Abstract
Purpose
Sensitization to house dust mite (Dermatophagoides pteronyssinus) is a considerable risk factor for the progression of allergic disease. The group 2 allergen from Dermatophagoides pteronyssinus, Der p 2, is considered a major one in patients with specific immunoglobulin E (IgE) to Der p 2. Der p 2 has structural homology with myeloid differentiation 2 (MD-2), which is involved in the lipopolysaccharide-binding component of the Toll-like receptor 4 signaling pathway and the development of inflammation. The aim of this study was to examine the genetic association of single nucleotide polymorphisms (SNPs) in the promoter region of MD-2 with Der p 2-sensitive allergy.
Methods
We investigated associations between cohort's characteristics, including 280 allergic and 80 healthy subjects by examining total IgE, eosinophils, D. pteronyssinus-specific IgE, Der p 2-specific IgE, the number of IgE-producing B cells induced by Der p 2, and the odds ratio of allergic symptoms.
Results
Based on the 1,000 genome project data, the minor allele frequencies of the rs1809441 and rs1809442 are 0.467 and 0.474, respectively. However, the correlation of linkage disequilibrium (LD) between these 2 SNPs is D'=1, the genotype frequencies of the 2 MD-2 (LY96) SNPs (rs1809441 and rs1809442) that are located nearby were significantly different between allergic and health subjects: the TT genotype of rs1809441 and the GG genotype of rs1809442 were more frequent in allergic subjects than in healthy subjects (16.1% vs 2.5% in both genotypes). The allergic patients with these genotypes exhibited significantly higher levels of D. pteronyssinus-specific IgE and Der p 2-specific Ig E, and a larger number of Der p 2-activated B cells. In addition, these 2 SNPs in the MD-2 promoter region were significantly associated with the prevalence of nasal, skin, and asthmatic allergic symptoms.
The incidence of most common allergic diseases, such as bronchial asthma, allergic rhinitis and atopic dermatitis has increased in many Western and developing countries in the past decades.1,2 It has been reported that sensitization to indoor allergens is a main factor for the development of airway hypersensitivity among allergic subjects who are genetically susceptible to having immunoglobulin E (IgE)-mediated responses.3 A strong genetic association with asthma has been supported by studies on families and twins, and many genes have been identified or are suspected to be involved in the pathogenesis of asthma.4,5 These patients are characterized by elevated levels of serum total IgE and allergen-specific IgE antibodies against a wide range of allergens.6 The occurrence and severity of allergic symptoms are associated with exposure to environmental allergens.7 The most predominant indoor allergens in tropical and humid areas are house dust mites, and the 2 most common house dust mites implicated in allergy are Dermatophagoides pteronyssinus (D. pteronyssinus) and Dermatophagoides farinae (D. farinae).8 At least 23 allergenic components have been identified in house dust mites.9 Among these allergens, more than 80% of mite-allergic children with asthma have positive skin test responses to group 1 (Der p 1) and group 2 (Der p 2) allergens.10 In particular, Der p 2 is a major allergen, and it has been reported that 79.2% of patients with allergic asthma and/or rhinitis have specific IgE to Der p 2.11
It has been reported that 80% of asthmatic children in Taiwan are sensitive to D. pteronyssinus.12 MD-1 {encoded by the LYMPHOCYTE ANTIGEN 86 (LY86) gene} and MD-2 {encoded by the LYMPHOCYTE ANTIGEN 96 (LY96 gene)}have been reported to play important roles in the Toll-like receptor (TLR) 4 signaling pathway.13 It has also been suggested that MD-1 and MD-2 are involved in the development of inflammation and atopic disease.14,15 Recently, the promoter polymorphism of MD-1 has been reported to be associated with mite-sensitive allergies possibly to be a susceptible gene for asthma.16 However, the role of MD-2 has yet to be elucidated. Der p 2 has structural homology with MD-2 protein,17 the lipopolysaccharide (LPS)-binding component of the TLR-4 signaling pathway. Der p 2 also has functional homology with MD-2 protein, facilitating signaling through direct interactions with the TLR-4 complex and reconstituting LPS-driven TLR-4 signaling in the absence of MD-2 protein.15 We have previously demonstrated that Der p 2 can up-regulate the expression of MD-2 protein and augment inflammatory cytokine release in B cells.18 Polymorphisms in the MD-2 promoter region have been reported to cause increased mRNA production and to be correlated with the incidence of organ dysfunction and sepsis after major trauma.19 It is conceivable that MD-2 promoter polymorphism and MD-2 gene expression may be associated with Der p 2-sensitive allergy.
