Abstract
Purpose
As pet ownership increases, sensitization to animal allergens due to domestic exposure is a concern. Sensitization to animal allergens may occur from indirect exposure, as well as direct ownership of animals. However, there have been conflicting results regarding the association between pet ownership and sensitization to animal allergens in adults.
Methods
In total, 401 patients with various allergic diseases were enrolled in this study. We performed skin prick tests with 55 common inhalant and food allergens, including dog, cat, and rabbit allergens. A mean wheal diameter of 3 mm or greater was considered a positive reaction. The exposure modality to each animal allergen was investigated using a questionnaire and included present ownership, past ownership, occupational exposure, occasional exposure, contact with pet owner, and no contact. Present ownership, past ownership, occupational, and occasional exposure were regarded as direct exposure.
Results
The sensitization rate for animal allergens was 20.4% for dog, 15.0% for cat, and 9.0% for rabbit. Direct exposure to dogs (72.0%) was significantly higher than that of other animals (18.4% for cats and 16.7% for rabbits), whereas 'no contact' with cats (78.3%) and rabbits (83.3%) was significantly higher than with dogs (26.8%; P<0.0001). Independent risk factors for sensitization to animal allergens were sensitization to Dermatophagoides pteronyssinus (OR=2.4, P=0.052), Dermatophagoides farinae (OR=5.1, P<0.001), cat (OR=4.4, P<0.0001), and direct exposure to dogs (OR=1.5, P=0.029) for dog, and sensitization to dog (OR=4.4, P<0.0001) and rabbit (OR=2.6, P=0.036) for cats. Finally, for rabbits, the independent risk factor was sensitization to Alternaria (OR=6.0, P<0.002).
Sensitization to animal allergens is one of the most important risk factors for developing allergic diseases such as asthma, rhinitis, and atopic dermatitis, particularly in occupationally exposed workers.1 As furry pet ownership in indoor environments increases, sensitization to animal allergens from domestic exposure is a concern. Few studies have evaluated the association between pet ownership and sensitization to animal allergens in adults. Furthermore, the studies that have been conducted have differed according to the type of animals, exposure timing and duration, and study design.2 In general, the relationship between cat ownership and sensitization to cats is still controversial, but dog ownership has been shown to be preventive for sensitization to dogs.2
There is some evidence that indirect exposure, not direct ownership, can result in the development of sensitization to animal allergens and allergic diseases in the general population. Noertjojo et al. recently reported that the sensitization to cat allergens was a more important risk factor for the development of asthma and asthma-like symptoms than was cat ownership in adults, suggesting that sensitization to cats may develop regardless of cat ownership.3 It has also been reported that the risk of sensitization to pet allergens and asthma development increases among non-pet owners in areas with a high proportion of pet owners.4 According to a survey by the Seoul Development Institute in 2004, 17.2% of households in Seoul had pets, and the prevalence of dog ownership (16.6%) was remarkably higher than that of cat ownership (0.8%).5 However, the sensitization rate to cats was reported to be 9.1%, which is comparable to 8.6% for dogs in Korea,6 suggesting the development of sensitization to cats by indirect exposure. Thus, the purpose of this study was to investigate the relationship between pet ownership (cat, dog, and rabbit) and sensitization to each animal in patients with various allergic diseases. We classified pet exposure into several categories according to the modality of exposure in order to evaluate how direct or indirect exposure contributes to the development of sensitization to each pet in patients with various allergic diseases.
Patients who took allergy skin prick tests for evaluation of various allergic diseases from July 2007 to August 2008 at Hallym University Kangdong Sacred Heart Hospital were enrolled in this study. Allergy skin prick tests were performed with 55 common inhalant and food allergens including Dermatophagoides pteronyssinus, Dermatophagoides farinae, birch, ragweed, mugwort, Alternaria, dog epithelium, cat epithelium, and rabbit epithelium. A mean wheal diameter of 3 mm or greater was considered a positive reaction.
All patients provided informed consent. The Regional Institutional Board of Ethics of Hallym University Kangdong Sacred Heart Hospital approved this study.
We focused on 3 animal allergens: cat, dog, and rabbit. The patients completed the questionnaire about demographic characteristics, pet ownership, and modality of exposure to each animal (Fig. 1). Briefly, the questionnaire about exposure modality was modified from a previous report by Liccardi et al.7 and included the followings: 1) I have been keeping a dog (cat, rabbit) at home for more than 6 months - present ownership, 2) I have kept a dog (cat, rabbit) at home in the past for more than one year - past ownership, 3) I have a job that deals with a dog (cat, rabbit) - occupational exposure, 4) I do not keep a dog at home, but I come in close contact with dogs (cats, rabbits) occasionally outside - occasional exposure, 5) I am in contact with a person who keeps a dog (cat, rabbit) at home - indirect exposure, or 6) I have never been in contact with a dog (cat, rabbit) - no contact. Present ownership, past ownership, occupational exposure, and occasional exposure were regarded as direct exposure.
