Abstract
Asthma is a chronic disease causing psychological stress which leads to the activation of hypothalamus-pituitary-adrenal axis. The purpose of this study is to compare morning salivary cortisol levels in persistent asthma patients according to their disease severities and control status. Total 206 adult asthma patients were recruited from four university hospitals. Spirometry, questionnaire of Asthma Quality of Life (AQOL) and Asthma Control Test (ACT) were completed, and saliva samples were collected prospectively to measure morning cortisol level. The mean patient age was 56.5±15.3 years with mean asthma duration of 9.1±11.1 years. Sixty five patents (31.6%) were classified as mild persistent asthma, and 141 patients (68.4%) were classified as moderate persistent asthma according to the Expert Panel Report 3. The mean predicted FEV1 was 88.8%±18.4%, and the methacholine PC20 was 9.6±8.5 mg/mL in all study population. The mean ACT score for all patients was 19.9±3.6, and there were 71 (34.5%) patients in poorly controlled and 135 (65.5%) in well controlled asthma. The poorly controlled asthma patients were characterized by significantly lower FEV1 (84.6%±17.6% vs 91.1%±18.5%, P=0.018), lower AQOL scores (46.0±13.9 vs 73.8±26.3, P<0.001), and lower salivary cortisol levels (0.14±0.08 vs 0.18±0.11 µg/dL, P=0.04) compared to well controlled asthma. The ACT score was significantly related to salivary cortisol levels (P=0.034) after adjusting for age. There was no significant difference in salivary cortisol levels (0.17±0.12 vs 0.16±0.08, P=0.725) when analyzed according to the dose of used corticosteroid and lung function. Asthma control status affects morning salivary cortisol level. Measuring the morning salivary cortisol level might be a simple and new way to assess asthma control status.
Asthma is one of the most common chronic diseases causing psychological stress which can lead to depression or anxiety, but psychological effect caused by asthma depends on disease duration.1 In airway inflammatory disease, acute stress causes a decrease in the forced expiratory volume in one second (FEV1), an increase in exhaled nitric oxide (NO), and a decrease in inflammatory cell numbers in bronchoalveolar lavage fluid (BALF), whereas chronic stress improves lung function and increases inflammatory cell numbers in BALF.2
Stress activates the hypothalamus-pituitary-adrenal axis which enhances cortisol secretion. Although serum cortisol levels can be measured, an effort is being made to develop a non-invasive method and salivary cortisol, that correlates well with serum cortisol levels,3 has widely used.
Asthmatic patients have lower morning salivary cortisol levels compared to healthy controls regardless of the use of inhaled corticosteroids (ICS).4 However, it is unknown whether asthma severity and control status affect the cortisol levels in patients with persistent asthma. Therefore, in this study the morning salivary cortisol levels were compared in patients with persistent asthma according to their disease severities and control status.
Total 206 adults with persistent asthma were recruited from four university hospitals in South Korea. The patients were included if they had more than 60% of the predicted FEV1 and were diagnosed with asthma based on American Thoracic Society guidelines, including presence of typical asthma symptoms for more than 6 months, airway hyper-responsiveness to methacholine, and reversible airway obstruction, and the patients were classified as moderate persistent asthma according to the Expert Panel Report 3. Spirometry, the Asthma Quality of Life (AQOL) questionnaire, and Asthma Control Test (ACT) were completed in all study subjects.5,6 Total used ICS doses were also included in this study after adjusting corticosteroid potency. Poorly controlled asthma was defined as an ACT score ≤19 (group I), while well-controlled asthma was defined as an ACT score ≥20 (group II).7 Saliva samples were collected prospectively on 3 consecutive days when patients awoke to measure salivary cortisol levels. The free salivary cortisol level was determined using a High Sensitivity Salivary Cortisol Enzyme Immunoassay Kit (Salimetrics LLC, State College, PA, USA), according to the manufacturer's instructions. A Mann-Whitney U-test was used to determine differences between the 2 groups; a general linear model was used to evaluate the effect of ACT on salivary cortisol levels with age as a covariate. Informed consent was obtained from each patient. The study protocol was approved by the ethics committee of each university hospital.
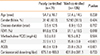
Female patients (59.7%) were predominant in this study. The mean patient age was 56.5±15.3 (range 20-84) years and mean asthma duration was 9.1±11.1 years. The mean FEV1 was 88.8%±18.4% of the predicted value, and the methacholine PC20 was 9.6±8.5 mg/mL in all subjects. Sixty five patents (31.6%) had mild persistent asthma, and 141 patients (68.4%) had moderate persistent asthma according to Expert Panel Report 3.8 The mean ACT score for all patients was 19.9±3.6 (range 7-25), and there were 71 (34.5%) patients in poorly controlled group and 135 (65.5%) in well controlled group decided by ACT score. The patients in poorly controlled state were characterized by a significantly lower FEV1 value (84.6%±17.6% vs 91.1%±18.5% pred., P=0.018) and lower AQOL scores (46.0±13.9 vs 73.8±26.3, P<0.001) (Table 1). There were no significant differences in age, sex, asthma duration and methacholine PC20 level between two groups (P>0.05, respectively). The mean salivary cortisol level was 0.17±0.10 (range 0.015-0.672) µg/dL in all study subjects, but was significantly lower in poorly controlled group than in well controlled group (0.14±0.08 vs 0.18±0.11 µg/dL, P=0.048), as shown in Fig. 1. The ACT score was significantly related to salivary cortisol levels (P=0.034) after adjusting for age (data not shown). One hundred ninety four patients (94.2%) had taken ICS during study period. The adjusted dose of beclomethasone dipropionate ranged about from 150 to 2,000 µg/day. However, there was no significant difference in the salivary cortisol level when analyzed according to the dose of corticosteroid used, and lung function (Fig. 2 A and B).
