Abstract
Mulberry (Morus spp.) is a widespread deciduous tree and its fruit is commonly eaten in Korea and eastern Asia. Some reports demonstrate that mulberry fruit is a food allergen in the Mediterranean area. However, there has been no report of systemic allergic reactions after ingesting mulberry fruit in Korea. An 18-year-old boy with a mulberry fruit allergy visited our allergy clinic. He had experienced generalized urticaria, chest tightness, breathing difficulty, and abdominal cramping after ingesting mulberry fruit. The patient had a positive skin reaction to mulberry fruit extract (mean wheal size, 5 mm). We performed an ELISA to detect specific IgE antibody (Ab) to mulberry fruit extract in the patient's serum compared to those of non-atopic healthy controls and birch-sensitized individuals. Specific IgE Ab to mulberry fruit extract was detected in the patient's serum, as compared to non-atopic healthy controls. Another subject, who was strongly sensitized to birch pollen, also had a positive serum-specific IgE Ab to mulberry fruit. We performed IgE immunoblot analysis using the patient's and the other subject's sera, who had serum-specific IgE to mulberry fruit, to identify the IgE-binding component. An identical IgE-binding component to mulberry extract was detected in the two subjects at around 17 kDa, and which might be PR 10 of Bet v 1. In conclusion, mulberry fruit could induce a systemic allergic reaction through an IgE-mediated mechanism, and cross-reactivity might occur between mulberry fruit and birch pollen.
Mulberry fruit (Morus alba, family Moraceae) is commonly used in wine and as a consumed fresh fruit in Korea and eastern Asia. Mulberry fruit is a traditional herbal medicine for improving health. Mulberry tree pollen has been reported to induce pollinosis in the Mediterranean region and India.1,2,3 A few reports of contact urticaria caused by mulberry4 and oral allergy syndrome to jackfruit5 which belongs to Moraceae have been published.
In this study, we report an anaphylactic reaction caused by ingesting mulberry fruit with detection of an IgE-binding component.
This report presents an anaphylactic reaction that occurred in an 18-year-old boy after ingesting mulberry fruit. He had had allergic rhinoconjuctivitis and atopic dermatitis from early childhood. In addition, he had oral allergy syndromes to peach, plum, and apple that included oral itching and lip swelling. His father also had an allergic rhinitis and asthma history. He visited our allergy clinic after experiencing systemic allergic reactions including generalized urticaria, chest tightness, breathing difficulty, oral swelling, runny nose, and nasal obstruction within 30 minutes after eating mulberry fruit. It was the first trial of mulberry fruit for his health promotion. After that event, he never attempted to eat mulberry fruit for his safety.
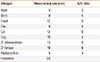
He had no peripheral blood eosinophilia, although serum total IgE was elevated to 278 IU/mL. To identify his atopic status, skin prick testing (SPT) was performed with common inhalant allergens. The results revealed that he was strongly sensitized to several kinds of tree pollens and indoor allergens (Table 1).
For in vitro and in vivo tests, fresh mulberry fruit was purchased and extracted with phosphate-buffered saline (PBS [pH7.5], 1:5 w/v) at 4℃ overnight. This extract was used for the enzyme-linked immunosorbent assay (ELISA), and immunoblot analysis. For SPT, the supernatants were mixed with an equal amount of sterile glycerin. SPT with mulberry fruit extract was also positive (mean wheal size, 5 mm). A non-specific bronchial challenge test with mannitol was performed to evaluate airway hyper-responsiveness, and it was positive [accumulated mannitol dose to cause a 15% fall in forced expiratory volume in 1 second (PD15) was 60.3 mg]. The fraction of exhaled nitric oxide was 85 ppb. Specific IgE Ab to mulberry fruit extract was detected in the patient's serum more than in non-atopic healthy controls (Fig. 1A). Another subject, who was strongly sensitized to birch pollen, was positive for serum-specific IgE Ab to mulberry fruit (Fig. 1B). Furthermore, we performed an IgE immunoblot analysis in the patient's and the other subject's sera who had specific IgE to mulberry fruit to identify the IgE-binding component. We found an identical IgE-binding component to mulberry extract in the two subjects at around 17 kDa (Fig. 2).
