Abstract
Purpose
This study evaluates offending allergens in patients with allergic rhinitis (AR) according to age that establish a minimal panel for skin prick test (SPT) allergens required to identify if a patient is sensitized.
Methods
We retrospectively analyzed SPT results according to age to determine the minimum test battery panel necessary to screen at least 93%-95% of AR patients. Allergic skin tests (common airborne indoor and outdoor allergens) were performed on 7,182 patients from January 2007 to June 2011. All patients were classified into 9 groups according to age; subsequently, we investigated offending allergens by age group.
Results
A total of 5,032 (70.1%) patients were found sensitized to at least one of the 55 aeroallergen extracts tested. The annual ranking of offending allergens was not significantly different from each other over the past 5 years. House dust mites (HDM) were the most prevalent allergens ranked from first to third for all 5 years. The allergens in the minimum test panel differed slightly among all age groups; in addition, the types of sensitized allergen sources were more diverse in the older versus younger age group. HDM covered a larger proportion of the sensitized allergens in the younger age group versus the older age group. Testing with 5 allergens (Dermatophagoides farinae, Tetranychus urticae, oak, mugwort and cockroach) adequately identified over 90% of the sensitized patients.
An investigation of the main offending allergen is essential to treat allergic rhinitis (AR). Offending allergens change steadily in accordance with the surrounding atmosphere; in addition, their distribution also differs by region. The continuous investigation and monitoring of offending allergens is a prerequisite for the treatment of AR.
A skin prick test (SPT) is a standard method for the diagnosis of IgE-mediated allergic disease and routinely performed to identify allergens in a clinical setting. However, the current SPT panel varies among hospitals and most allergic disease clinics perform the SPT with 55 allergens irrespective of patient age. There is no current age dependent standard test panel in Korea. The SPT with 55 allergens is problematic in terms of patient inconvenience and cost, especially when the subjects are preschool children. The application of limited number of allergens could be possible for patients since the rate of sensitization to some allergens is quite low and differs based on age. This is an important concept when an epidemiologic study is required. Knowledge of the composition of the minimally required SPT panel and the difference of SPT sensitization dependent on age is an essential factor for a reliable epidemiologic survey.
A recent study of the Global Allergy and Asthma European Network demonstrated the sensitization patterns of different inhalant allergens in patients across Europe and the minimum test battery of inhalant allergens needed for an epidemiological study.1-3 Other studies similar to population-based epidemiologic studies show that a limited number of allergens identified the majority of sensitized subjects in patients-based studies.4
This study evaluates the annual distribution of offending allergens in AR patients over a 5 year period and documents the most prevalent offending allergens based on age. Based on the results, the authors suggest the basic optimal required items for a simple screening SPT tailored to individual age and epidemiological study.
From January 2007 to June 2011, data, including age, sex, and sensitized allergens, were obtained from subjects who performed SPT for respiratory symptoms at the Allergy and Clinical Center Laboratory of Seoul National University Hospital. This study utilized the archived data from 7,182 AR patients (3,761 men and 3,421 women) aged 5 to 88 years old. We analyzed common indoor and outdoor airborne allergens in all patients according to age groups: 0-6 years, 7-12, 13-19, 20-29, 30-39, 40-49, 50-59, 60-69, and over 70 years old.
