ASST results. In contrast, the mean CU-QoL score in patients with positive ASST results was significantly higher than in those with negative ASST results at the first month of treatment (80.0±20.3 vs 70.9±24.7, P=0.024).
Fig. 5 shows the proportion of patients achieving well-controlled CU according to both their treatment steps and baseline ASST results over the study period. Changes in treatment steps are not remarkable between ASST positive and ASST negative patients with positive and negative ASST results. Five of the 39 patients with negative ASST results received the step IV treatment in the 6th month. Among them, 1 (20%) patient achieved well-controlled CU. Two (50%) of the 4 ASST-positive patients receiving the step IV treatment at the last visit had well-controlled status. The generalized estimating equation demonstrated that a positive ASST (OR=2.648, 95% CI 1.256-5.583, P=0.011) was a significant determinant of well-controlled CU at the end of this study even after adjusting for the treatment step (OR=0.891, 95% CI 0.709-1.121, P=0.325) and treatment period (OR=1.232, 95% CI 1.086-1.397, P=0.001) as covariates.
In this study, we investigated remission and urticaria control status classified as well, partly, and uncontrolled, as well as factors related to the prognosis of CU using the standard treatment of 6 months. The CU remission rate within 6 months of stepwise treatment based on recent guidelines4 was 3.4% in the 59 patients. Regardless of their urticaria duration before enrollment in this study, 39% of the patients achieved at least well-controlled CU after 6 months. However, 61% of the patients suffered from wheals and pruritus, without a significant difference in treatment pattern between the 2 groups. Considering that 43.2% of the subjects continuously advanced in treatment steps during the study period, while 27.0% of patients were able to tolerate a step-down of treatment, 6 months of observation is insufficient to determine the exact prognosis of CU. The natural course of CU is unpredictable, and reported remission rates vary. In general, CU remission has been achieved in 11.5% to 47.4% of patients at 1 year.891119 However, to date, most studies investigating the prognosis of CU were retrospective,7920 and they differ in terms of onset age, disease duration, and previous treatment step at the enrollment, as well as ethnicity.9
This study suggests a potential use of ASST to predict the control status of CU over a 6-month period of stepwise treatment. The patients with negative ASST results at enrollment showed more severe CU in terms of higher CRP levels and more prominent basopenia, which have previously been demonstrated to be associated with urticaria severity.212223 Additionally, we previously demonstrated a significant association of negative ASST results with a higher prevalence of metabolic syndrome, which is a chronic, low-grade systemic inflammatory state that coexists in severe CU patients.15 However, these results that patients with negative ASST results had more severe inflammatory conditions at the beginning of the study suggest a possible limitation in the assessment of the urticaria control under the same standard stepwise treatment for both ASST positive and negative groups. In addition, considering that some patients who had a longer disease duration, without statistical significance, were included in the ASST negative-group, we could not completely exclude a potential bias in subjects selection. However, multivariate regression analysis revealed that a positive ASST was a significant independent predictor of urticaria control over 6 months of stepwise treatment, whereas no significant difference was noted in urticaria duration and disease activity.
The UAS was demonstrated to be a good parameter for predicting severe CU refractory to antihistamines in our previous studies.1524 However, the baseline UAS in this study had no impact on urticaria control, although changes in the UAS were significantly different between groups I and II. The frequency and dosage of rescue steroid use during the study in CU patients were significantly different according to their control status. These results indicate that both UAS and CU-QoL can be useful parameters for monitoring the treatment response or control status in patients with CU.
