Abstract
Purpose
Mycoplasma pneumoniae pneumonia (MP) is associated with the exacerbation, timing, and onset of asthma. The goal of this study was to elucidate the impact of MP on eosinophil-related hyper-reactive amplification in atopic children.
Methods
We studied 48 patients with MP (26 atopic, 22 non-atopic), between 3 and 12 years of age. Serial changes in blood eosinophil counts, serum interleukin-5 (IL-5), and serum eosinophil cationic protein (ECP) levels were measured in atopic and non-atopic children with MP upon admission, recovery, and at 2 months post-recovery. Serum IL-5 and ECP levels were measured by enzyme-linked immunosorbent assays; eosinophil counts were measured using an autoanalyzer.
Results
Serial changes in serum IL-5, ECP, and total eosinophil counts were significantly higher in atopic patients, relative to non-atopic controls (P≤0.001). Serum IL-5 and ECP levels were significantly higher in atopic patients at all three time points tested, while eosinophil counts were higher in the clinical recovery and follow-up phases, but not in the acute phase. Furthermore, among atopic patients, serum ECP levels were significantly higher in the recovery and follow-up phases than in the acute phase.
Conclusions
The present study demonstrated significant differences in eosinophil counts, serum IL-5, and serum ECP levels between atopic and non-atopic children with MP at admission, recovery, and 2 months after clinical recovery. These outcomes are suggestive of eosinophil-related hyperreactivity in atopic children, with this status maintained for at least 2 months after MP.
Mycoplasma pneumoniae has long been recognized as a cause of primary atypical pneumonia, particularly among children. This microorganism accounts for 7 to 40% of all community-acquired pneumonias in children 3 to 15 years of age, with a lower incidence in children under the age of 3 years. Other respiratory illnesses, including tracheobronchitis, bronchopneumonia, pharyngitis, sinusitis, croup, and bronchiolitis have also been associated with M. pneumoniae. In contrast to the acute, short-lived epidemics of some respiratory viral agents, M. pneumoniae is endemic to large communities, with outbreaks occurring every 4 to 7 years.1,2,3 According to the Korea Centers for Disease Control and Prevention, the most recent outbreak of Mycoplasma pneumoniae pneumonia (MP) in Korea lasted from late summer 2010 to the fall of 2011, with peak positivity rates in community-acquired pneumonia ranging from 23.6% in October 2010 to 62.5% in September 2011.4
In addition to its role as a cause of community-acquired pneumonia, M. pneumoniae is also known to trigger acute asthmatic exacerbations.5,6,7 M. pneumoniae has been linked to the development of chronic infections, and may contribute to the persistence and severity of asthmatic symptoms.8 Furthermore, these persistent infections can result in decreased expiratory flow rates and increased airway hyperresponsiveness in individuals without asthma, consistent with a role for M. pneumoniae as an asthmatic trigger.9 Similar effects were observed in a murine study of MP, in which pulmonary structural abnormalities suggestive of airway hyperreactivity, airway obstruction, and histological inflammation were more frequent 1 to 2 years after respiratory M. pneumoniae infection.10 This suggests that mediators associated with airway hyperreactivity could provide information regarding the cause of these structural abnormalities after M. pneumoniae respiratory infection. Although clinical manifestations of pneumonia disappear within a few months following recovery from an M. pneumoniae infection, mediators of airway hyperreactivity may continue to be released into the circulation long after the infection has been cleared.
Allergic reactions are characterized by an infiltration of T helper type 2 (Th2) cells into affected tissues. Upon exposure to an allergen, these cells expand rapidly, and begin secreting large amounts of IL-4, IL-5, and IL-13, resulting in IgE synthesis and eosinophilia. IL-5 is a potent mediator of eosinophil activation, and along with eosinophil cationic protein (ECP), plays a key role in airway hyperresponsiveness.11
Children with acute M. pneumoniae infection and wheezing exhibited higher serum IL-5 concentrations than those with asymptomatic acute infection without wheezing, suggesting the association of IL-5 with airway hyperresponsiveness.12 Similar increases in serum IL-5 levels have also been seen in children with atopic MP.13 Furthermore, eosinophilia has been reported in up to 44% of children with M. pneumoniae infections, suggesting that potent Th2-like immune responses are common in MP. Taken together, these and other studies suggest a mechanism by which activated eosinophils in the airway undergo degranulation leading to injury of the bronchial epithelium, and induction of bronchial hyperreactivity.14,15
In addition to IL-5, ECP is also a key mediator of eosinophil activation. Yamashita and colleagues reported that the serum concentrations of ECP in children with M. pneumoniae infections were higher than those of healthy controls. These elevated ECP levels may be associated with damage to the respiratory epithelium and accelerated hypersensitivity in the respiratory system, resulting in a chronic, persistent cough that can last several months.16,17
The aim of this study was to investigate serial changes in blood eosinophil counts, serum IL-5, and serum ECP levels in atopic and non-atopic children with MP at admission, recovery, and 2 months after recovery. These findings should help to elucidate the role of MP in eosinophil-related hyperreactive amplification in atopic children.