Food allergy is a hypersensitive immune reaction after exposure to a particular food allergen. Its pathogenic mechanisms are mainly explained by IgE-mediated reactions.6 Generally, the overall prevalence of food allergy is reported as 1%-2%.7 In a Korean nationwide population study, food allergy prevalence was 3.3%-4.5% in schoolchildren.8 Considering causative food allergens, the prevalence of allergy to fruits and vegetables was estimated at 0.1%-4.3% according to a meta-analysis result.9
Pollen and edible plant products commonly cause pollen-food syndrome that typically manifests as oral symptoms, including tongue edema, lip/perioral swelling, and pruritus of the palate and lips. It is also known as oral allergy syndrome.7 These phenomena result from cross-reactive sensitizations to homologous allergens from pollen (e.g., birch).
Allergenic pollen contains several allergenic components including major and minor allergens. Major allergens are components to which the majority of sensitized patients react while minor allergens are ubiquitous molecules comprised of a cross-reaction of unrelated plant species, involved in general vital functions. These minor allergens are defined as panallergens, in which profilins, non-specific lipid transfer proteins (ns-LTP), procalcins and so on.10 Pathogen-related (PR) proteins are a kind of "defense-related protein" produced in response to a pathogen in higher plants.11 Fourteen families of PR proteins are classified, and some members of them have demonstrated allergenicity. PR proteins have structural homologies in other families of plants. Among them, PR 10 protein has sequence homology to Bet v 1, the major allergen in birch pollen. Its molecular weight is 17.0 kDa. Many of the other PR 10-homologous allergens, including Rosaceae (apple and pear), Prunoideae (cherry and peach), and Apiaceae (celery and carrot), have cross-reactivity with Bet v 1. Therefore, all they can induce birch pollen-related oral allergy syndrome.12 Hemmer et al. identified PR 10 allergens in Moraceae fruits including mulberry fruit, which cross-reacted with Bet v 1.13 Therefore, sensitization to PR 10 proteins can be a cause for the development of pollen-food syndrome.7 Profilins are a family of small molecules (12-15 kDa) that play a role in cytokinesis and cytoplasmatic polymerization.14 As profilin-specific IgE has cross-reactivity with homologies from virtually every plant source, individuals with sensitization to profilin have risk factors for allergic reactions to multiple pollen and food allergen sources.15 Plant ns-LTPs are identified as a kind of fruit allergens causing more severe systemic symptoms compared to birch-related allergens, which cause mild oral allergy syndrome. They are divided into 2 subfamilies according to their molecular masses; the 9-kDa ns-LTP1 and the 7-kDa ns-LTP2.16 There have been some reports on mulberry species allergy, in which ns-LTPs are major culprit allergens. Ciardiello et al. isolated Mor n 3, a ns-LTP 1 from black mulberry and showed its allergenic activity.17 In addition, Micheal et al. reported that they found a 10-kDa protein as a major allergen of paper mulberry pollen, a respiratory allergen, in Pakistan.18 Considering its molecular weight, it can be assumed as a kind of ns-LTP.
In this study, we report a case of systemic allergic reaction after ingestion of mulberry fruit. The patient was strongly sensitized to birch pollen, and had serum specific IgE to a mulberry fruit extract. These findings were suggested the presence of cross-reactivity between birch pollen and mulberry fruit. We identified an identical IgE binding component, at around 17 kDa, in the patient and another subject, strongly sensitized to birch pollen, and mulberry fruit extract confirmed by ELISA. It may have been PR 10 of Bet v 1-related molecules considering its molecular weight. This finding supports the presence of cross-reactivity between mulberry fruit and PR 10 of birch pollen.
In conclusion, we report a case of systemic allergic reaction caused by mulberry fruit in a patient with allergic rhinitis and asthma. This reaction might be explained as an IgE-mediated mechanism by detection of 17 kDa IgE-binding component to a mulberry fruit extract, which is identical to one found in birch pollen. In addition, this finding can be an evidence of cross-reactivity between mulberry fruit and birch pollen.
Figures and Tables
Fig. 1
The level of specific IgE to mulberry fruit extract in the sera of our patient, birch sensitized individuals (n=31), and non-atopic controls (n=20). The positive cut-off value (1.621) was derived from the mean plus three standard deviations of readings from the non-atopic control sera. A, index patient; B, subject with positive serum specific IgE to mulberry fruit in birch sensitized individuals.

Fig. 2
Results of IgE immunoblot analysis to mulberry fruit extract. Blank, buffer control; A, patient's serum; B, serum from a subject who was strongly sensitized to birch pollen and had serum specific IgE antibody to mulberry fruit; NC, non-atopic controls.