In spite of the fact that 156 SNPs are identified within the whole MD-2 gene, as shown in the public SNP database (dbSNP) (www.ncbi.nlm.nih.gov), little is known about the functional significance of these SNPs. The promoter region of MD-2 has been reported to be located within an upstream 2 kb sequence of the gene translational start site.19 This promoter region includes 6 SNP sites (Table 1) within the MD-2 gene according to the dbSNP. Several studies have indicated that genetic variations in the promoter region may affect the transcription of the target gene.20 The promoter region plays an essential role in the regulation of gene transcription because it contains multiple transcription factor-binding sites.20 Increasing evidence suggests that such genetic variants in the promoter region of the CD14 gene are associated with a high expression of soluble CD14 (sCD14)21 and that MD-2 promoter polymorphisms may be an important genetic risk factor for susceptibility to post-traumatic sepsis and vital organ dysfunction.19
The aims of this study were to examine the genetic association of SNPs in the promoter region of MD-2 with Der p 2-sensitive allergy and to investigate their possible functional significance by examining associations of clinical characteristics, such as total IgE, eosinophils, D. pteronyssinus-specific IgE, Der p 2-specific IgE, and the number of IgE-producing B cells induced by Der p 2, with the outcomes of patients with allergic symptoms. Identifying biological functions of the SNPs in the promoter region of MD-2 would help researchers better understand clinical relevance between gene variations and susceptibility to Der p 2-sensitive allergy.
A total of 280 allergic subjects who attended the allergy and clinical immunology outpatient clinics, and 80 healthy subjects who received health checks at Taichung Veterans General Hospital were recruited in this study. Informed written consent was obtained from the participants after the study had been described in detail. The Institutional Review Board of our hospital reviewed and approved the ethical nature of this study (IRB No.CF12009, CF12010 and CF12085). Among the 280 allergic subjects, 172 had nasal symptoms (rhinitis), 146 had skin symptoms (atopic dermatitis or urticaria), and 81 had asthmatic symptoms (airway allergies). None of the healthy controls had immunological disease. Blood samples were drawn, and isolated sera were obtained for the measurement of specific IgE to D. pteronyssinus.
Genomic DNA was isolated from blood samples using QIAamp DNA Blood kits (QIAGEN, Valencia, CA, USA) according to the manufacturer's instructions. The quality and quantity of the purified genomic DNA were checked by agarose gel electrophoresis and spectrophotometry. The DNA samples were stored at -80℃ until use.