All subjects that presented respiratory symptoms suggestive of AR underwent SPT with a standard panel of 55 allergen extracts. A battery of eight airborne allergens was used for the skin test (Allegropharma, Reinbek, Germany): House dust mites (HDM) (Dermatophagoides farinae [Df], Dermatophagoides pteronyssinus [Dp], Tyrophagus putrescentiae [Tp], and Tetranychus urticae [Tu]), outdoor mold mixture (Alternaria, Cladosporium, Fusarium, Aspergillus niger, and Candida albicans), indoor mold mixture (Aspergillus fumigates, Mucor mucedo, Neurospora sitophila, and Penicillium notatum), animal dander (Cat, Dog, Rat, Chicken, and Rabbit), cockroach (German cockroach, and American cockroach), tree pollen mixture 1 (Alder, Hazel, Popular, Elm, Willow tree, Ash, and Elder), tree pollen mixture 2 (Birch, Beech, Oak, Plane tree, and Japanese cedar), grass pollen mixture (Velvet, Orchard, Rye, Timothy, Kentucky, Meadow, Nettle, and Bermuda), weeds (Ragweed, Mugwort, Japanese Hop [Hop J], Chrysanthemum, Dandelion, Golden Rod, Plantain and Latex), and 10 mg/mL histamine phosphate as positive control and 0.9% saline as negative control. SPTs were evaluated 15 min after application and interpreted as 3+ when the mean wheal diameter was identical to the histamine control and 2+ when the mean wheal diameter was 50% of the histamine control. A positive response was defined as more than 2 or more positive (2+, 3+, 4+) to the allergen tested. Positive response to at least one of the allergens was accepted as the presence of sensitization.
First, most prevalent allergens according to age were defined using frequency and percentage. A systematic conditional approach then classified the allergens from the highest prevalence of sensitization to the lowest. The second highest allergen was identified through elimination of the subjects sensitized to the previous allergen.1 The prevalence of sensitization was calculated for each age group. The combination of allergens, which identified at least 93%-95% of the sensitized subjects, was defined as the optimal SPT panel. This procedure was performed repeatedly with each group classified by age: ≤6 years, 7 to <12 years, 13 to <19 years, 20 to <29 years, 30 to <39 years, 40 to <49 years, 50 to <59 years, 60 to <69 years, and ≥70 years. A SPSS 17.0 software (Chicago, IL, USA) was used for the statistical analysis.
To evaluate the change of the trend of offending allergens, a comparison of the year 2007 and the year 2011 showed that the positive rates of allergens increased slightly in most allergens (Fig. 1). However, the overall ranking of each allergen was similar between the year 2007 and the year 2011 (except for beech and Hop J pollens). In addition, there was a remarkable increase in the positive rate of beech/Hop J as a seasonal allergen and cockroach as perennial allergens between the year 2007 and the year 2011 (Fig. 2).
The overall positive response rate was 70.1% (5,032/7,182) and all sensitized subjects showed a positive response to at least 1 aeroallergen. The number of patients according to age group was as follow: group 0-6 years, n=268 (3.7%); 7-12 years, n=673 (9.3%); 13-19 years, n=660 (9.1%); 20-29 years, n=1,032 (14.3%); 30-39 years, n=735 (10.2%); 40-49 years, n=550 (7.6%); 50-59 years, n=622 (8.6%); 60-69 years, n=356 (4.8%); and over 70 years, n=136 (1.8%) (Table 1). The prevalence of sensitization to common allergens increased with age, from group 0-6 years to group 13-19 years, and then decreased progressively (Fig. 3). A maxim sensitization rate was observed in the age group 13-19 years, with 92.8% of subjects sensitized to at least 1 aeroallergen. The sensitization rate then decreased to 34.7% in the age group over 70 years. The sensitized allergens were different according to age group. HDM showed the highest prevalence in all age groups. Among HDM, Df was the most prevalent mite followed by Dp in all age groups. The prevalence of sensitization to Tu and Tp were lower than that to Df or Dp throughout the age groups; however, the overall percentages of the four mites gradually converged on a similar percentage at over 60 years of age.
Dog hair-dander was the most prevalent allergen, followed by cat hair-epithelium, for animal allergens and showed a higher incidence than cockroach allergens. Sensitization to animal allergens peaked in the ages of 20-29 years and then deceased with age. In addition, tree pollen was more prevalent than grass or weed allergens among pollen allergens. The sensitization rate peaked in the ages of 20-29 years and then the overall percentage of sensitization fell sharply at over 60 years of age. In addition, mold allergens increased steadily in the ages of 20-29 years and then steeply decreased at over 40 years of age (Table 1).
Table 2 and Table 3 show the minimum test battery panel to reach a detection rate of 93%-95% of sensitized persons for all or different age groups. The N column number in Table 2 and Table 3 (calculated from Table 1) represents the number of patients with a positive response to that allergen. The "Left" column can be calculated by a subtraction of the positive response number from the previous left number; hence, the remnant patient number (missed by the allergen combination) is serially added. A combination of the top 4 allergens in Table 2 provides a total of 503 patients marked as SPT negative, even though these patients were initially classified as positive.