Forty-eight patients between 3 and 12 years of age were included in this study. Patients were admitted to the Department of Pediatrics at Hanyang University Guri Hospital, Gyeonggi-do, Korea with a diagnosis of MP between October 2011 and June 2012. All children received a physical examination, and were evaluated regarding their personal and family history of allergic diseases. Routine laboratory tests were performed, including measurement of total serum IgE. Patients were then divided into 2 groups: those exhibiting elevated serum IgE levels in combination with a personal or family history of allergic diseases (group 1, n=26), and those who had normal serum IgE levels and no personal or family history of allergic diseases (group 2, n=22). All study protocols and patient consent forms were approved by the Institutional Review Board of Hanyang University Guri Hospital, and informed written consent was obtained from all parents and/or participants.
MP was diagnosed based on clinical findings (such as fever, cough, dyspnea, and crackles), radiological findings (such as chest infiltrates and consolidative lesions), and changes in anti-mycoplasma antibody titers. Anti-mycoplasma antibody titers were measured on admission, at clinical recovery, and on follow-up visits 2 months later by the microparticle agglutination method using a commercial kit (Serodia-Myco II, Fujirebio, Tokyo, Japan). Each phase was defined as follows; patients at admission phase had acute typical symptoms and signs of pneumonia and laboratory findings, patients at recovery phase had clinically improving symptoms, and patients on follow-up visits 2 months later had no obvious symptoms of pneumonia after recovery. Positive titers were defined as ≥1:160 at admission or a titer ≥fourfold the admission titer during the symptomatic recovery phase. The time between admission and symptomatic recovery ranged from 7 to 10 days. Clinical recovery was defined as absence of asthmatic symptoms and normal physical examination. We performed viral-specific polymerase chain reaction (PCR) analysis of nasopharyngeal secretions, and excluded patients with positive results. Nasopharyngeal specimens were independently screened for the presence of common respiratory viruses, including influenza viruses, parainfluenza viruses, human coronaviruses, human rhinoviruses, human metapneumoviruses, human adenoviruses and respiratory syncytial viruses, by reverse transcription-PCR using a commercial kit (Seeplex RV 12 ACE Detection, Seegene, Seoul, Korea).
Serum IgE levels at admission were measured using an IRMA kit (Diagnostic Products Co., Los Angeles, CA, USA). A value of 100 IU/mL was used as the threshold for discriminating between allergic and non-allergic children.18 Patients with serum IgE levels ≥100 IU/mL were considered at risk for asthma.19
Venous blood was taken from each subject, centrifuged at 1,000×g for 10 minutes at 4℃, and stored at -70℃. Serum IL-5 levels were measured using a commercial enzyme-linked immunosorbent assay (ELISA) (DBD Inc., San Diego, CA, USA), according to the manufacturer's instructions. The detection limit was 2 pg/mL. Peripheral blood eosinophil counts were measured with an automated hematology analyzer (Coulter Counter STKS, Beckman Coulter, Fullerton, CA, USA) using blood samples collected in tubes containing EDTA. Serum ECP was measured using a commercial fluoroimmunoassay kit (PharmaciaECP UniCAP System FEIA; Pharmacia Diagnostics, Uppsala, Sweden), with a detection limit of 2 µg/L; a level of ≥16 µg/L was considered abnormal.20 IL-5, ECP, and peripheral blood eosinophils were assayed at admission, recovery, and at the follow-up visit 2 months later.
