Abstract
A novel delayed anaphylactic reaction to red meat, associated with tick bites and IgE antibodies against galactose-α-1, 3-galactose (α-gal), was reported in 2009 in the US, Australia and Europe. In this case, serum specific IgE to galactose-α-1, 3-galactose (>100 kU/L) and IgE to multiple non-primate mammalian proteins were positive. However, the pathogenesis of this disease remains unclear. We report the first case in Asia of delayed anaphylactic reaction to red meat, which was induced by bites from the hard tick, Hematophagous ixodidae. We confirmed the increased concentration of IgE reactive epitopes in non-primate mammalian organs, which may be rich in α-gal proteins in lymphatic and endothelial tissues. All confirmed ticks associated with this disorder in the literature and in our case belonged to the hard tick family. We hypothesize that hard tick saliva is enriched with blood-type substances, such as oligosaccharides, from the non-primate mammal victim's blood after days to weeks of blood sucking, which sensitizes humans through the injection route while blood sucking.
A novel delayed anaphylactic reaction to red meat was first reported in 2009 in the US, Australia and Europe. This phenomenon was related to tick bites, which are thought to induce IgE antibodies against galactose-α-1,3-galactose (α-gal).1,2,3 However, the pathogenesis of this disease remains unclear. Here, we report a case of delayed anaphylaxis to red meat with sensitization to α-gal and various non-primate mammalian proteins. To our knowledge, this is the first case of delayed anaphylactic reaction to red meat in Asia.
A 56-year-old female visited our clinic with primary complaints of urticaria and anaphylaxis at midnight on 2 occasions. Two weeks before this presentation, she experienced hives with intensive itch and slight palpitations with normal blood pressure at 11 pm. She denied dyspnea or disturbance of consciousness and reacted well to dexamethasone (5 mg) and diphenhydramine (20 mg) intramuscularly. She had eaten 4 hours before the reaction and denied any changes in diet. Three days before her appointment, she experienced a second episode at midnight. Extensive itchy hives rapidly extended from the buttocks to all over the body. She was administered a tablet of cetirizine (10 mg) and felt the urge to have a bowel movement. She showed dizziness, palpitation, hyperhidrosis, chest tightness and dyspnea soon after defecation. She was extremely fatigued and experienced a feeling of impending death, and lost consciousness subsequently. She was sent to the emergency room and her blood pressure was measured as 70/30 mmHg. She reacted well to epinephrine (0.5 mL) intramuscularly and methylprednisolone (40 mg) intravenously. She had eaten 5 hours prior to this reaction. The meal included chicken, eggs, pork, corn, wheat, millet, eggplant, tomatoes and onions. She denied intake of alcohol, seafood or any medicines prior to the episode. She had previously been diagnosed with infiltrating ductal carcinoma of the right breast and had been treated with surgery followed by radiotherapy, as well as chemotherapy consisting of vinorelbine and capecitabine, which were stopped 7 months before the anaphylaxis attacks. She had no history of monoclonal antibody therapy, including with cetuximab. She lived near farmland with cattle and outdoor dogs. There was no history of allergy, asthma, rhinitis, metabolic disorders, or cardiovascular disease.
Complete blood count, biochemical test panel, complement fractions C3 and C4, antinuclear antibody and tryptase levels were normal. Intracutaneous allergen skin tests to a food panel were negative, except for cow's milk, pork, beef and lamb (Fig. 1).
Fluorenzymeimmunoassy results for IgE were as follows (ImmunoCAP, Phadia, Sweden): total-IgE 276 kU/L, pork (15.4 kU/L), beef (1.98 kU/L), rabbit meat (2.29 kU/L), cow's milk (3.62 kU/L), dog dander (1.19 kU/L), cat dander (1.30 kU/L), and rat proteins (0.40 kU/L). IgE to mites, a mold mixture panel, and a spring pollen mixture panel including birch pollen, shrimp, chicken, maize, millet, rice, wheat and gluten were all negative. Specific IgE to α-gal was strongly positive (>100 kU/L). Bovine thyroglobulin served as the antigen absorbed in the solid phase in the assay.
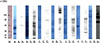
Previous studies have shown that fresh extracts of red meat contain more α-gal than commercial extracts, and hence may produce better skin test results.1,3 In addition, non-primate mammalian organs such as kidney contain a higher content of α-gal epitopes, which may contribute to the severity of anaphylactic reactions.4,5 Western blotting was performed to analyze the antigen-binding characteristics of serum specific IgE antibodies with pork extracts (with blood), organs and bovine thyroglobulin (Thyroglobulin from Bovine Thyroid Gland, Wako SHIRAI Japan, Lot SDP6845), which are rich in 1, 3-galac (α-gal)-gal, using sera from the patient and a negative control (Fig. 2). Both the intensity of the reaction and the number of positive bands with the patient serum were stronger for organ meat (lanes B3, C3, D3, E3, F3, G3) than pork meat (lane A3), which was suggestive of a higher concentration of α-gal epitopes in organs. This may be due to increased expression of α-gal epitopes in lymphatic and endothelial tissue, which are prevalent in organ meat. The pork protein bound to the patient serum (lane A3) at 40, 80, and 120 kDa, similar to a previous study that identified five major groups of molecules with α-gal structures in pig lymphocytes and endothelial cells.6 The specific IgE binding proteins from denatured bovine thyroglobulin, with molecular weights of 52, 68, 90, 140, and 165 kDa (as shown in lane G3), were thought to contain high levels of α-gal epitopes that could induce high levels of specific IgE to α-gal (>100 kU/L) compared to the moderate levels of specific IgE to pork or beef in the ImmunoCAP assay.