In the whole generation, 5 allergen extracts (Df, Tu, oak, mugwort and cockroach G) were sufficient to detect sensitizations (Table 2). With only 4-allergen extracts (Df, Tu, oak and mugwort), the detection rate reached the level of 90.0%; however, the allergens in the minimum test panel differed slightly among all age groups. A total of 5 to 7 allergen extracts were the minimum number required to reach a detection rate level of 93%-95% and were similar in each age group (Table 3). In addition to the number, the kinds of allergens extracts were similar. A comparison of the content of the SPT panel of the whole generation showed that the age group 40-49 was composed of the exact same allergen extracts. In addition, the type of allergen was identical except for one allergen in the age group 50-59 years. The type of sensitized allergen source was more diverse in the older age group than in the younger group. This phenomenon resulted in the increment of the numbers of allergens in the optimal panel that represent a detection rate of 93%-95% of sensitizations.
Table 4 shows the detection missing rate where the optimized test panel (Table 2) was applied to all age groups when the allergen extracts ranked from the first to seventh. The low was 2.4% for the age group of 20-29 years and the high 10.4% for the age group of 60-69 years. Table 5 shows the detection rate differences between combinations of 2 allergens according age groups. A combination of Df and Tu allergens detected more sensitizations than Df and Dp.
This study showed that the type of sensitized allergens differ according to age. We found that the majority of patients was sensitized to indoor aeroallergens such as house dust mites and animal dander. The prevalence of sensitization peaked at 13-19 years regardless of the type of allergens and then decreased progressively with age. The sensitization pattern did not change according to different years. The similarity of the year variance according to age provides an idea of the simplification of the allergens used in the SPT as possible. This study suggests that SPT with a specialized allergen combination tailored for each age group as a cost effective screening of AR.
In present study, we found that the offending allergens differed according to age groups. The most common aeroallergen was HDM as expected. Especially, among the mites, Df ranked first in the allergen extract used in the panel of all ages and Tu was the second important mite in the panel of all ages except the age group under 6 years. However, it is notable that Dp was not a major impact in this study. Df, slightly more prevalent in all age groups, was used as a screening allergen because many patients were sensitized to both. Nearly all patients sensitized to Dp showed a positive response to Df; however, the same was not true in reverse.
The proportion of sensitization to the Tu increased gradually among HDM; however, the other mites decreased with age (Table 1). Unlike the Dermatophagoides species, Tu was identified not to share a common positivity relatively with other mite species. Table 5 shows the detection rate differences between the combinations of 2 allergens according to age group. The combination of Df and Tu allergens could detect more sensitizations than Df and Dp. The effectiveness of the Df and Tu union was more obvious in the advanced age group; subsequently, most HDM sensitization was covered in the majority of the groups by adding Tu to the Df.
HDM sensitization (Df) was up to 87.0% in the 13 to <19 age group; however, the importance of HDM decreased to the 55.3% level in the 60 to <69 age group (Table 3). A decline of the proportion of sensitization to HDM led to the diversity of the composed offending allergens in the SPT panel according to the age group. The predominant allergen HDM (as the first applying factor) allowed the simplification of the number of allergen extracts (required to cover most sensitization) at a rate of 93%-95% in the test panel. The phenomena reflect that HDM are the main offending allergens in Korea compared to standard SPT panels evaluated in Europe where pollens are the most prevalent allergen.5,6
Pollens are usually the second most important allergen factor to cover many of the sensitizations among all age groups. Tree pollen oak was more commonly sensitized in the younger age group; however, weed pollen mugwort was more sensitized in the older age group. This study performed the screening test with a tree mixture. The number of allergen extracts required for the screening test should decrease more easily with a tree mixture usage; however, this did not significantly affect the total number. Many sensitizations could be identified in the majority of the diverse age groups with only HDM plus tree pollen (Table 3).