Angioedema, severe CU, and autoimmunity resulting in positive ASST and anti-thyroid antibodies or hypertension have recently been identified as factors associated with a longer disease duration.911 However, a recent systematic review revealed no evidence to support the association between ASST positivity and a longer duration or disease activity in CU patients.13 Even though ASST is generally used and well established, variance in the positivity rate and clinical association of ASST has been issued. The frequency of ASST positivity in CSU patients in this study (25.4%) is comparable with those of previous studies.11121317252627 There are considerable heterogeneous data on the prognostic role of ASST reactivity.13 Previous studies mainly investigated the association between ASST positivity and urticaria duration/disease severity. Some studies showed increased disease activity or longer duration in ASST positive patients,1128293031 whereas no significant differences in severity,26273031 disease duration,26272930 and quality of life scores31 between the ASST-positive and ASST-negative patients were noted in others. However, there has been no attempt to study on whether ASST reactivity can predict urticaria control status and therapeutic response in CSU patients. Staubach et al.31 reported that ASST-positive CU patients require more antihistamines; however, their results were based on retrospective observation without further steps of treatment. In this study, we demonstrated that ASST positivity was a significant predictor of well-controlled CU during the 6-month stepwise treatment after adjusting for urticaria duration in a multivariate regression model considering the treatment step and duration as covariates in the generalized estimating equation.
When we analyzed time from the onset of symptoms to enrollment in this study, the time appeared to be longer in patients having angioedema, anti-thyroid antibodies, and negative ASST results, albeit not significantly so. Additionally, the presence of angioedema or anti-thyroid autoantibodies had no impact on the control status of urticaria in previous studies. In contrast, our study demonstrated that the mean UAS and CU-QoL over the study period were more favorable in patients with positive ASST results as compared to those with negative ASST results. However, due to the limitations associated with the small number of patients, further prospective studies with a longer time frame using stepwise treatment are necessary to evaluate the clinical utility of ASST and to investigate other factors for predicting the prognosis of CU.
Since only half of the ASST-positive sera induced histamine release from donor basophils, ASST results were suggested to indicate the presence of vasoactive factors other than IgG autoantibodies able to activate basophils.13233 Serum factors present in CU patients are associated with ASST reactivity, and their role in the course of disease remains to be elucidated. We speculate that patients with positive ASST results have serum factors that enable the release of histamine and vasodilators that were controlled by antihistamines, whereas sera from ASST-negative patients may contain inflammatory mediators, such as CRP, that perpetuate inflammation rather than histamine-releasing factors. Therefore, the majority of ASST-positive patients whose urticaria symptoms are induced mainly by histamine are expected to achieve a well-controlled state within 6 months of treatment. Since exacerbating and triggering factors in CU patients are heterogeneous, it is unclear whether urticaria control state assessed at the end of the 6-month period would be maintained in the long term. It is another limitation of our study not to evaluate whether functional histamine releasability of the sera from our study patients was different according to the ASST results. Therefore, further studies are needed to validate the association between ASST reactivity and the long-term prognosis of CU.
In conclusion, a 6-month stepwise treatment approach based on the recent guidelines induced a remission of 3.4% of patients from urticaria, and 35.6% of the 59 CU patients were able to achieve well-controlled status. Changes in the UAS and CUQoL from baseline levels are well correlated with CU control. A positive ASST has been identified as an independent predictor of well-controlled CU. However, future studies should investigate which serum factors that induce ASST reactivity in CU patients are involved in the therapeutic response.
Figures and Tables
Fig. 2
Treatment steps for controlling CU during the study period. Group I, patients with remission or well-controlled CU; Group II, patients with partly controlled or uncontrolled CU.

Fig. 3
Changes in UAS (A) and CU-QoL (B) according to control status. Data are presented as mean±standard error. UAS, urticaria activity score; CU-QoL, chronic urticaria-specific quality of life; group I, patients with remission or well-controlled CU; group II, patients with partly controlled or uncontrolled CU.

Fig. 4
Mean UAS (A) and CU-QoL (B) scores over the study period according to the ASST results. Data are presented as mean±standard error. *P for interaction between time and ASST results at each visit from baseline <0.05. UAS, urticaria activity score; CU-QoL, chronic urticaria-specific quality of life; ASST, autologous serum skin test.

Fig. 5
The proportion of patients who achieved well-controlled CU stratified by their treatment steps and baseline ASST results over the study period. Grey bars show the proportion of patients according to their treatment steps at each visit. Black bars represent the proportion of patients who achieved well-controlled CU with respect to their treatment step at each visit.

