This article has been corrected. See "Erratum: Butter Tolerance in Children Allergic to Cow's Milk" in Volume 8 on page 178.
Abstract
We performed an oral food challenge (OFC) with 10 g of butter (equivalent of 2.9 mL cow's milk) and 25-mL heated cow's milk for 68 children with cow's milk-allergy. Thirty-eight children reacted only to heated cow's milk. Twenty-four children reacted to neither heated milk nor butter. Thirty-eight (86.4%) of 44 patients with positive results to the OFC for heated milk could safely tolerate butter. It is highly likely that even children with cow's milk-allergy who show positive results to an OFC for heated milk can consume butter. The milk-specific IgE value indicative of a negative predictive value of over 95% was 17.8 kUA/L, and patients with low milk-specific IgE values may be able to safely consume butter. Including butter in the diets of patients with milk-allergy after a butter challenge may improve quality of life.
Some studies have reported that most patients with an allergy to cow's milk can consume heated cow's milk.1 The majority of children with a cow's milk allergy tolerate extensively heated milk products.2 The current management strategy for these patients who do not tolerate extensively heated milk products is only the elimination of cow's milk from the diet. However, butter is used as an ingredient in many foods. Therefore, if children allergic to cow's milk can tolerate butter, their quality of life (QOL) will improve considerably. The purpose of this study was to examine whether children with a cow's milk allergy who also react to heated milk can tolerate butter in their diet.
Patients with a history of immediate reaction to cow's milk were enrolled. Patients who were strongly suspected to have a cow's milk allergy, such as those who experienced an allergic reaction to cow's milk, such as eczema, that improved by elimination of cow's milk and who were positive for cow's milk-specific IgE, were also enrolled. Past history of anaphylaxis was not established as an exclusion criterion, and no exclusion criteria were established with respect to cow's milk-specific IgE antibody titers. We did not use the skin prick test because cow's milk-specific IgE is more useful for the diagnosis of heated cow's milk allergy.1
Oral food challenges (OFCs) were not performed on patients with a history of immediate reaction to cow's milk within the past 6 months or those with comorbid symptoms such as eczema or respiratory symptoms that would affect the determination of OFC results.
We used total and specific IgE values (Immuno CAPTM; Thermo Fisher Scientific, MA, USA) measured within 6 months before the OFC. Cow's milk-specific IgE titers were measured within 6 months of OFC.
The OFC was performed by an open challenge method during hospitalization. We first performed an OFC for butter and then performed an OFC for heated cow's milk, regardless of the test outcome.
In the OFC for butter, we made a sweet potato cake containing 10 g butter (equivalent of 2.9 mL cow's milk) and sweet potatoes. First, the potatoes were boiled and mashed, and then the butter was added. The potato cake was administered either all at once or for patients with a past history of severe reaction to cow's milk, in 2 portions administered 1 hour apart. For the heated cow's milk OFC, we used a pumpkin cake containing 25 mL of cow's milk. The pumpkin cake was heated in a microwave (1,000 W for 1 minute and 30 seconds at a temperature of 89℃). We performed the OFC for heated cow's milk by administering the cake in 2 separate portions 1 hour apart. Challenges were discontinued at the first objective sign of reaction.
The results of statistical analyses are expressed as the median value and 25-75th percentiles. To make a statistical comparison between 2 groups, we used the Mann-Whitney U test or Fisher's exact test, and P values of <0.05 were considered statistically significant. We created probability curves using the regression analysis method after logarithmic transformation of antibody values. Sensitivity, specificity, positive predictive values, and negative predictive value were calculated. The data were statistically analyzed using the statistical software SPSS 20.0 (IBM Corporation, NY, USA).
According to the Declaration of Helsinki, the study design and risks of symptom provocation were fully explained to patients' guardians both orally and in writing, and written informed consent was obtained from all participants. Approval by the institutional review board was not necessary because in Japan, food challenge tests are within the purview of health insurance treatment.
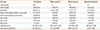
Sixty-eight children (median age, 3.9 years; 25-75th percentile, 2.1-7.2 years) underwent butter and heated milk challenges (Fig. 1, Table). Thirty-eight children tolerated butter only (butter-tolerant), 6 reacted to butter (butter-reactive), and 24 tolerated heated milk (heated milk-tolerant). Thirty-eight (86.4%) of 44 patients with a positive OFC for heated cow's milk could tolerate butter. All 6 patients with a positive OFC for butter also had a positive OFC for heated cow's milk. Four of 6 patients with a positive OFC for butter had minimal symptoms within 10 minutes and did not need to be treated. One patient developed a wheezing cough. This patient improved rapidly with administration of oral antihistamine and steroids and an inhaled bronchodilator. Another patient complained of symptoms of cough and itchiness in the throat and over the whole body. This patient's symptoms resolved rapidly after an oral antihistamine was taken (Supplementary Table 1). Patients were observed 4 hours after the symptoms disappeared, and no biphasic reaction was observed.
