Abstract
Purpose
This study was aimed to investigate the relationship between the allergen components and moderate-to-severe allergic reactions in patients with buckwheat allergy.
Methods
Fifteen patients with a history of buckwheat ingestion and a buckwheat specific IgE level≥0.35 kU/L were enrolled. They were divided into 2 groups according to clinical severity scores, with 0-1 being asymptomatic-to-mild and 2-4 being moderate-to-severe symptoms. Immunoblotting was performed to investigate IgE reactivity toward buckwheat allergens and to measure intensity of each component by using a reflective densitometer.
Results
The proportions of positive band to the 16 kDa (62.5% vs 0%, P=0.026) and 40-50 kDa (87.5% vs 28.6%, P=0.041) buckwheat allergens in the grade 2-4 group were higher than those in grade 0-1 group. The level of buckwheat specific IgE of grade 2-4 group was higher than that of grade 0-1 group (41.3 kU/L vs 5.5 kU/L, P=0.037). The median optical densities (ODs) of IgE antibody binding to 40-50 kDa protein were higher in the grade 2-4 group, compared with those in the grade 0-1 group (130% OD vs 60.8% OD, P=0.037).
Buckwheat is a member of the Polygonaceae group of herbaceous species. Fagopyrum esculentum Moench and Fagopyrum tataricum Gaertn are most often used as an ingredient of buckwheat foods such as noodles, Muk (jellied food), Jeon (pancake) and tea in Korea. Buckwheat is a popular traditional food in Asian countries and has more recently become increasingly popular in many countries in Europe and North America as a health food.
Buckwheat is one of the major foods causing allergic reactions with severe symptoms in Korea.1,2,3 The prevalence of buckwheat allergy in Korea was 0.10% (25 of 27,425) and 0.13% (19 of 14,777) in elementary schools and middle schools, respectively, according to the International Study of Asthma and Allergies in Childhood survey in 2000.4 Despite the low prevalence, buckwheat can induce serious immediate allergic reactions such as anaphylaxis.1 Therefore, proper diagnosis and prediction of serious allergic reaction of buckwheat are essential.
The detection of buckwheat specific IgE (sIgE) using the ImmunoCAP system has been used to diagnose buckwheat allergy.5 However, the presence of sIgE does not always identify the development of allergic symptoms. Recently molecular diagnostic technologies, such as component-resolved diagnosis, have been introduced to predict the severity and the presence of buckwheat allergy.6,7,8 Fag e 1 (24 kDa), Fag e 2 (16 kDa), Fag e 3 (19 kDa), 10 kDa, and 9 kDa proteins were identified as major allergens. Fag e 1 (24 kDa), the β-subunit of 11S globulin that was previously reported as a major allergen of buckwheat, shows IgE reactivity on most patients regardless of their symptoms.9,10 Fag e 2 (16 kDa), a member of 2S albumin, is highly resistant to peptic hydrolysis11,12 and is the most allergenic protein.13 Fag e 3 (19 kDa), a vicilin, has no homology with other buckwheat allergens and distinguishes symptomatic individuals from asymptomatic patients more exclusively. The 10 kDa protein (Fag e 10 kDa) is classified as 2S albumin and was reactive to buckwheat in 57% of patients in a previous study.14
There have been only a few reports in the literature regarding the difference in allergens according to the clinical severity of buckwheat allergy, although specific allergens could be associated with clinical manifestations of different severity.15 Predicting the clinical severity would be valuable in the management of patients with buckwheat allergy. Therefore, we investigated the relationship between the allergen components and moderate-to-severe allergic reactions in patients with buckwheat allergy.