All of the SNPs in the entire MD-2 promoter region were detected by polymerase chain reaction (PCR), followed by gel extraction of the PCR products and direct sequencing. The PCR products contained the entire 2 kb MD-2 promoter region, which was amplified by forward primer AF: 5'-ATTTTCTTCTTAAGTGTGCAGAT-3' and reverse primer AR: 5'-TCCACGGCCCCCAGAGGAT-3'; forward primer BF: 5'-TGGGGGCCGTGGACCAGTA-3' and reverse primer BR: 5'-TTTCAGTAAGCAGAAAAGATTTAAC-3'. PCR was performed with denaturation at 94℃ for 5 minutes, followed by 94℃ for 50 seconds, 58℃ for 30 seconds, and 72℃ for 1 minute for 35 cycles, with a final extension at 72℃ for 10 minutes. The PCR products were purified and analyzed by an ABI 3100 sequencer (Applied Biosystems: ABI, CA, USA). Genotyping of 2 SNPs (rs1809441 and rs1809442) in the MD-2 promoter region was performed using Custom TaqMan® SNP Genotyping Assay Mix (Rack ID: 4620713-1 and ID: 186819793-1) and TaqMan® Universal PCR Master Mix. The reactions were performed according to the manufacturer's protocol. Detection of the probe signal with 2 ABI fluorescent dyes (FAM™-Allele 1 and VIC®-Allele 2) was conducted using 96-well plates in an ABI Prism 7900 Real-Time PCR system (Applied Biosystems). Duplicate samples and negative controls were included to ensure genotyping accuracy.
We collected 5 mL of blood samples in serum separator tubes (Kendall Healthcare, Mansfield, MA, USA) and processed within 4 hours. The serum samples were stored at -20℃ until analysis. Specific IgE against D. pteronyssinus was measured using ImmunoCap® (Thermo Fisher Scientific Inc. Manufacturer: Phadia AB, Uppsala, Sweden) with a UniCAP 250 system according to the manufacturer's instructions. A concentration of greater than 0.35 kU/L was considered positive. The concentration ranged from 0.35 to 100 kU/L. The assay was performed automatically, and the results were calibrated against the World Health Organization standard for IgE. Serum total IgE was measured by ImmuneCAP cellulose solid phase with the ImmuneCAP Total IgE assay (Thermo Fisher Scientific Inc. Manufacturer: Phadia AB, Uppsala, Sweden). The recombinant allergen of D. pteronyssinus, Der p 2, was prepared and used to analyze IgE reactivity by enzyme-linked immunosorbent assay (ELISA) as previously described.22
Human peripheral blood mononuclear cells (PBMCs) were prepared by density centrifugation in Ficoll-paque™PLUS. B cells were then purified by negative selection with a B-cell isolation kit. Non-B cells were indirectly magnetically labeled using a cocktail of biotin-conjugated antibodies against CD2, CD14, CD16, CD36, CD43, and CD235a (glycophorin A), and Anti-Biotin MicroBeads (Miltenyi Biotec, Bergisch Gladbach, Germany). Isolation of highly pure B cells was achieved by depletion of the magnetically labeled cells. Purified B cells were cultured with Der p 2 (10 µg/mL) in the presence of IL-4 (30 ng/mL), IL-21 (25 ng/mL), and anti-CD40 (1 µg/mL) for 5 days in a CO2 incubator. ELISPOT assays were performed using Mabtech™ ELISpot plus Human IgE kits (MABTECH AB, Nacka Strand, Sweden). The number of spot-forming cells in each well was automatically counted with a CTL-ImmunoSpot Analyzer (Cellular Technology Ltd., Shaker Heights, OH, USA).
All statistical analyses were performed using the SPSS software (version 22; SPSS Inc, Chicago, IL, USA). The SPSS Sample Power 2.0 was used for power calculation analysis. The genotype frequency at each SNP was examined for significant departure from Hardy-Weinberg equilibrium by using a χ2 test. Differences in genotype frequency between allergic patients and controls were analyzed by using a χ2 test and by calculating the odds ratio with 95% confidence interval. Linkage disequilibrium between loci was measured by using the absolute value of Lewontin |D'| and r2. The sample power calculation for the association study was >0.8 when at the 2-tailed α=0.05 level. Two-tailed P values lower than 0.05 were considered statistically significant.