Data were analyzed using the SPSS statistical package (SPSS Inc., version 18.0, Chicago, IL, USA). Differences in the sex ratio between 2 groups were analyzed using the χ2 test. Continuous variables were summarized as means±standard deviation (SD); values for serum total IgE were expressed as geometric means (range of 1 SD). Normally distributed parameters such as age were compared by Student's t-tests; the Mann-Whitney U test was used for serum total IgE, which was not normally distributed. Repeated-measure analysis of variance was used to evaluate differences in the serial changes of serum IL-5, serum ECP, total eosinophil counts, and anti-mycoplasma antibody titers between the two groups. In each phase, differences between the 2 groups in serum IL-5, serum ECP and total eosinophil counts were analyzed by Student's t-test. Comparisons between the three phases within each group were conducted by one-way analysis of variance and the Kruskal-Wallis test, combined with the appropriate post hoc Tukey multiple comparison test and Mann-Whitney U-test, respectively. P values ≤0.05 were considered to indicate significance.
The characteristics of the subjects are shown in Table 1. No significant differences were observed in the age or sex of the 2 groups. A significantly higher geometric mean serum total IgE level was found in group 1 (atopic patients). Within each group, significant differences in anti-mycoplasma antibody titers were observed among the 3 phases; however, these changes were not statistically significantly between groups.
Total eosinophil counts, serum IL-5, and serum ECP levels at each of the 3 time points tested are shown in Table 2. Serial changes in serum IL-5 levels were significantly higher in group 1 relative to group 2 (P<0.001; Fig. 1), with group 1 exhibiting higher IL-5 levels at each of the three time points tested (P<0.05). However, no significant differences between time points were observed within each group.
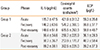
The serial change in eosinophil counts was higher in group 1 than in group 2 (P=0.001; Fig. 2). Furthermore, eosinophil counts were higher in group 1 than in group 2 in both the recovery and follow-up stages, but not during acute infection (P<0.05). No significant differences between time points were observed for either group.
As with IL-5 and eosinophil counts, the serial change in serum ECP levels was significantly higher in group 1 than in group 2 (P<0.001; Fig. 3), and for each time point, group 1 exhibited a higher ECP level than group 2 (P<0.05). A significant difference in ECP levels across time points was also evident in group 1, with ECP levels higher in both the recovery and follow-up stages, relative to during acute infection (P<0.05).
The data presented here demonstrated clear, phase-specific changes in serum IL-5, ECP, and total eosinophil counts in children with MP. Levels of all three markers were significantly higher in atopic patients (group 1) 2 months after recovery of pneumonia than in the non-atopic control group (group 2). With the exception of eosinophil counts in the acute phase of disease, each of these markers was significantly higher in group 1 than in group 2, across all time points tested. Within group 1, only serum ECP levels differed among time points, with both the recovery and 2 follow-up levels significantly higher than that during the acute phase of disease. Taken together, the data show pronounced increases in serum IL-5, serum ECP, and total eosinophil counts in atopic children relative to non-atopic controls.
Infections with M. pneumoniae have been shown to precede the onset of asthma, exacerbate asthmatic symptoms, and cause difficulties with asthma management.21 These symptoms are thought to be the result of M. pneumoniae infections, which cause chronic lower airway inflammation by impairing mucociliary clearance and increasing mucus production in the lung.22 Furthermore, M. pneumoniae exacerbates asthma by upregulating MUC5AC expression.23 These observations are consistent with murine studies that demonstrated airway hyper-responsiveness resembling chronic asthma.
The organism can be cultured from rodent lung for over 1 year after the initial infection, permitting long-term studies of the effects of M. pneumoniae infection on lung anatomy, physiology, and allergic sensitization.10 Interestingly, Th2-dominant airway inflammation seems to potentiate the survival of M. pneumoniae in the lung.10,24 Human subjects with allergic sensitization of the lung may therefore be at increased risk of developing chronic airway colonization by M. pneumoniae, resulting in enhanced airway hyperreactivity.1
Recent studies have identified specific factors associated with the clinical symptoms of asthma. M. pneumoniae has been shown to trigger wheezing by means of increased IL-5 secretion in subjects predisposed to asthma, whether as a result of their genetic background, or through previous events that have primed their immune system and lungs.12 Similar results were reported by Choi et al.25 who identified elevated levels of serum IL-5, VEGF, and ECP, along with increase blood eosinophil counts in children with wheezing during acute MP. These findings are consistent with the results described here, which showed higher levels of serum IL-5, ECP, and eosinophil counts, in atopic children with acute MP.
IL-5 plays a key role in eosinophil differentiation, maturation, recruitment, and activation at sites of inflammation during the development of allergic airway inflammation in asthmatic patients.26,27,28 Eosinophils act as a primary mediator of inflammation in asthma pathogenesis,29 with even mild asthmatics exhibiting significant increases in the numbers of activated eosinophils found in biopsies of the airway mucosa and in bronchoalveolar lavage.30,31 Previously, we reported that serum IL-5 levels were significantly higher in atopic children with MP during the recovery phase, relative to samples collected at the time of admission32; similar results were not seen in non-atopic children with MP.