We enrolled patients with a history of buckwheat ingestion and buckwheat sensitization at the Allergy Clinic of Samsung Medical Center. Buckwheat sensitization was defined as the buckwheat sIgE level≥0.35 kU/L by using the ImmunoCAP system (Thermo Fisher Scientific, Waltham, MA, USA). History of allergic symptoms after eating buckwheat was evaluated and clinical severity of symptoms were assessed on a 0-5 scale with a reported grading system of peanut allergy16: 0 indicating no symptoms; 1 indicating abdominal pain that resolved without medical treatment, rhinoconjunctivitis, urticaria fewer than 10 papules, or rash (eczema onset); 2 indicating 1 organ involved, abdominal pain requiring treatment, generalized urticaria, non-laryngeal angioedema, or mild asthma (cough or fall of peak expiratory flow<20%); 3 indicating 2 organs involved; 4 indicating 3 organs involved, asthma requiring treatment, laryngeal edema or hypotension; and 5 indicating cardiac and respiratory symptoms requiring hospitalization in intensive care. Patients were divided into 2 groups based on the clinical severity: asymptomatic-to-mild (grades 0-1) and moderate-to-severe (grades 2-4) group. After written informed consent was received, blood samples were obtained and the serum samples were frozen at -80℃ until use. This study was approved by the Samsung Medical Center institutional review board (IRB No. 2012-06-047-001).
Buckwheat protein was extracted as described by Tanaka et al.11 with minor modifications using Buckwheat powder (Fagopyrum esculentum, National Agricultural Cooperative Federation, Bong-pyung, Korea). Five grams of finely ground buckwheat was extracted overnight by shaking at 4℃ in 50 mL 0.086M NaCl (Showa, Gyoda, Japan) solution containing 0.033 M NaHCO3 (Duksan, Ansan, Korea). After centrifugation at 12,000 g for 30 minutes, the supernatant was filtered with a 3,000 Da ultrafilter (Millipore, Cork, Ireland) to exclude proteins exceeding 3,000 Da, and freeze-dried at -80℃. It was stored at -70℃ until use. The protein concentrations were then determined by a Bradford Assay (Bio-Rad, Hercules, CA, USA) using a microplate reader (Bio-Rad).
The protein extracts were separated by sodium dodecyl sulfate-polyacrylamide gel electrophoresis (SDS-PAGE) according to the method described by Laemmli.17 The samples were then reduced by heating with 4x SDS-PAGE gel loading buffer (LDS Sample Buffer, Novex, Carlsbad, CA, USA), mixed 1:10 with reducing agent (Novex, Carlsbad, CA, USA), and loaded into each well of a 4%-12% Bis-Tris Aminomethane Gel (NuPAGE; Invitrogen, Carlsbad, CA, USA). Precision plus protein standards (Bio-Rad) were used as molecular weight markers to estimate the protein size. For immunoblotting, proteins from buckwheat were transferred from the gel onto a polyvinylidene difluoride membrane using an iBlot Dry Blotting System (Invitrogen). The membrane was blocked with 2% nonfat dried milk (NFDM) for 1 hour at room temperature, after which it was incubated with the serum samples diluted 1:10 in 2% NFDM for overnight at 4℃. The membrane was then washed 3 times with phosphate-buffered saline containing 0.03% Tween-20 (PBST) for 10 minutes each and incubated with biotin-labeled goat IgG anti-human IgE (KPL, Gaithersburg, MD, USA) diluted 1:4,000 in 2% NFDM for 1 hour at room temperature. Next, the membrane was washed three times with PBST as described, after which it was incubated with NeutrAvidin horseradish peroxidase (Pierce Chemical, Rockford, IL, USA) for 30 minutes at room temperature. After three PBST washes, the membrane was reacted with ECL reagent (GE Healthcare Bio-Sciences AB, Uppsala, Sweden) for 2 minutes. The membrane was then exposed to high-performance chemiluminescence film (GE Healthcare Limited, Buckinghamshire, UK), after which the film was developed.
The band intensity of immunoblots of buckwheat proteins were measured using a reflective densitometer (Bio-Rad). Detection of an individual protein band was defined as optical density (OD/mm2) more than 2 standard deviations (SD) from the mean in backgrounds.
For the statistical analysis, values>100 kUA/L were assigned a value of 101 kUA/L. Total IgE, buckwheat sIgE, relative optical density (OD) of immunoblots of each buckwheat protein (16, 24, 30, 40-50, 75, and 100 kDa) were analyzed between the grade 0-1 and grade 2-4 groups using Mann-Whitney U-tests. The proportions of positive band to the allergens were analyzed between the grade 0-1 and grade 2-4 groups using Fisher's exact test. A P value<0.05 was considered significant. The analysis was performed using SPSS for Windows (version 20.0; Chicago, IL, USA).