Six SNPs of the MD-2 gene promoter region were identified and used to compare the differences in genotype and allelic frequency between allergic and healthy subjects. Three SNPs, rs1809441, rs1809442, and rs16938754, were found to be significantly different between allergic and healthy subjects for the test genotype (P<0.05) (Table S1 in Supplementary data). Furthermore, the frequencies of the G allele of rs11465996, the T allele of rs1809441 and the G allele of rs1809442 were found to be significantly higher in allergic subjects compared to healthy subjects (P<0.05) (Table S2 in Supplementary data). Based on the 1,000 genome project data, the minor allele frequencies of the rs1809441 and rs1809442 are 0.467 and 0.474, respectively. However, the correlation of linkage disequilibrium (LD) between these 2 SNPs is D'=1.
We first tested a smaller cohort, and then recruited more allergic subjects (n=280) with D. pteronyssinus sensitivity and healthy controls (n=80) who were not sensitive to D. pteronyssinus. They were enrolled and genotyped for MD-2 promoter SNPs rs1809441 and rs1809442 to confirm the genotype differences between these 2 populations. Similar results were observed in that the TT genotype of rs1809441 and GG genotype of rs1809442 were found to be more frequent in allergic subjects than in healthy subjects (16.1% vs 2.5%) (Table 1). Significant differences in serum total IgE and Der p 2-specific IgE were observed between allergic subjects and healthy controls (Table S3 in Supplementary data).
Genetic associations between MD-2 gene promoter SNPs and serum levels of mite-specific IgE were examined and analyzed between allergic and healthy subjects. The results showed that allergic patients with the GT and TT genotypes in SNP rs1809441 exhibited significantly higher serum specific IgE levels to D. pteronyssinus and Der p 2 than those with the GG genotype (Table 2). The CG and GG genotypes in SNP rs1809442 were also associated with a high serum IgE level in allergic subjects (Table 3).
The relationships of each genotype of the MD-2 gene promoter SNPs rs1809441 and rs1809442 with serum specific IgE levels to D. pteronyssinus and Der p 2 in allergic subjects were analyzed to further confirm the genotype association of their serum specific IgE levels to D. pteronyssinus and Der p 2. The D. pteronyssinus-specific IgE levels were measured using ImmunoCap®, and a value of greater than 0.35 kU/L was considered positive. The specific IgE levels to Der p 2 were measured by ELISA, and absorbance greater than 0.03 at an optical density of 405 nm was considered positive. The results showed that the GT and TT genotypes in rs1809441 and the GC and GG genotypes in rs1809442 occurred more frequently in allergic subjects with positive IgE to D. pteronyssinus and Der p 2 than in those without (Table S4 in Supplementary data). A total of 360 subjects were analyzed for relationships between genotypes and serum IgE levels, and the results showed that the GT and TT genotypes in SNP rs1809441 were associated with a high level of serum specific IgE to D. pteronyssinus/Der p 2 and that the GG genotype was associated with a low serum IgE level in allergic subjects (Table 2). The GC and GG genotypes in SNP rs1809442 were associated with a high serum level of IgE to D. pteronyssinus/Der p 2, and the CC genotype was associated with a low serum level in allergic subjects (Table 3).
Genetic associations were examined between the 6 genetic polymorphisms in the MD-2 gene promoter region with clinical characteristics, including age, eosinophils, total IgE, D. pteronyssinus-specific IgE, Der p 2-specific IgE, and the number of B cells which could produce IgE after Der p 2 challenge. There were significant associations between 3 MD-2 promoter SNPs (rs1809440, rs1809441, and rs1809442) and clinical parameters of Der p 2 allergy, such as Der p 2-specific IgE and Der p 2-activated B cells (P<0.05) (Table 4). Allergic patients carrying the homozygous TT genotype of SNP rs1809441 and the GG genotype of rs1809442 exhibited significantly higher levels of serum total IgE, mite-specific IgE, Der p 2-specific IgE, and the number of Der p 2-activated B cells than those with the GG (rs1809441) and CC (rs1809442) genotypes (P<0.05) (Table 4).