References
1. Sneller MR, Hayes HD, Pinnas JL. Pollen changes during five decades of urbanization in Tucson, Arizona. Ann Allergy. 1993; 71:519–524.
2. Subiza J, Jerez M, Jiménez JA, Narganes MJ, Cabrera M, Varela S, Subiza E. Allergenic pollen pollinosis in Madrid. J Allergy Clin Immunol. 1995; 96:15–23.
3. Kosisky SE, Marks MS, Nelson MR. Pollen aeroallergens in the Washington, DC, metropolitan area: a 10-year volumetric survey (1998-2007). Ann Allergy Asthma Immunol. 2010; 104:223–235.
4. Muñoz FJ, Delgado J, Palma JL, Giménez MJ, Monteseirín FJ, Conde J. Airborne contact urticaria due to mulberry (Morus alba) pollen. Contact Dermatitis. 1995; 32:61.
5. Wüthrich B, Borga A, Yman L. Oral allergy syndrome to a jackfruit (Artocarpus integrifolia). Allergy. 1997; 52:428–431.
6. Johansson SG, Bieber T, Dahl R, Friedmann PS, Lanier BQ, Lockey RF, Motala C, Ortega Martell JA, Platts-Mills TA, Ring J, Thien F, Van Cauwenberge P, Williams HC. Revised nomenclature for allergy for global use: report of the Nomenclature Review Committee of the World Allergy Organization, October 2003. J Allergy Clin Immunol. 2004; 113:832–836.
7. Robison RG, Pongracic JA. Chapter 23: food allergy. Allergy Asthma Proc. 2012; 33:Suppl 1. S77–S79.
8. Ahn K, Kim J, Hahm MI, Lee SY, Kim WK, Chae Y, Park YM, Han MY, Lee KJ, Kim JK, Yang ES, Kwon HJ. Prevalence of immediate-type food allergy in Korean schoolchildren: a population-based study. Allergy Asthma Proc. 2012; 33:481–487.
9. Zuidmeer L, Goldhahn K, Rona RJ, Gislason D, Madsen C, Summers C, Sodergren E, Dahlstrom J, Lindner T, Sigurdardottir ST, McBride D, Keil T. The prevalence of plant food allergies: a systematic review. J Allergy Clin Immunol. 2008; 121:1210–1218.e4.
10. Hauser M, Roulias A, Ferreira F, Egger M. Panallergens and their impact on the allergic patient. Allergy Asthma Clin Immunol. 2010; 6:1.
11. van Loon LC, van Strien EA. The families of pathogenesis-related proteins, their activities, and comparative analysis of PR-1 type proteins. Physiol Mol Plant Pathol. 1999; 55:85–97.
12. Midoro-Horiuti T, Brooks EG, Goldblum RM. Pathogenesis-related proteins of plants as allergens. Ann Allergy Asthma Immunol. 2001; 87:261–271.
13. Hemmer W, Focke M, Marzban G, Swoboda I, Jarisch R, Laimer M. Identification of Bet v 1-related allergens in fig and other Moraceae fruits. Clin Exp Allergy. 2010; 40:679–687.
14. Valenta R, Duchene M, Ebner C, Valent P, Sillaber C, Deviller P, Ferreira F, Tejkl M, Edelmann H, Kraft D, Scheiner O. Profilins constitute a novel family of functional plant pan-allergens. J Exp Med. 1992; 175:377–385.
15. Asero R, Mistrello G, Roncarolo D, Amato S, Zanoni D, Barocci F, Caldironi G. Detection of clinical markers of sensitization to profilin in patients allergic to plant-derived foods. J Allergy Clin Immunol. 2003; 112:427–432.
16. Zuidmeer L, van Ree R. Lipid transfer protein allergy: primary food allergy or pollen/food syndrome in some cases. Curr Opin Allergy Clin Immunol. 2007; 7:269–273.
17. Ciardiello MA, Palazzo P, Bernardi ML, Carratore V, Giangrieco I, Longo V, Melis M, Tamburrini M, Zennaro D, Mari A, Colombo P. Biochemical, immunological and clinical characterization of a cross-reactive nonspecific lipid transfer protein 1 from mulberry. Allergy. 2010; 65:597–605.
18. Micheal S, Wangorsch A, Wolfheimer S, Foetisch K, Minhas K, Scheurer S, Ahmed A. Immunoglobulin E reactivity and allergenic potency of Morus papyrifera (paper mulberry) pollen. J Investig Allergol Clin Immunol. 2013; 23:168–175.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download