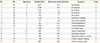
Fifteen patients (12 boys and 3 girls) were included in this study (median age, 5 years). Seven subjects presented with grade 0-1 allergic symptoms after ingestion of buckwheat, and eight subjects had grade 2-4 allergic reactions requiring treatment (Table 1). The median buckwheat sIgE level was 33.6 kU/L (interquartile range [IQR] 4.9-44.4 kU/L).
Immunoblotting identified eight allergens: 16, 24, 30, 40-50 (40-, 45-, 48-kDa), 75, and 100 kDa in the buckwheat protein. The proportions of positive band to the 16 kDa (62.5% vs 0%, P=0.026) and 40-50 kDa (87.5% vs 28.6%, P=0.041) allergens in the grade 2-4 group were higher than those in grade 0-1 group (Fig. 1). However, there was no difference in proportions of IgE detection against 24 kDa (50.0% vs 14.3%, P=0.282), 30 kDa (12.5% vs 28.6%, P=0.569), 75 kDa (12.5% vs 28.6%, P=0.569), and 100 kDa (12.5% vs 28.6%, P=0.569) allergens between 2 groups.
The sera in the grade 0-1 group presented with weak IgE binding intensity with buckwheat proteins, except that of patients 1 and 2. On the other hand, the sera in the grade 2-4 group showed strong IgE binding activity with buckwheat proteins components. Notably, 40-50 kDa and 16 kDa among the protein components showed strong IgE binding intensity in the grade 2-4 group, except subject 8. In addition, IgE binding intensities against 16 kDa were very strong for 5 patients (No. 9, 11, 12, 13, and 15) in the grade 2-4 group than in the grade 0-1 group. The level of buckwheat sIgE of grade 2-4 group was higher than that of grade 0-1 group (41.3 kU/L vs 5.5 kU/L, P=0.037) (Fig. 2). The median ODs of IgE antibody binding to 40-50 kDa protein were also higher in the grade 2-4 group, compared with those in the grade 0-1 group (130% OD vs 60.8% OD, P=0.037). However, there were no differences in total IgE levels and binding activity to 16, 24, 30, 75, and 100 kDa proteins between the 2 groups (P=0.165, 0.203, 0.728, 0.355, 0.165, and 0.908).
Buckwheat is a major food allergen that can cause severe allergic reactions, such as anaphylaxis, in Korean children.18,19 To confirm buckwheat allergy using double-blind placebo-controlled food challenge (DBPCFC) is time-consuming and can be life-threatening, although it is the diagnostic gold standard of food allergy.20 The measurements of food sIgE antibody levels and sIgE to individual components could be a useful method for diagnosing symptomatic allergy and for predicting the clinical severity in a large number of children that may eliminate the need to perform DBPCFC.21 However, controversy exists concerning the usefulness of food sIgE levels for the prediction of clinical allergy,22,23 and the reactivity to different buckwheat allergens has not been evaluated for its contribution to clinical patterns of patients with buckwheat allergy. The present study implicates the 40-50 kDa cluster and 16 kDa buckwheat proteins as important allergens to predict moderate-to-severe (grade 2-4) symptoms in Korean children. In addition, the level of buckwheat sIgE was significantly higher in the moderate-to-severe (grade 2-4) group, suggesting that buckwheat sIgE could be applicable for predicting more severe reaction in a clinical setting.