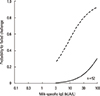
All subjects with serum milk-specific IgE <11.3 kUA/L tolerated the butter challenge (24/24); thus, both negative tests had excellent sensitivity (100%) and negative predictive value (100%). However, specificity (37.1%) and positive predictive value (13.3%) were poor. A total of 90.2% of patients with milk-specific IgE levels of 11.3 kUA/L to 100 kUA/L tolerated the butter challenge (37/41), and 60.0% of patients with milk-specific IgE levels over 100 kUA/L tolerated the butter challenge (3/5). We then created probability curves based on the results of the OFCs (Fig. 2). With a higher milk-specific IgE value, there was a higher positive probability of OFC for butter. Based on the statistical model, the positive probability of patients with a milk-specific IgE value of 100 kUA/L was 31.3%. We could not calculate milk-specific IgE values to indicate a positive predictive value over 95%. Based on this statistical model, a cut-off value of 17.8 kUA/L was proposed for identifying those who would tolerate the butter challenge (approximately 95% rate of tolerating butter). We created probability curves by patient age based on the results of the OFCs (Fig. 3). All patients aged ≤2 years passed the challenge test. Based on this statistical model, a cut-off value of 13.7 kUA/L was proposed for identifying those aged ≥2 years who would tolerate the butter challenge (approximately 95% rate of tolerating butter).
Patients with a positive result to an OFC for heated cow's milk can poorly tolerate cow's milk in any form.3 Patients were forced to accept the elimination of cow's milk from their diet, thereby decreasing their QOL. The results of this study demonstrated that most patients with a positive result to an OFC for heated cow's milk are able to safely consume raw butter. Butter is in a large number of foods, such as confectionery and seasoning. Butter made from cow's milk consists of butterfat, milk proteins, and water. Few milk proteins in butter may affect patients who are allergic to cow's milk. If patients can tolerate butter, the number of food items allowed in their diet may be increased. We recommend an OFC for butter to potentially improve the QOL of these patients.
According to some reports about the natural history of cow's milk allergy, it is difficult for patients with high specific IgE values to acquire tolerance.4,5 In the probability curve for non-heated or heated milk, the positive ratio of patients with milk-specific IgE values of 100 kUA/L approached nearly 100%.1 On the other hand, the positive ratio of patients with butter-specific IgE values greater than 100 kUA/L was only 40.0%. Based on our statistical model, the positive probability of patients with milk-specific IgE values of 100 kUA/L was 31.3%. Therefore, it is important to conduct an OFC for butter in patients with high cow's milk-specific IgE values. The milk-specific IgE value indicative of a negative predictive value of over 95% was 17.8 kUA/L, and the patients with low milk-specific IgE values may be able to safely consume butter.
There were certain limitations to this study. First, 6 patients were reactive to the butter OFC. Patients severely allergic to cow's milk might require an OFC containing less cow's milk protein than the butter OFC. Second, this study was an open, double-blind, placebo-controlled OFC; additional studies for further confirmation of the results may be warranted.
In conclusion, 38 (86.4%) of the 44 patients with positive results in the OFC for heated cow's milk were able to consume butter. Therefore, we recommend an OFC for butter be conducted for patients expected to react to heated cow's milk before conducting an OFC for heated cow's milk. The addition of butter into the diets of these milk-allergic patients will considerably improve their QOL.
Figures and Tables
Fig. 2
Fitted predicted probability curves for the outcome of challenge at a given milk-specific IgE value. The solid curve represents the results of the butter challenge test, and the dotted curve represents the results of the heated milk challenge test.
Fig. 3
Fitted predicted probability curves for challenge outcome at a given milk-specific IgE value for patients aged ≥2 years. All patients aged <2 years passed the butter challenge test.
Table
Baseline clinical characteristics of study participants
References
1. Nowak-Wegrzyn A, Bloom KA, Sicherer SH, Shreffler WG, Noone S, Wanich N, et al. Tolerance to extensively heated milk in children with cow's milk allergy. J Allergy Clin Immunol. 2008; 122:342–347. 347.e1–347.e2.
2. Kim JS, Nowak-Węgrzyn A, Sicherer SH, Noone S, Moshier EL, Sampson HA. Dietary baked milk accelerates the resolution of cow's milk allergy in children. J Allergy Clin Immunol. 2011; 128:125–131.e2.
3. Carraro S, Frigo AC, Perin M, Stefani S, Cardarelli C, Bozzetto S, et al. Impact of oral immunotherapy on quality of life in children with cow milk allergy: a pilot study. Int J Immunopathol Pharmacol. 2012; 25:793–798.
4. Wood RA, Sicherer SH, Vickery BP, Jones SM, Liu AH, Fleischer DM, et al. The natural history of milk allergy in an observational cohort. J Allergy Clin Immunol. 2013; 131:805–812.
5. Skripak JM, Matsui EC, Mudd K, Wood RA. The natural history of IgE-mediated cow's milk allergy. J Allergy Clin Immunol. 2007; 120:1172–1177.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download