Table 1
Baseline characteristics according to the ASST results

Table 2
Comparisons of clinical characteristics of CSU patients according to controlled status after 6-month stepwise treatment

Table 3
Multivariate analysis for urticaria control (group I vs II) after 6-month stepwise treatment
ACKNOWLEDGMENTS
This study was supported by the Dong-A ST Pharmaceutical Company, Korea. The authors wish to acknowledge the Ajou Clinical Trial Center ARO team (supported by a grant from the Korean Health Technology R&D project, Ministry of Health Welfare, ROK (H14C1061) for their generous support of the development of the database and the statistical analysis.
References
1. Saini SS. Chronic spontaneous urticaria: etiology and pathogenesis. Immunol Allergy Clin North Am. 2014; 34:33–52.
2. Maurer M, Weller K, Bindslev-Jensen C, Giménez-Arnau A, Bousquet PJ, Bousquet J, et al. Unmet clinical needs in chronic spontaneous urticaria. A GA(2)LEN task force report. Allergy. 2011; 66:317–330.
3. O'Donnell BF. Urticaria: impact on quality of life and economic cost. Immunol Allergy Clin North Am. 2014; 34:89–104.
4. Zuberbier T, Aberer W, Asero R, Bindslev-Jensen C, Brzoza Z, Canonica GW, et al. The EAACI/GA(2) LEN/EDF/WAO Guideline for the definition, classification, diagnosis, and management of urticaria: the 2013 revision and update. Allergy. 2014; 69:868–887.
5. Bernstein JA, Lang DM, Khan DA, Craig T, Dreyfus D, Hsieh F, et al. The diagnosis and management of acute and chronic urticaria: 2014 update. J Allergy Clin Immunol. 2014; 133:1270–1277.
6. Greaves M. Chronic urticaria. J Allergy Clin Immunol. 2000; 105:664–672.
7. Gaig P, Olona M, Muñoz Lejarazu D, Caballero MT, Domínguez FJ, Echechipia S, et al. Epidemiology of urticaria in Spain. J Investig Allergol Clin Immunol. 2004; 14:214–220.
8. Kozel MM, Mekkes JR, Bossuyt PM, Bos JD. Natural course of physical and chronic urticaria and angioedema in 220 patients. J Am Acad Dermatol. 2001; 45:387–391.
9. Hiragun M, Hiragun T, Mihara S, Akita T, Tanaka J, Hide M. Prognosis of chronic spontaneous urticaria in 117 patients not controlled by a standard dose of antihistamine. Allergy. 2013; 68:229–235.
10. Losol P, Yoo HS, Park HS. Molecular genetic mechanisms of chronic urticaria. Allergy Asthma Immunol Res. 2014; 6:13–21.
11. Toubi E, Kessel A, Avshovich N, Bamberger E, Sabo E, Nusem D, et al. Clinical and laboratory parameters in predicting chronic urticaria duration: a prospective study of 139 patients. Allergy. 2004; 59:869–873.
12. Sabroe RA, Grattan CE, Francis DM, Barr RM, Kobza Black A, Greaves MW. The autologous serum skin test: a screening test for autoantibodies in chronic idiopathic urticaria. Br J Dermatol. 1999; 140:446–452.
13. Rabelo-Filardi R, Daltro-Oliveira R, Campos RA. Parameters associated with chronic spontaneous urticaria duration and severity: a systematic review. Int Arch Allergy Immunol. 2013; 161:197–204.
14. Ye YM, Park JW, Kim SH, Choi JH, Hur GY, Lee HY, et al. Clinical evaluation of the computerized chronic urticaria-specific quality of life questionnaire in Korean patients with chronic urticaria. Clin Exp Dermatol. 2012; 37:722–728.
15. Ye YM, Jin HJ, Hwang EK, Nam YH, Kim JH, Shin YS, et al. Co-existence of chronic urticaria and metabolic syndrome: clinical implications. Acta Derm Venereol. 2013; 93:156–160.
16. Zuberbier T, Asero R, Bindslev-Jensen C, Walter Canonica G, Church MK, Giménez-Arnau AM, et al. EAACI/GA(2)LEN/EDF/WAO guideline: management of urticaria. Allergy. 2009; 64:1427–1443.