In the present study, 16, 24, 30, 40-50, 75, and 100 kDa were IgE-reactive proteins and 16 kDa, 24 kDa, and 40-50 kDa (40, 45, 48 kDa) were major allergens. IgE bindings to 40-, 45-, and 48-kDa were shown in a similar pattern, so 40-, 45-, and 48-kDa were analyzed in cluster (40-50 kDa). The immunologic profiles of buckwheat allergens have been studied by several investigators. Nagata et al.24 described that the 24 kDa molecule was the most prominent allergen recognized with IgE. Yoshimasu et al.12 reported that IgE binding was detected to proteins with molecular masses of approximately 14 and 18 kDa. Park et al.25 showed that the allergens of 24, 19, 16, and 9 kDa were strong candidates to be major allergens, and the 19-kDa allergen was relatively specific for buckwheat-allergic patients. Heffer et al.15 identified several IgE-binding proteins and grouped proteins into three patterns: a 16-kDa band in patients with predominantly gastrointestinal symptoms with grass and wheat flour co-sensitization, a 25-kDa band in patients with predominantly cutaneous symptoms and a low frequency of co-sensitization, and a 40-kDa band in patients with anaphylaxis and a low frequency of co-sensitization. Although a variety of allergens were reported, only 3 allergens, Fag e 1 (24 kDa), Fag e 2 (16 kDa), and Fag e 3 (19 kDa) have been considered as major allergens. We found that 40-, 45-, and 48-kDa proteins reacted with specific IgE from patients with buckwheat allergy, especially those who had moderate-to-severe clinical symptoms. The role of these proteins in buckwheat allergy may have been underestimated, even though 40 kDa was reported to be associated with anaphylaxis15 and 45-, and 48-kDa were mentioned in previous papers.24,25 Fag e 3 (19 kDa) was the most specific buckwheat allergen in a Korean study,25 while it did not react with specific IgE in other studies.15,24 In this study, we could not find the immune reaction with serum from our patients with buckwheat allergy. It might be due to small number of study population and differences in various factors such as ethnicity, age, feeding habits or cooking conditions.25,26,27
Some specific components of crude allergen are reportedly useful to discriminate symptomatic allergic patients from asymptomatic sensitized subject in some foods such as peanut, kiwifruit, carrot and soybean.28,29,30,31,32 In the present study, we quantitatively analyzed immunoblotting profile using OD to measure the binding activity of all specific buckwheat components and investigated the relation of the specific allergens with severe allergic reaction. Specific protein components, 40 kDa, 45 kDa, 48 kDa, and 16 kDa, were more reactive to IgE from the subjects with grade 2-4 symptoms than those with grade 0-1 symptoms in immunoblotting profiles. These results imply that specific allergen components may be associated with severe clinical symptom. Fag e 2, a 2S albumin, is refractory to peptic hydrolysis11,12,13 and measurement of the sIgE to 16 kDa protein is more discriminating than sIgE to whole buckwheat extracts for the diagnosis of clinical reactivity to buckwheat.7 Tanaka et al.11 reported that 16 kDa protein bound with IgE in sera from 9 of 10 patients with immediate hypersensitivity reactions including 8 patients with anaphylaxis, but not in sera from buckwheat sIgE-positive subjects without immediate hypersensitivity reactions. Heffler et al.15 reported that the association of 16 kDa protein with gastrointestinal symptoms, 25 kDa protein with cutaneous symptoms and 40 kDa protein with anaphylaxis, suggesting that specific allergens could be more frequently associated with clinical manifestations of different severity. Our study showed consistent results with these previous studies11,15 and also suggest that further studies on the significance of buckwheat allergens are needed.
This study has some limitations. One is its small sample size and another is that we could not use the DBPCFC test to confirm buckwheat allergy. Considering severe symptoms of buckwheat allergy, it was hard to repeat symptom provocation. Despite the limitations, this study has provided useful information regarding buckwheat allergy.
In conclusion, 40-, 45-, 48-, and 16-kDa proteins in buckwheat may act as important allergens in severe clinical symptoms in patients with buckwheat allergy. Quantitative and qualitative measurements of specific components in buckwheat proteins may be helpful for predicting significant clinical symptoms.
Figures and Tables
Fig. 1
Immunoblotting of buckwheat protein with patients` serum samples. Lanes are: M, molecular weight; S, Sodium dodecyl sulfate-polyacrylamide gel electrophoresis; B, blank; N, normal serum; 1-7, patients with allergic reactions of grade 0 to 1; 8-15, patients with allergic reactions of grade 2 to 4.

Fig. 2
Comparison of IgE level and component binding activity between grade 0-1 group and grade 2-4 group. (A) Level of total IgE (kU/L); (B) Level of buckwheat specific IgE (kU/L); (C) IgE binding activities of subjects' serum against 16 kDa protein component measured by optical density (OD)/mm2 of protein band; (D) OD/mm2 of 24 kDa protein band; (E) OD/mm2 of 30 kDa protein band; (F) OD/mm2 of 40-50 kDa protein band; (G) OD/mm2 of 75 kDa protein band and (H) OD/mm2 of 100 kDa protein band from buckwheat, respectively. *P<0.05.