Several studies have reported lower cortisol levels or a blunted circadian rhythm in asthma patients compared to non-asthmatic controls in pediatric patients.4 However, cortisol levels between children and adults were quite different.9 To the best of our knowledge, this is the first study to analyze salivary cortisol levels according to asthma control status in adult asthma patients. Main finding of this study is significantly lower salivary cortisol levels in poorly controlled patients defined by ACT than in well controlled patients. The ACT score reflects the individual patient's perception of his or her symptoms that leads to psychological stress. It is easily presumed that poorly controlled asthma patients with continuous respiratory symptoms can give rise to chronic psychological stress. For example, an asthma exacerbation can induce post-traumatic stress that is closely associated with patients' perceptions of their asthma symptoms,10 and in other disease, women with chronic pelvic pain had significant lower salivary cortisol levels regardless of their pain intensity.11 These findings suggested that poorly controlled asthma might induce chronic stress and decrease morning salivary cortisol level in adult asthmatic patients.
A previous study showed that asthma patients taking moderate- to high-dose ICS had lower salivary cortisol levels than healthy controls in children without considering their asthma control status.4 In the present study, the salivary cortisol levels in adult patients did not differ significantly according to the use or dose of ICS, but were different significantly according to asthma control status. This discordance between children and adult patients might be explained by age of study population, because cortisol levels depend on age.9
Salivary cortisol levels vary greatly between individuals and confounding factors such as smoking and adherence to the saliva collection protocol may change the results. In the present study, we collected saliva samples prospectively for 3 consecutive days to eliminate the disadvantage of a cross-sectional study design in more than 200 patients. Although subsequent prospective studies with a larger cohort are needed to demonstrate that obtaining salivary cortisol levels will help with management of asthmatic patients, measurement of salivary cortisol level is a simple and objective non-invasive procedure that can be used in a clinical setting, because we have few objective tools for monitoring control status in the management of adult asthma.
In conclusion, asthma control status affects morning salivary cortisol level. Measuring the morning salivary cortisol level might be a new way to assess asthma control status in adult asthmatics.
Figures and Tables
 | Fig. 1Morning salivary cortisol levels according to asthma control status. Poorly controlled asthma was defined as an ACT score ≤19, and well-controlled asthma was defined as an ACT score ≥20. |
 | Fig. 2Correlation analysis between salivary cortisol levels and equivalent corticosteroid dose per day (A) and percentage of predicted FEV1 (B). Equivalent corticosteroid doses were adjusted to beclomethasone dipropionate. |
Table 1
Clinical characteristics of the study subjects according to asthma control status assessed by ACT score
References
1. Oraka E, King ME, Callahan DB. Asthma and serious psychological distress: prevalence and risk factors among US adults, 2001-2007. Chest. 2010; 137:609–616.
2. Forsythe P, Ebeling C, Gordon JR, Befus AD, Vliagoftis H. Opposing effects of short- and long-term stress on airway inflammation. Am J Respir Crit Care Med. 2004; 169:220–226.
3. Ahn RS, Lee YJ, Choi JY, Kwon HB, Chun SI. Salivary cortisol and DHEA levels in the Korean population: age-related differences, diurnal rhythm, and correlations with serum levels. Yonsei Med J. 2007; 48:379–388.
4. Bakkeheim E, Mowinckel P, Carlsen KH, Burney P, Lødrup Carlsen KC. Reduced basal salivary cortisol in children with asthma and allergic rhinitis. Acta Paediatr. 2010; 99:1705–1711.
5. Lee EH, Kim SH, Choi JH, Jee YK, Nahm DH, Park HS. Development and evaluation of an Asthma-Specific Quality of Life (A-QOL) questionnaire. J Asthma. 2009; 46:716–721.
6. Hwang EK, Jin HJ, Nam YH, Shin YS, Ye YM, Nahm DH, Park HS. The predictors of poorly controlled asthma in elderly. Allergy Asthma Immunol Res. 2012; 4:270–276.
7. Thomas M, Kay S, Pike J, Williams A, Rosenzweig JR, Hillyer EV, Price D. The Asthma Control Test (ACT) as a predictor of GINA guideline-defined asthma control: analysis of a multinational cross-sectional survey. Prim Care Respir J. 2009; 18:41–49.
8. Busse WW, Lemanske RF Jr. Expert panel report 3: moving forward to improve asthma care. J Allergy Clin Immunol. 2007; 120:1012–1014.
9. Gröschl M, Rauh M, Dörr HG. Circadian rhythm of salivary cortisol, 17alpha-hydroxyprogesterone, and progesterone in healthy children. Clin Chem. 2003; 49:1688–1691.
10. Chung MC, Rudd H, Wall N. Posttraumatic stress disorder following asthma attack (post-asthma attack PTSD) and psychiatric co-morbidity: the impact of alexithymia and coping. Psychiatry Res. 2012; 197:246–252.
11. Petrelluzzi KF, Garcia MC, Petta CA, Grassi-Kassisse DM, Spadari-Bratfisch RC. Salivary cortisol concentrations, stress and quality of life in women with endometriosis and chronic pelvic pain. Stress. 2008; 11:390–397.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download