Based on the questionnaire on tick bites,7 the patient noticed ticks on the dogs and cattle on her farm and had been bitten ~2-3 weeks before the first attack of anaphylaxis; large local reactions resulted, which healed with topical corticosteroid treatment. Some ticks parasitic on her dogs were captured upon request, which were identified as Haemaphysalis longicornis, one of the most common Hematophagous ixodidae in north China (Fig. 3).
The patient was diagnosed with delayed anaphylaxis to red meat according to the history, skin tests, serological tests, and immunoblotting. Antihistamine and adrenalin, as well as a medical recommendation to avoid red meat, were given. During the 2-year follow-up, she reported mild urticaria several hours after exposure to red meat twice-once after unexpected intake of pork and once after "a bite of" bovine organs. She reacted well to oral antihistamine without an ER visit. The reason for the recurrence was unexpected exposure and unawareness of cross reactivity.
It remains unclear how tick bites induce α-gal sensitization and how delayed anaphylaxis can be triggered by consumption of meat containing α-gal. According to the 32 confirmed cases of tick bite-induced IgE antibodies against 1,3-galac-(α-gal)-gal, the suspected ticks are Amblyomma americanum, Ixodes holocyclus, and Ixodes ricinu, which all belong to the family Ixodidae (hard ticks).1,2,3,7,8 The culprit ticks in this case were also hard ticks, which are unique among bloodfeeders for their prolonged feeding period of several days to 2 weeks, during which time the ticks secrete saliva rich in antihemostatic agent to evade the host's defense mechanisms.9 We hypothesize that tick saliva may be contaminated with oligosaccharides from non-primate mammal blood, which is obtained during blood sucking. In this report, the patient became sensitized to α-gal through the "injection" route by tick bites since she had a history of tick bites but had never received monoclonal antibody therapy, such as with cetuximab (with α-gal located on the Fab portion). Ticks are known to serve as vectors for the pathogen that causes Lyme disease or tick-borne encephalitis9; based on these results, ticks may also serve as a "vector" of α-gal, the blood-type substance of oligosaccharides, into humans.
Figures and Tables
Fig. 2
Western blot analysis of the antigen-binding characteristics of serum specific IgE antibodies with pork, organs and bovine thyroglobulin using sera from the patient and a negative control. Lane M: molecular weight markers. Lane A1, B1, C1, D1, E1, F1, G1: protein profiles of pork extracts, porcine liver, porcine intestines, porcine kidney, bovine kidney, bovine heart, and bovine thyroglobulin, respectively (Amido Black 10B staining of the blotted membrane following SDS-PAGE performed on a 12.5% polyacrylamide gel with 20 µg of sample in each lane). Lanes A2, B2, C2, D2, E2, F2, G2: Immunoblotting patterns of protein extracts using negative control serum in accordance with the above order. A3, B3, C3, D3, E3, F3, G3: Immunoblotting patterns of protein extracts with the patient serum in accordance with the above order.
ACKNOWLEDGMENTS
We would like to thank Yuxuan Wang (Emory University, Rollins School of Public Health, Department of Behavioral Sciences and Health Education, 1518 Clifton Rd. NE, Atlanta, GA, USA 30322) for his help with revision of the manuscript.
References
1. Commins SP, Satinover SM, Hosen J, Mozena J, Borish L, Lewis BD, Woodfolk JA, Platts-Mills TA. Delayed anaphylaxis, angioedema, or urticaria after consumption of red meat in patients with IgE antibodies specific for galactose-alpha-1,3-galactose. J Allergy Clin Immunol. 2009; 123:426–433.
2. Van Nunen SA, O'Connor KS, Clarke LR, Boyle RX, Fernando SL. An association between tick bite reactions and red meat allergy in humans. Med J Aust. 2009; 190:510–511.
3. Jacquenet S, Moneret-Vautrin DA, Bihain BE. Mammalian meat-induced anaphylaxis: clinical relevance of anti-galactose-alpha-1,3-galactose IgE confirmed by means of skin tests to cetuximab. J Allergy Clin Immunol. 2009; 124:603–605.
4. Morisset M, Richard C, Astier C, Jacquenet S, Croizier A, Beaudouin E, Cordebar V, Morel-Codreanu F, Petit N, Moneret-Vautrin DA, Kanny G. Anaphylaxis to pork kidney is related to IgE antibodies specific for galactose-alpha-1,3-galactose. Allergy. 2012; 67:699–704.
5. Spiro RG, Bhoyroo VD. Occurrence of alpha-D-galactosyl residues in the thyroglobulins from several species. Localization in the saccharide chains of the complex carbohydrate units. J Biol Chem. 1984; 259:9858–9866.
6. Vaughan HA, McKenzie IF, Sandrin MS. Biochemical studies of pig xenoantigens detected by naturally occurring human antibodies and the galactose alpha(1-3)galactose reactive lectin. Transplantation. 1995; 59:102–109.
7. Commins SP, James HR, Kelly LA, Pochan SL, Workman LJ, Perzanowski MS, Kocan KM, Fahy JV, Nganga LW, Ronmark E, Cooper PJ, Platts-Mills TA. The relevance of tick bites to the production of IgE antibodies to the mammalian oligosaccharide galactose-α-1,3-galactose. J Allergy Clin Immunol. 2011; 127:1286–1293.e6.
8. Nuñez R, Carballada F, Gonzalez-Quintela A, Gomez-Rial J, Boquete M, Vidal C. Delayed mammalian meat-induced anaphylaxis due to galactose-alpha-1,3-galactose in 5 European patients. J Allergy Clin Immunol. 2011; 128:1122–1124.e1.
9. Chmelar J, Calvo E, Pedra JH, Francischetti IM, Kotsyfakis M. Tick salivary secretion as a source of antihemostatics. J Proteomics. 2012; 75:3842–3854.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download