The odds ratios of allergic symptoms, including nasal, skin, and airway, were compared between different genotypes of SNP rs1809441 and rs1809442 in the MD-2 promoter region. The results showed the GT and TT genotypes of rs1809441 were significantly associated with the prevalence of allergic diseases, including nasal, skin, and asthmatic symptoms compared to the GG genotype (P<0.001) (Table 5), whereas the GC and GG genotypes of rs1809442 were positively associated with the prevalence of the allergic symptoms (P<0.001). When the homozygous genotypes (TT genotype of rs1809441; GG genotype of rs1809442) were compared to the heterozygous genotypes (GT genotype of rs1809441; GC genotype of rs1809442), the prevalence of all 3 features of allergic symptoms were higher in the homozygous genotypes, especially nasal symptom, which were 4-fold increases in comparison to the heterozygous genotypes.
Sensitization to the house dust mite D. pteronyssinus is a considerable risk factor for the progression of allergic diseases, such as asthma, rhinitis, and dermatitis.23 Recently, several large-scale genomewide association studies have been conducted to identify susceptibility loci for asthma, and their results showed an associated locus on chromosome 17q21 embodying the genes ORMDL3, GSDMB, and ZPBP2.24 Genome-wide associations between asthma and SNPs have also been observed in rs3771166 (IL1RL1/IL18R1), rs9273349 (HLA-DQ), rs1342326 (IL-33), rs744910 (SMAD3), and rs2284033 (IL2RB).25 Three SNPs (rs7775228, rs2155219, and rs17513503) at different loci have been identified in a genomewide meta-analysis, which are significantly associated with the risk of allergic and grass sensitization.26 Furthermore, 3 SNPs (rs3918392, rs528557, and rs2787093) in the ADAM33 gene have been reported to be significantly associated with mite-sensitized persistent allergic rhinitis.27
Despite the genomewide meta-analysis studies of genetic variants associated with allergic rhinitis and mite sensitization, no research has focused on interactions between mite sensitization and SNPs in the MD-2 promoter region. In this study, 6 SNPs in the proximal promoter region of the MD-2 gene were analyzed, and 2 SNPs (rs1809441 and rs1809442) in the MD-2 promoter region had statistically significant differences between D. pteronyssinus-allergic patients and healthy controls when the genotypes and allele frequencies were compared. These 2 SNPs of the MD-2 promoter were associated with the presence of high levels of D. pteronyssinus- and Der p 2-specific IgE in the sera of the mite allergy group. Significant associations were also observed between the 2 SNPs of the MD-2 promoter region and high expressions of Der p 2 allergy characteristics, such as Der p 2-specific IgE and Der p 2-activated B cells, in allergic patients. These results suggest that these SNPs in the promoter regions may indicate genes that are susceptible to allergic inflammation caused by D. pteronyssinus, and supports the hypothesis that genetic polymorphisms in the MD-2 promoter region significantly contribute to susceptibility to Der p 2 allergy.
MD-2/TLR-4 signaling has been reported to be involved in many disease processes, including allergy and asthma,28 inflammatory bowel disease,29 increased susceptibility to infection,19 autoimmune encephalomyelitis,30 and multiple sclerosis.30 Therefore, it is conceivable that the MD-2/TLR-4 complex could be a genetic candidate for a variety of inflammatory diseases. The rationale for this study is that MD-2 protein and Der p 2 have structural homology. There are statistically significant differences in associations between the SNPs in the promoter region of the MD-2 gene and D. pteronyssinus allergy. In addition, Der p 2-driven inflammatory responses in PBMCs derived from allergic patients sensitized to D. pteronyssinus are different among different genotypes. Although the importance of MD-2/TLR-4 signaling in LPS responses is well known, the role of Der p 2 in the MD-2/TLR-4 pathway remains controversial.