Table 1
Characteristics of study population
ACKNOWLEDGMENTS
This work was supported by research grant from the Korea Food Research Institute. We appreciate Dosoo Kim for his data filing.
References
1. Ahn K, Kim J, Hahm MI, Lee SY, Kim WK, Chae Y, Park YM, Han MY, Lee KJ, Kim JK, Yang ES, Kwon HJ. Prevalence of immediate-type food allergy in Korean schoolchildren: a population-based study. Allergy Asthma Proc. 2012; 33:481–487.
2. Lee SY, Lee KS, Hong CH, Lee KY. Three cases of childhood nocturnal asthma due to buckwheat allergy. Allergy. 2001; 56:763–766.
3. Lee SY. IgE mediated food allergy in Korean children: focused on plant food allergy. Asia Pac Allergy. 2013; 3:15–22.
4. Oh JW, Pyun BY, Choung JT, Ahn KM, Kim CH, Song SW, Son JA, Lee SY, Lee SI. Epidemiological change of atopic dermatitis and food allergy in school-aged children in Korea between 1995 and 2000. J Korean Med Sci. 2004; 19:716–723.
5. Sohn MH, Lee SY, Kim KE. Prediction of buckwheat allergy using specific IgE concentrations in children. Allergy. 2003; 58:1308–1310.
6. Choi SY, Sohn JH, Lee YW, Lee EK, Hong CS, Park JW. Characterization of buckwheat 19-kD allergen and its application for diagnosing clinical reactivity. Int Arch Allergy Immunol. 2007; 144:267–274.
7. Choi SY, Sohn JH, Lee YW, Lee EK, Hong CS, Park JW. Application of the 16-kDa buckwheat 2 S storage albumin protein for diagnosis of clinical reactivity. Ann Allergy Asthma Immunol. 2007; 99:254–260.
8. Tohgi K, Kohno K, Takahashi H, Matsuo H, Nakayama S, Morita E. Usability of Fag e 2 ImmunoCAP in the diagnosis of buckwheat allergy. Arch Dermatol Res. 2011; 303:635–642.
9. Wang Z, Zhang Z, Zhao Z, Wieslander G, Norbäck D, Kreft I. Purification and characterization of a 24 kDa protein from tartary buckwheat seeds. Biosci Biotechnol Biochem. 2004; 68:1409–1413.
10. Yoshioka H, Ohmoto T, Urisu A, Mine Y, Adachi T. Expression and epitope analysis of the major allergenic protein Fag e 1 from buckwheat. J Plant Physiol. 2004; 161:761–767.
11. Tanaka K, Matsumoto K, Akasawa A, Nakajima T, Nagasu T, Iikura Y, Saito H. Pepsin-resistant 16-kD buckwheat protein is associated with immediate hypersensitivity reaction in patients with buckwheat allergy. Int Arch Allergy Immunol. 2002; 129:49–56.
12. Yoshimasu MA, Zhang JW, Hayakawa S, Mine Y. Electrophoretic and immunochemical characterization of allergenic proteins in buckwheat. Int Arch Allergy Immunol. 2000; 123:130–136.
13. Lee S, Han Y, Do JR, Oh S. Allergenic potential and enzymatic resistance of buckwheat. Nutr Res Pract. 2013; 7:3–8.
14. Matsumoto R, Fujino K, Nagata Y, Hashiguchi S, Ito Y, Aihara Y, Takahashi Y, Maeda K, Sugimura K. Molecular characterization of a 10-kDa buckwheat molecule reactive to allergic patients' IgE. Allergy. 2004; 59:533–538.
15. Heffler E, Nebiolo F, Asero R, Guida G, Badiu I, Pizzimenti S, Marchese C, Amato S, Mistrello G, Canaletti F, Rolla G. Clinical manifestations, co-sensitizations, and immunoblotting profiles of buckwheat-allergic patients. Allergy. 2011; 66:264–270.