ECP is currently the most widely used clinical marker of eosinophil activity in asthma.32 It has been shown to have cytotoxic effects on respiratory epithelial cells,33 stimulates mucous production in airways, and histamine release by basophils and mast cells in vitro.34 Serum ECP levels are directly correlated with the number of eosinophils in BAL and lung biopsies, making ECP an excellent marker for gauging the degree of eosinophilic inflammation.31 Furthermore, clinical studies have suggested that eosinophil granule proteins, of which ECP is the best characterized, are useful for assessing and managing asthma.35
In this study, we focused on the gradual increase in serum IL-5, ECP, and eosinophil counts in process of phases in atopic and non-atopic patients. Serial increases in all three parameters persisted for at least 2 months after resolution of pneumonia. These data suggest a long-term effect of M. pneumoniae infection on allergic inflammation, with significant implications for the treatment of atopic asthma.
We also focused on the role of eosinophil activation in allergic inflammation due to M. pneumoniae infection. Although anti-mycoplasma antibody titers had decreased by 2 months post-recovery, serum IL-5, ECP, and eosinophil counts in atopic children with MP gradually increased between the acute, recovery, and follow-up phases of the disease at levels significantly higher than that of non-atopic controls. Furthermore, serum ECP levels in atopic children were significantly higher in the recovery and follow-up phases, as compared with the acute phase of disease. This effect was unique to ECP, with other parameters showing no statistically significant differences among time points. These data imply that activated eosinophils, represented by ECP, may contribute to the allergic inflammatory seen in atopic children with MP.
Few limitations of this study should be noted. First, our findings were confined to a 2-month follow-up period, which may not be sufficient to gauge the period of abnormal immune responses after M. pneumoniae infection. Second, the definition of atopy used in this study was not based on allergen-specific IgE, but was instead a measurement of predisposition to atopy.
In this study, we investigated changes in three immunologic mediators, focusing primarily on the eosinophil-related immunologic reaction in MP. However, it has been suggested that eosinophils within the airway may be regulated by IL-5-independent mechanisms,36 such as IL-3 and granulocyte monocyte colony stimulating factor can sustain tissue eosinophilia in the absence of IL-5.28 In addition, treatment of asthmatic patients with an anti-IL-5 mAb reduced circulating and sputum eosinophils, but did not inhibit airway responses to inhaled allergen,37 suggesting that IL-5 may be dispensable in airway inflammation.
The most significant aspect of this study was its evaluation of the long-term impact of MP on allergic inflammation, as patients were followed for a considerable period of time beyond resolution of pneumonia-like symptoms. Persistently increasing levels of serum IL-5, ECP, and eosinophil counts are indicative of an increase in allergic inflammation driven primarily by activated eosinophils, and may contribute to clinical manifestation, such as wheezing, excessive mucus production, and allergic stimulation. Further evaluation is needed to determine whether our results correlate with clinical manifestations or lung function over a longer period of time.
Figures and Tables
Fig. 1
Serial changes in serum IL-5 levels, and comparison of serum IL-5 levels during each phase of disease. Serial changes in serum IL-5 levels were significantly higher in group 1 than in group 2 (P<0.001). Group 1 IL-5 levels were consistently higher than those of group 2 at each of the three time points tested (P<0.05). *P<0.05. IL, interleukin.

Fig. 2
Serial changes in peripheral blood eosinophil counts, and comparison of eosinophil counts during each phase of disease. The serial change in eosinophil counts was higher in group 1 than in group 2 (P=0.001). *P<0.05.
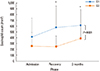
Fig. 3
Serial changes in serum ECP levels, and comparison of serum ECP levels during each phase of disease. The serial change in serum ECP level in group 1 was higher than in group 2 (P<0.001). Within group 1, ECP levels were higher at both recovery and 2 months post-recover than during the acute phase of infection (P<0.05). *P<0.05. ECP, eosinophil cationic protein.

Table 1
Clinical characteristics and laboratory findings in atopic (group 1) and non-atopic (group 2) patients.
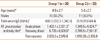
Table 2
Serum levels of IL-5, eosinophil counts, and ECP in the three phases of pneumonia*
References
1. Atkinson TP, Balish MF, Waites KB. Epidemiology, clinical manifestations, pathogenesis and laboratory detection of Mycoplasma pneumoniae infections. FEMS Microbiol Rev. 2008; 32:956–973.