The role of Der p 2 in the up-regulation of MD-2 expression could not be simply understood due to the structural homology of Der p 2 and MD-2 protein. It has been reported that Der p 2-associated allergic diseases are Th2-dependent and that Th2-cell activation is associated with the expression of the GATA-3 gene. Based on the database of the TRANSFAC MATRIX TABLE transcription factor binding site, the sequence fragments of rs1809441 and rs1809442 were highly correlated with the binding sites of transcription site GATA-3 (data not shown). This suggests that Der p 2 may trigger the promoter of MD-2, followed by activation of GATA-3 and Th2 cells. Although the 2 SNPs (rs1809441 and rs1809442) identified in this way may be related to binding of transcription factor GATA-3 by silico analysis tools (bioinformatics), a report gene promoter assay needs to be further clarified that it will be helpful in elucidating the effect of MD-2 (LY-96) gene promoter SNPs in the MD-2 (LY-96) gene expression.
Since MD-2 protein can play an important role as a cofactor with cell surface TLR-4 and recognition of LPS and since group 2 allergenic components of house dust mite Der p 2 have been reported to serve as an accessory protein in TLR-4 signaling, both LPS and Der p 2 may affect host cells synergistically. In our PBMC study, the number of B cells which could produce IgE was up-regulated by Der p 2 in subjects with both SNP mutants (rs1809441 and rs1809442), suggesting that Der p 2 could trigger a large amount of IgE antibodies in these subjects. B-cell activation and production of specific IgE augmented by Der p 2 in these subjects may also be due to the overexpression of MD-2. Our study showed that the SNPs of MD-2 promoter region to had a high association with Der p 2-specific IgE in the sera and that there was an increase in IgE-producing B cells after Der p 2 stimulation as assessed by ELISpot (P<0.001). Therefore, Der p 2-triggered MD-2/TLR-4 signaling may play an important role only in Der p 2-specific IgE synthesis. MD-2 protein is believed to be a significant accessory protein in TLR-4 signaling, which is involved in bacterial recognition, activation of inflammatory cascades, and many disease processes, including increased susceptibility to infection, inflammatory bowel disease, and allergy. Therefore, it is reasonable to speculate that MD-2 could be a candidate for genetic modification for a variety of inflammatory and atopic diseases.
According to data from a publicly available database (dbSNP, http://www.ncbi.nlm.nih.gov/SNP), allelic frequencies of genetic variations in the MD-2 gene promoter region vary according to ethnicity (for example, rs1809440 C-allele: 0.479 in African Americans and 0.325 in Europeans). These differences may result in diverse genetic roles of these polymorphisms in different populations with regards to the occurrence of certain diseases. Therefore, additional studies are needed to clarify the precise role of these polymorphisms in the pathogenesis of Der p 2 allergy and specific IgE synthesis.
The limitations of this study were that only the promoter region of MD-2 was analyzed and that a limited number of subjects were included. The real significance of MD-2 gene regulation in Der p 2-induced allergic inflammation requires studies with more patients and investigating more genes.
In conclusion, although the pathogenesis of mite allergy may be different among various ethnic popgest that polymorphisms in the MD-2 promoter region may be associated with Der p 2-specific IgE and play a major role in susceptibility to Der p 2-triggered immune responses in a Taiwanese population.
Figures and Tables
Table 1
Comparison of 2 SNPs in the MD-2 gene promoter region between allergic and healthy subjects
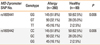
Table 2
Comparison of serum IgE levels of SNP No. rs1809441 in the MD-2 gene promoter region between allergic and healthy subjects
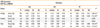
Table 3
Comparison of serum IgE levels of SNP No. rs1809442 in the MD-2 gene promoter region between allergic and healthy subjects
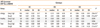
Table 4
Comparison of clinical characteristics of 2 SNPs in the MD-2 gene promoter region among different genotypes in allergic patients (n=52)

Pa for the Kruskal-Wallis test.