16. Astier C, Morisset M, Roitel O, Codreanu F, Jacquenet S, Franck P, Ogier V, Petit N, Proust B, Moneret-Vautrin DA, Burks AW, Bihain B, Sampson HA, Kanny G. Predictive value of skin prick tests using recombinant allergens for diagnosis of peanut allergy. J Allergy Clin Immunol. 2006; 118:250–256.
17. Laemmli UK. Cleavage of structural proteins during the assembly of the head of bacteriophage T4. Nature. 1970; 227:680–685.
18. Nakamura S, Yamaguchi M, Oishi M, Hayama T. Studies on the buckwheat allergose report 1: on the cases with the buckwheat allergose. Allerg Immunol (Leipz). 1974; 20-21:449–456.
19. Takahashi Y, Ichikawa S, Aihara Y, Yokota S. Buckwheat allergy in 90,000 school children in Yokohama. Arerugi. 1998; 47:26–33.
20. Shaker M, Woodmansee D. An update on food allergy. Curr Opin Pediatr. 2009; 21:667–674.
21. Sampson HA. Utility of food-specific IgE concentrations in predicting symptomatic food allergy. J Allergy Clin Immunol. 2001; 107:891–896.
22. Sicherer SH, Wood RA. American Academy of Pediatrics Section On Allergy And Immunology. Allergy testing in childhood: using allergen-specific IgE tests. Pediatrics. 2012; 129:193–197.
23. Söderström L, Kober A, Ahlstedt S, de Groot H, Lange CE, Paganelli R, Roovers MH, Sastre J. A further evaluation of the clinical use of specific IgE antibody testing in allergic diseases. Allergy. 2003; 58:921–928.
24. Nagata Y, Fujino K, Hashiguchi S, Abe N, Zaima Y, Ito Y, Takahashi Y, Maeda K, Sugimura K. Molecular characterization of buckwheat major immunoglobulin E-reactive proteins in allergic patients. Allergol Int. 2000; 49:117–124.
25. Park JW, Kang DB, Kim CW, Ko SH, Yum HY, Kim KE, Hong CS, Lee KY. Identification and characterization of the major allergens of buckwheat. Allergy. 2000; 55:1035–1041.
26. Kim J, Lee J, Park MR, Han Y, Shin M, Ahn K. Special consideration is required for the component-resolved diagnosis of egg allergy in infants. Ann Allergy Asthma Immunol. 2014; 112:53–57.
27. Kim J, Lee JY, Han Y, Ahn K. Significance of Ara h 2 in clinical reactivity and effect of cooking methods on allergenicity. Ann Allergy Asthma Immunol. 2013; 110:34–38.
28. Eller E, Bindslev-Jensen C. Clinical value of component-resolved diagnostics in peanut-allergic patients. Allergy. 2013; 68:190–194.
29. Bublin M, Pfister M, Radauer C, Oberhuber C, Bulley S, Dewitt AM, Lidholm J, Reese G, Vieths S, Breiteneder H, Hoffmann-Sommergruber K, Ballmer-Weber BK. Component-resolved diagnosis of kiwifruit allergy with purified natural and recombinant kiwifruit allergens. J Allergy Clin Immunol. 2010; 125:687–694. 694.e1
30. Nicolaou N, Poorafshar M, Murray C, Simpson A, Winell H, Kerry G, Härlin A, Woodcock A, Ahlstedt S, Custovic A. Allergy or tolerance in children sensitized to peanut: prevalence and differentiation using component-resolved diagnostics. J Allergy Clin Immunol. 2010; 125:191–197.e1-13.
31. Mittag D, Vieths S, Vogel L, Becker WM, Rihs HP, Helbling A, Wüthrich B, Ballmer-Weber BK. Soybean allergy in patients allergic to birch pollen: clinical investigation and molecular characterization of allergens. J Allergy Clin Immunol. 2004; 113:148–154.
32. Ballmer-Weber BK, Wangorsch A, Bohle B, Kaul S, Kündig T, Fötisch K, van Ree R, Vieths S. Component-resolved in vitro diagnosis in carrot allergy: does the use of recombinant carrot allergens improve the reliability of the diagnostic procedure? Clin Exp Allergy. 2005; 35:970–978.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download