2. Clyde WA Jr. Clinical overview of typical Mycoplasma pneumoniae infections. Clin Infect Dis. 1993; 17:Suppl 1. S32–S36.
3. Powell DA. Mycoplasmal infections. In : Kliegman RM, Stanton BF, St. Geme JW, Schor NF, Behrman RE, editors. Nelson textbook of pediatrics. Philadelphia (PA): Elsevier Saunders;2011. p. 1029–1032.
4. Kim SH, Jung SW. Properties of M. pneumoniae infections in Korea, 2011. Public Health Wkly Rep. 2011; 4:893–896.
5. Seggev JS, Lis I, Siman-Tov R, Gutman R, Abu-Samara H, Schey G, Naot Y. Mycoplasma pneumoniae is a frequent cause of exacerbation of bronchial asthma in adults. Ann Allergy. 1986; 57:263–265.
6. Biscardi S, Lorrot M, Marc E, Moulin F, Boutonnat-Faucher B, Heilbronner C, Iniguez JL, Chaussain M, Nicand E, Raymond J, Gendrel D. Mycoplasma pneumoniae and asthma in children. Clin Infect Dis. 2004; 38:1341–1346.
7. Wilsher ML, Kolbe J. Association of Mycoplasma pneumoniae antigen with initial onset of bronchial asthma. Am J Respir Crit Care Med. 1995; 151:579–580.
8. Biscione GL, Corne J, Chauhan AJ, Johnston SL. Increased frequency of detection of Chlamydophila pneumoniae in asthma. Eur Respir J. 2004; 24:745–749.
9. Kraft M, Cassell GH, Pak J, Martin RJ. Mycoplasma pneumoniae and Chlamydia pneumoniae in asthma: effect of clarithromycin. Chest. 2002; 121:1782–1788.
10. Hardy RD, Jafri HS, Olsen K, Hatfield J, Iglehart J, Rogers BB, Patel P, Cassell G, McCracken GH, Ramilo O. Mycoplasma pneumoniae induces chronic respiratory infection, airway hyperreactivity, and pulmonary inflammation: a murine model of infection-associated chronic reactive airway disease. Infect Immun. 2002; 70:649–654.
11. Afshar R, Medoff BD, Luster AD. Allergic asthma: a tale of many T cells. Clin Exp Allergy. 2008; 38:1847–1857.
12. Esposito S, Droghetti R, Bosis S, Claut L, Marchisio P, Principi N. Cytokine secretion in children with acute Mycoplasma pneumoniae infection and wheeze. Pediatr Pulmonol. 2002; 34:122–127.
13. Jeong YC, Yeo MS, Kim JH, Lee HB, Oh JW. Mycoplasma pneumoniae infection affects the serum levels of vascular endothelial growth factor and interleukin-5 in atopic children. Allergy Asthma Immunol Res. 2012; 4:92–97.
14. Gleich GJ, Adolphson CR. The eosinophilic leukocyte: structure and function. Adv Immunol. 1986; 39:177–253.
15. Coyle AJ, Uchida D, Ackerman SJ, Mitzner W, Irvin CG. Role of cationic proteins in the airway. Hyperresponsiveness due to airway inflammation. Am J Respir Crit Care Med. 1994; 150:S63–S71.
16. Kitahara H, Yamashita R, Kanemitsu T, Niwa I, Osano M. Relationship between M. pneumoniae infections and eosinophilia. Proceedings of the 12th Annual Congress of the Japanese Society of Mycoplasmology. Tokyo: Japanese Society of Mycoplasmology;1985. p. 75–78.
17. Yamashita R, Kitahara H, Kanemitsu T, Takeda T, Yamaguchi S. Eosinophil cationic protein in the sera of patients with Mycoplasma pneumonia. Pediatr Infect Dis J. 1994; 13:379–381.
18. Marsh DG, Bias WB, Ishizaka K. Genetic control of basal serum immunoglobulin E level and its effect on specific reaginic sensitivity. Proc Natl Acad Sci U S A. 1974; 71:3588–3592.
19. Wittig HJ, Belloit J, De Fillippi I, Royal G. Age-related serum immunoglobulin E levels in healthy subjects and in patients with allergic disease. J Allergy Clin Immunol. 1980; 66:305–313.
20. Peterson CG, Enander I, Nystrand J, Anderson AS, Nilsson L, Venge P. Radioimmunoassay of human eosinophil cationic protein (ECP) by an improved method. Establishment of normal levels in serum and turnover in vivo. Clin Exp Allergy. 1991; 21:561–567.