S.E.M., standard error of mean; ELISPOT, The number of B-cells which could produce IgE after Der p2 stimulation; Dp IgE, specific IgE to the dust mite Dermatophagoides pteronyssinus; Der p2-IgE, specific IgE to the dust mite Dermatophagoides pteronyssinus group 2 allergen Der p 2.
Table 5
Comparison the odds ratios of allergic symptoms of 2 SNPs in the MD-2 gene promoter region among different genotypes (n=280)

ACKNOWLEDGMENTS
This study was supported by grants (TCVGH-1017302B and NCHU1027617) from Taichung Veterans General Hospital. The authors sincerely appreciate the assistance of the Biostatistics Task Force and the Center for Translational Medicine of Taichung Veterans General Hospital, Taichung, Taiwan.
References
1. Schram ME, Tedja AM, Spijker R, Bos JD, Williams HC, Spuls PI. Is there a rural/urban gradient in the prevalence of eczema? A systematic review. Br J Dermatol. 2010; 162:964–973.
2. Toh ZQ, Anzela A, Tang ML, Licciardi PV. Probiotic therapy as a novel approach for allergic disease. Front Pharmacol. 2012; 3:171.
3. D'Amato G, Liccardi G, D'Amato M, Holgate S. Environmental risk factors and allergic bronchial asthma. Clin Exp Allergy. 2005; 35:1113–1124.
4. LeSouëf P. Genetics of asthma: what do we need to know? Pediatr Pulmonol Suppl. 1997; 15:3–8.
5. Zaas D, Schwartz DA. Genetics of environmental asthma. Semin Respir Crit Care Med. 2003; 24:185–196.
6. Williams AH, Smith JT, Hudgens EE, Rhoney S, Ozkaynak H, Hamilton RG, et al. Allergens in household dust and serological indicators of atopy and sensitization in Detroit children with history-based evidence of asthma. J Asthma. 2011; 48:674–684.
7. Gent JF, Belanger K, Triche EW, Bracken MB, Beckett WS, Leaderer BP. Association of pediatric asthma severity with exposure to common household dust allergens. Environ Res. 2009; 109:768–774.
8. Arlian LG, Morgan MS, Neal JS. Dust mite allergens: ecology and distribution. Curr Allergy Asthma Rep. 2002; 2:401–411.
9. Weghofer M, Grote M, Resch Y, Casset A, Kneidinger M, Kopec J, et al. Identification of Der p 23, a peritrophin-like protein, as a new major Dermatophagoides pteronyssinus allergen associated with the peritrophic matrix of mite fecal pellets. J Immunol. 2013; 190:3059–3067.
10. Schuetze G, Storm van's Gravesande K, Sparhold S, Frischer T, Kuehr J. Comparison between serial skin-prick tests and specific serum immunoglobulin E to mite allergens. Pediatr Allergy Immunol. 1999; 10:138–142.
11. Trombone AP, Tobias KR, Ferriani VP, Schuurman J, Aalberse RC, Smith AM, et al. Use of a chimeric ELISA to investigate immunoglobulin E antibody responses to Der p 1 and Der p 2 in mite-allergic patients with asthma, wheezing and/or rhinitis. Clin Exp Allergy. 2002; 32:1323–1328.
12. Kam KL, Hsieh KH. Comparison of three in vitro assays for serum IgE with skin testing in asthmatic children. Ann Allergy. 1994; 73:329–336.
13. Kimoto M, Nagasawa K, Miyake K. Role of TLR4/MD-2 and RP105/MD-1 in innate recognition of lipopolysaccharide. Scand J Infect Dis. 2003; 35:568–572.
14. Nagai Y, Watanabe Y, Takatsu K. The TLR family protein RP105/MD-1 complex: a new player in obesity and adipose tissue inflammation. Adipocyte. 2013; 2:61–66.
15. Trompette A, Divanovic S, Visintin A, Blanchard C, Hegde RS, Madan R, et al. Allergenicity resulting from functional mimicry of a Toll-like receptor complex protein. Nature. 2009; 457:585–588.