Weed sensitization reached 24.4% in our study. Among the weed pollens, mugwort and were prevalent allergens listed on the SPT panel in the majority of the age category; however, (even though we used the grass mixture) grass pollens were not incorporated in the SPT panel except for one age group over the age of 70. This suggests grass pollens are inappropriate as screening allergens.
In terms of cockroach, the positive rate peaked and maintained a similar lifetime rate in subjects over the age of 20 years old. Cockroach could not get a place in the SPT panel in subjects under 19 years of age; however, it ranked high at over 20 years of age. Previous studies reported an 11.4%-30% sensitization to cockroach.7-9 In our study, the overall prevalence of cockroach (German or American type) according to each year eventually increased between the years of 2007 and 2011 (Fig. 2). This reflects the recent trend of cockroach playing a major role as an important allergen in urban areas. In addition, cockroach should be listed the SPT panel due to its expected importance in subjects over 20 years of age. A total of 30% of AR patients were sensitized to cockroach and our study results suggest that cockroach should be considered an important antigen in AR in Korea.7
Animal dander (especially dog) are incorporated into the children and adolescent age group combination because sensitization to dog or cat were more prominent in younger age populations compared to other age populations. In addition, animal dander is no longer an important allergen in subjects over 50 years of age. The number of dog owners in Korea is higher than that of cat owners and explain the difference in findings compared to the Turkish study that ranked cat allergen as an important allergen.10
Testing with allergen combinations of Df, Tu, oak, mugwort, and cockroach G identified over 90% of the sensitized patients of all ages for AR screening in the epidemiologic study. The optimized SPT result can significantly reflect the age-specific allergens character since the majority of the study population belonged to the 20-39 year age group; subsequently, it would be good to customize a supplementary allergens option plus the minimally required SPT panel in regards to a specific age bracket. For instance, animal dander, especially dog, is a recommended allergen incorporated in the combination for children and cat is specifically recommended for subjects 20-49 years old because sensitization to dog is shown more prominently in that age range. The positive rate for cockroach peaked and maintained a similar rate in subjects more than 20 years old. For pollen allergens, hop J is a recommended and necessary item for subjects over 20 years of age and mugwort for subjects over 30 years of age. Oak should be considered as a solitary allergen (among tree pollen) for all ages when SPT is not performed with a pollen mixture allergen even though the importance was weakened by HDM. In addition, if a study is to be performed on a 50-59 age group, researchers should be cautious in the selection of optimal allergens due the diversity of allergen sensitization.
A possible limitation of this study is that the results do not reflect the regional characteristics; subsequently, it is recommended that some region-specific allergens should be added to the SPT panel.
In conclusion, a limited number of allergens should be sufficient for screening AR patients at around 93%-95% of sensitized patients. Even though only 5 allergens proved adequate for the epidemiologic study, we should consider the increase of missing rate in elderly subjects.
Figures and Tables
Fig. 1
Annual positive rate of offending allergens. The comparison of year 2007 and year 2011 to evaluate the change of the trend of offending allergens; the positive rates of allergens increased slightly in most allergens.
Fig. 2
Annual variability of offending allergens between 2007 and 2011 year. The overall allergen ranking was similar between year 2007 and year 2011 (except for beech and hop J pollens). In addition, there was a remarkable increase in the positive rate of beech as a seasonal allergen and cockroach/hop J as perennial allergens between year 2007 and year 2011. D.f, Dermatophagoides farinae; D.p, Dermatophagoides pteronyssinus.
Fig. 3
The prevalence of sensitization peaked in young adults (regardless of the allergen) and diminished with age. The prevalence of sensitization to common allergens increased with age, from group 0-6 years to group 13-19 years, and then decreased progressively.