21. MacDowell AL, Bacharier LB. Infectious triggers of asthma. Immunol Allergy Clin North Am. 2005; 25:45–66.
22. Kraft M, Cassell GH, Henson JE, Watson H, Williamson J, Marmion BP, Gaydos CA, Martin RJ. Detection of Mycoplasma pneumoniae in the airways of adults with chronic asthma. Am J Respir Crit Care Med. 1998; 158:998–1001.
23. Chu HW, Rino JG, Wexler RB, Campbell K, Harbeck RJ, Martin RJ. Mycoplasma pneumoniae infection increases airway collagen deposition in a murine model of allergic airway inflammation. Am J Physiol Lung Cell Mol Physiol. 2005; 289:L125–L133.
24. Martin RJ, Chu HW, Honour JM, Harbeck RJ. Airway inflammation and bronchial hyperresponsiveness after Mycoplasma pneumoniae infection in a murine model. Am J Respir Cell Mol Biol. 2001; 24:577–582.
25. Choi IS, Byeon JH, Yoo Y, Lee KC, Choung JT. Increased serum interleukin-5 and vascular endothelial growth factor in children with acute mycoplasma pneumonia and wheeze. Pediatr Pulmonol. 2009; 44:423–428.
26. Flood-Page PT, Menzies-Gow AN, Kay AB, Robinson DS. Eosinophil's role remains uncertain as anti-interleukin-5 only partially depletes numbers in asthmatic airway. Am J Respir Crit Care Med. 2003; 167:199–204.
27. Nakajima H, Takatsu K. Role of cytokines in allergic airway inflammation. Int Arch Allergy Immunol. 2007; 142:265–273.
28. Robinson DS, Hamid Q, Ying S, Tsicopoulos A, Barkans J, Bentley AM, Corrigan C, Durham SR, Kay AB. Predominant TH2-like bronchoalveolar T-lymphocyte population in atopic asthma. N Engl J Med. 1992; 326:298–304.
29. Frigas E, Gleich GJ. The eosinophil and the pathophysiology of asthma. J Allergy Clin Immunol. 1986; 77:527–537.
30. Synek M, Beasley R, Frew AJ, Goulding D, Holloway L, Lampe FC, Roche WR, Holgate ST. Cellular infiltration of the airways in asthma of varying severity. Am J Respir Crit Care Med. 1996; 154:224–230.
31. Oddera S, Silvestri M, Balbo A, Jovovich BO, Penna R, Crimi E, Rossi GA. Airway eosinophilic inflammation, epithelial damage, and bronchial hyperresponsiveness in patients with mild-moderate, stable asthma. Allergy. 1996; 51:100–107.
32. Venge P. Monitoring the allergic inflammation. Allergy. 2004; 59:26–32.
33. Lehrer RI, Szklarek D, Barton A, Ganz T, Hamann KJ, Gleich GJ. Antibacterial properties of eosinophil major basic protein and eosinophil cationic protein. J Immunol. 1989; 142:4428–4434.
34. Hernnäs J, Särnstrand B, Lindroth P, Peterson CG, Venge P, Malmström A. Eosinophil cationic protein alters proteoglycan metabolism in human lung fibroblast cultures. Eur J Cell Biol. 1992; 59:352–363.
35. Löwhagen O, Wever AM, Lusuardi M, Moscato G, De Backer WA, Gandola L, Donner CF, Ahlstedt S, Larsson L, Holgate ST. The inflammatory marker serum eosinophil cationic protein (ECP) compared with PEF as a tool to decide inhaled corticosteroid dose in asthmatic patients. Respir Med. 2002; 96:95–101.
36. Liu LY, Sedgwick JB, Bates ME, Vrtis RF, Gern JE, Kita H, Jarjour NN, Busse WW, Kelly EA. Decreased expression of membrane IL-5 receptor alpha on human eosinophils: II. IL-5 down-modulates its receptor via a proteinase-mediated process. J Immunol. 2002; 169:6459–6466.
37. Leckie MJ, ten Brinke A, Khan J, Diamant Z, O'Connor BJ, Walls CM, Mathur AK, Cowley HC, Chung KF, Djukanovic R, Hansel TT, Holgate ST, Sterk PJ, Barnes PJ. Effects of an interleukin-5 blocking monoclonal antibody on eosinophils, airway hyper-responsiveness, and the late asthmatic response. Lancet. 2000; 356:2144–2148.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download