16. Wang JY, Lin CG, Hsiao YH, Liou YH, Wu LS. Single nucleotide polymorphisms and haplotype of MD-1 gene associated with high serum IgE phenotype with mite-sensitive allergy in Taiwanese children. Int J Immunogenet. 2007; 34:407–412.
17. Thomas WR. Molecular mimicry as the key to the dominance of the house dust mite allergen Der p 2. Expert Rev Clin Immunol. 2009; 5:233–237.
18. Tsai JJ, Liu SH, Yin SC, Yang CN, Hsu HS, Chen WB, et al. Mite allergen Der-p2 triggers human B lymphocyte activation and Toll-like receptor-4 induction. PLoS One. 2011; 6:e23249.
19. Gu W, Shan YA, Zhou J, Jiang DP, Zhang L, Du DY, et al. Functional significance of gene polymorphisms in the promoter of myeloid differentiation-2. Ann Surg. 2007; 246:151–158.
20. Wray GA, Hahn MW, Abouheif E, Balhoff JP, Pizer M, Rockman MV, et al. The evolution of transcriptional regulation in eukaryotes. Mol Biol Evol. 2003; 20:1377–1419.
21. Baldini M, Lohman IC, Halonen M, Erickson RP, Holt PG, Martinez FD. A Polymorphism* in the 5' flanking region of the CD14 gene is associated with circulating soluble CD14 levels and with total serum immunoglobulin E. Am J Respir Cell Mol Biol. 1999; 20:976–983.
22. Liao EC, Ho CM, Lin MY, Tsai JJ. Dermatophagoides pteronyssinus and Tyrophagus putrescentiae allergy in allergic rhinitis caused by cross-reactivity not dual-sensitization. J Clin Immunol. 2010; 30:830–839.
23. Henszel Ł, Kuźna-Grygiel W. House dust mites in the etiology of allergic diseases. Ann Acad Med Stetin. 2006; 52:123–127.
24. Akhabir L, Sandford AJ. Genome-wide association studies for discovery of genes involved in asthma. Respirology. 2011; 16:396–406.
25. Moffatt MF, Gut IG, Demenais F, Strachan DP, Bouzigon E, Heath S, et al. A large-scale, consortium-based genomewide association study of asthma. N Engl J Med. 2010; 363:1211–1221.
26. Ramasamy A, Curjuric I, Coin LJ, Kumar A, McArdle WL, Imboden M, et al. A genome-wide meta-analysis of genetic variants associated with allergic rhinitis and grass sensitization and their interaction with birth order. J Allergy Clin Immunol. 2011; 128:996–1005.
27. Chen RX, Lu WM, Zhu LP, Lu MP, Wang ML, Wang YL, et al. Association study on ADAM33 polymorphisms in mite-sensitized persistent allergic rhinitis in a Chinese population. PLoS One. 2014; 9:e95033.
28. Simpson A, Martinez FD. The role of lipopolysaccharide in the development of atopy in humans. Clin Exp Allergy. 2010; 40:209–223.
29. Trøseid M, Lind A, Nowak P, Barqasho B, Heger B, Lygren I, et al. Circulating levels of HMGB1 are correlated strongly with MD2 in HIV-infection: possible implication for TLR4-signalling and chronic immune activation. Innate Immun. 2013; 19:290–297.
30. Kan QC, Zhu L, Liu N, Zhang GX. Matrine suppresses expression of adhesion molecules and chemokines as a mechanism underlying its therapeutic effect in CNS autoimmunity. Immunol Res. 2013; 56:189–196.
Supplementary Material
Table S1
Comparison of genotypic frequency of SNPs in the MD-2 gene promoters region between allergic and healthy subjects
Table S2
Comparison of allele frequencies of SNPs in the MD-2 gene promoter region between allergic and healthy subjects




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download