Table 1
Distribution of the frequencies of sensitization for each allergen used in skin prick test by age group and in the whole study population, % (n)

Table 2
The offered test panel for all age groups and the percent of sensitization by given aeroallergen extracts
Table 3
The offered test panel for different age groups and the percent of sensitization by given aeroallergen extracts

Table 4
The detection missing rate according to the age groups
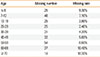
| Age | Missing number | Missing rate |
|---|---|---|
| ≤6 | 25 | 9.30% |
| 7-12 | 48 | 7.10% |
| 13-19 | 25 | 3.80% |
| 20-29 | 25 | 2.40% |
| 30-39 | 31 | 4.20% |
| 40-49 | 32 | 5.80% |
| 50-59 | 54 | 8.60% |
| 60-69 | 37 | 10.40% |
| ≥70 | 14 | 10.30% |
The detection missing rate was around 2.4% - 10.4 % when the allergen extracts from top to 7th in the offered test panel of table 2 were applied to all age groups.
Table 5
Differences of detection rate between combinations of 2 allergens according to the age

References
1. Bousquet PJ, Burbach G, Heinzerling LM, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, Bousquet-Rouanet L, Demoly P, Bresciani M, Bruno A, Gjomarkaj M, Canonica GW, Darsow U, Durham S, Fokkens WJ, Giavi S, Gramiccioni C, Papadopoulos NG, Haahtela T, Kowalski ML, Magyar P, Muraközi G, Orosz M, Röhnelt C, Stingl G, Todo-Bom A, von Mutius E, Wiesner A, Wöhrl S, Bousquet J, Zuberbier T. GA2LEN skin test study III: minimum battery of test inhalent allergens needed in epidemiological studies in patients. Allergy. 2009; 64:1656–1662.
2. Bousquet PJ, Hooper R, Kogevinas M, Jarvis D, Burney P. Number of allergens to be tested to assess allergenic sensitization in epidemiologic studies: results of the European Community Respiratory Health Survey I. Clin Exp Allergy. 2007; 37:780–787.
3. Heinzerling LM, Burbach GJ, Edenharter G, Bachert C, Bindslev-Jensen C, Bonini S, Bousquet J, Bousquet-Rouanet L, Bousquet PJ, Bresciani M, Bruno A, Burney P, Canonica GW, Darsow U, Demoly P, Durham S, Fokkens WJ, Giavi S, Gjomarkaj M, Gramiccioni C, Haahtela T, Kowalski ML, Magyar P, Muraközi G, Orosz M, Papadopoulos NG, Röhnelt C, Stingl G, Todo-Bom A, von Mutius E, Wiesner A, Wöhrl S, Zuberbier T. GA(2)LEN skin test study I: GA(2)LEN harmonization of skin prick testing: novel sensitization patterns for inhalant allergens in Europe. Allergy. 2009; 64:1498–1506.
4. Bousquet PJ, Chatzi L, Jarvis D, Burney P. Assessing skin prick tests reliability in ECRHS-I. Allergy. 2008; 63:341–346.
5. Burney PG, Luczynska C, Chinn S, Jarvis D. The European Community Respiratory Health Survey. Eur Respir J. 1994; 7:954–960.
6. Zureik M, Neukirch C, Leynaert B, Liard R, Bousquet J, Neukirch F. European Community Respiratory Health Survey. Sensitisation to airborne moulds and severity of asthma: cross sectional study from European Community Respiratory Health Survey. BMJ. 2002; 325:411–414.
7. Eun YG, Kim SW, Lee IY, Cho JS. Cockroach allergic rhinitis in the urban area in Korea: sensitivity and diagnosis. Korean J Otolaryngol-Head Neck Surg. 2004; 47:747–750.
8. Bang JH, Kim YJ, Shin HS, Lee BJ. Clinical analysis of allergic rhinitis in Seoul. Korean J Rhinol. 1996; 3:130–134.
9. Ko YH, Park SY, Lee JH, Koo GJ, Koo SK, Lee SH, Kim SW. A clinical statistics on the offending allergens of allergic rhinitis. Korean J Otolaryngol-Head Neck Surg. 1998; 41:42–47.
10. Şahiner UM, Civelek E, Yavuz ST, Büyüktiryaki AB, Tuncer A, Şekerel BE. Skin prick testing to aeroallergen extracts: what is the optimal panel in children and adolescents in Turkey? Int Arch Allergy Immunol. 2012; 157:391–398.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download