17. Konstantinou GN, Asero R, Maurer M, Sabroe RA, Schmid-Grendelmeier P, Grattan CE. EAACI/GA(2)LEN task force consensus report: the autologous serum skin test in urticaria. Allergy. 2009; 64:1256–1268.
18. Ye YM, Hur GY, Park HJ, Kim SH, Kim HM, Park HS. Association of specific IgE to staphylococcal superantigens with the phenotype of chronic urticaria. J Korean Med Sci. 2008; 23:845–851.
19. Sahiner UM, Civelek E, Tuncer A, Yavuz ST, Karabulut E, Sackesen C, et al. Chronic urticaria: etiology and natural course in children. Int Arch Allergy Immunol. 2011; 156:224–230.
20. van der Valk PG, Moret G, Kiemeney LA. The natural history of chronic urticaria and angioedema in patients visiting a tertiary referral centre. Br J Dermatol. 2002; 146:110–113.
21. Kasperska-Zajac A, Sztylc J, Machura E, Jop G. Plasma IL-6 concentration correlates with clinical disease activity and serum C-reactive protein concentration in chronic urticaria patients. Clin Exp Allergy. 2011; 41:1386–1391.
22. Rorsman H. Basopenia in urticaria. Acta Allergol. 1961; 16:185–215.
23. Grattan CE, Dawn G, Gibbs S, Francis DM. Blood basophil numbers in chronic ordinary urticaria and healthy controls: diurnal variation, influence of loratadine and prednisolone and relationship to disease activity. Clin Exp Allergy. 2003; 33:337–341.
24. Ye YM, Yang EM, Yoo HS, Shin YS, Kim SH, Park HS. Increased level of basophil CD203c expression predicts severe chronic urticaria. J Korean Med Sci. 2014; 29:43–47.
25. Fusari A, Colangelo C, Bonifazi F, Antonicelli L. The autologous serum skin test in the follow-up of patients with chronic urticaria. Allergy. 2005; 60:256–258.
26. Kulthanan K, Jiamton S, Gorvanich T, Pinkaew S. Autologous serum skin test in chronic idiopathic urticaria: prevalence, correlation and clinical implications. Asian Pac J Allergy Immunol. 2006; 24:201–206.
27. Nettis E, Dambra P, D'Oronzio L, Cavallo E, Loria MP, Fanelli M, et al. Reactivity to autologous serum skin test and clinical features in chronic idiopathic urticaria. Clin Exp Dermatol. 2002; 27:29–31.
28. Caproni M, Volpi W, Giomi B, Cardinali C, Antiga E, Melani L, et al. Chronic idiopathic and chronic autoimmune urticaria: clinical and immunopathological features of 68 subjects. Acta Derm Venereol. 2004; 84:288–290.
29. Vohra S, Sharma NL, Mahajan VK, Shanker V. Clinicoepidemiologic features of chronic urticaria in patients having positive versus negative autologous serum skin test: a study of 100 Indian patients. Indian J Dermatol Venereol Leprol. 2011; 77:156–159.
30. Kocatürk E, Kavala M, Kural E, Sarıgul S, Zındancı I. Autologous serum skin test vs autologous plasma skin test in patients with chronic urticaria: evaluation of reproducibility, sensitivity and specificity and relationship with disease activity, quality of life and anti-thyroid antibodies. Eur J Dermatol. 2011; 21:339–343.
31. Staubach P, Onnen K, Vonend A, Metz M, Siebenhaar F, Tschentscher I, et al. Autologous whole blood injections to patients with chronic urticaria and a positive autologous serum skin test: a placebo-controlled trial. Dermatology. 2006; 212:150–159.
32. Sabroe RA, Greaves MW. Chronic idiopathic urticaria with functional autoantibodies: 12 years on. Br J Dermatol. 2006; 154:813–819.
33. Kawakami T, Kashiwakura J, Kawakami Y. Histamine-releasing factor and immunoglobulins in asthma and allergy. Allergy Asthma Immunol Res. 2014; 6:6–12.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download