The prevalence was expressed as a percentage and continuous variables were expressed as the mean±standard deviation. Comparisons of the modality of exposure to each animal in the sensitized patients were performed using chi-square tests. To evaluate independent risk factors for sensitization to each animal allergen, multivariate analyses by binary logistic regression analyses were performed, controlling for age and sex as covariates, and were expressed as odds ratios with 95% confidence intervals (CI). A P value of less than 0.05 was regarded as statistically significant. All statistical analyses were performed using SPSS version 12.0 (SPSS Inc., Chicago, IL, USA).
In total, 401 patients were enrolled in this study. The mean age of the study subjects was 40.9±15.6 years with a range of 16 to 82, and 201 (50.1%) subjects were male. Of the subjects, 178 (44.4%) had a family history of allergic diseases. The most common clinical diagnosis of the patients was chronic cough (34.2%), followed by asthma (28.2%), allergic rhinitis (11.2%), urticaria (3.2%), and atopic dermatitis (2.5%). The prevalence of pet ownership in the past was 55.8% (dog: 52.9%, cat: 3.1%, rabbit: 7.6%), and the prevalence of pet ownership at present was 22.2% (dog: 83.1%, cat: 2.2%, rabbit: 0.2%). Sensitization rates to common inhalant allergens in the study subjects were 47.1% for Dermatophagoides pteronyssinus, 47.4% for Dermatophagoides farinae, 5.7% for Alternaria, 20.4% for dog epithelium, 15.0% for cat epithelium, 9.0% for rabbit epithelium, 10.7% for birch, 12.0% for ragweed, and 13.5% for mugwort (Fig. 2).
The clinical characteristics of the patients sensitized to each animal are shown in Table 1. The number of sensitized patients was 82 for dog, 60 for cat, and 36 for rabbit. There were no significant differences in sex, age, or family history of allergic diseases among the 3 groups. The prevalence of pet ownership in the past was 53.7% of the dog-sensitized group, 60.6% for the cat-sensitized group, and 55.6% for the rabbit-sensitized group. The prevalence of pet ownership at present was 41.5% of the dog-sensitized patients, 35.0% of the cat-sensitized patients, and 38.9% of the rabbit-sensitized patients. Dogs were the most popular pet raised in the past or at present, regardless of the sensitization to each animal. The most common clinical diagnosis of each group was asthma, followed by chronic cough, allergic rhinitis, and atopic dermatitis.
The sensitization rate to common inhalant allergens in each group showed a similar trend to the sensitization rate of all study subjects. House dust mites were the most commonly sensitized allergens (range: 77.8%-89.0%). Each group also showed relatively higher levels of co-sensitization to the other 2 animal allergens. Sensitization rates were 45.1% to cat and 23.2% to rabbit in the dog-sensitized group; 61.7% to dog and 28.3% to rabbit in the cat-sensitized group; 52.8% to dog and 47.2% to cat in the rabbit-sensitized group.
There were significant differences in the modality of exposure to each sensitized animal among 3 groups (Table 2). The prevalence of 'direct exposure' to each animal was significantly higher in the dog-sensitized group (72.0%) than in the other animal-sensitized groups (18.4% for cat, 16.7% for rabbit). 'No exposure' to the sensitized animal was significantly higher in the cat-sensitized group (78.3%) and rabbit-sensitized group (83.3%) than in the dog-sensitized group (26.8%) (P<0.0001).
When we analyzed independent risk factors for sensitization to each animal allergen, direct exposure to dogs (OR=1.5, P=0.029), as well as sensitization to Dermatophagoides pteronyssinus (OR=2.4, P=0.052), Dermatophagoides farinae (OR=5.1, P=0.001) and cat epithelium (OR=4.4, P<0.0001) were found to be independent risk factors for sensitization to the dog allergen. However, direct exposure to cat or rabbit were not independent risk factors for the sensitization to cat or rabbit. Sensitization to dog epithelium (OR=4.4, P<0.0001) and rabbit epithelium (OR=2.6, P=0.036) were independent risk factors for sensitization to cat, and the sensitization to Alternaria (OR=6.0, P=0.002) was an independent risk factor for sensitization to rabbit (Table 3).
We found that the prevalence of 'direct exposure' to dog was significantly higher in the dog-sensitized patients whereas 'no exposure' was significantly higher in the cat- or rabbit-sensitized patients. Direct dog exposure was one of the independent risk factors for sensitization to dog.
Although there have not been many studies about the relationship between dog ownership and sensitization to dogs, dog ownership has consistently been suggested to be protective for sensitization to dog.8-10 This is quite contrary to our results about dog ownership. Two previous reports investigated the effect of early-life dog exposure, such as in the first year of life, on sensitization to dog in childhood or adolescence.8,9 We also questioned the study subjects about pet ownership in the past. However, the question did not clarify the exact timing of pet ownership, but instead asked whether the subjects had owned certain types of pets as far as they could remember. This methodological difference would cause different results. One report that studied the relationship between current dog ownership and sensitization to dog in adulthood could not show any significant relationship between them.10 In addition, the study subjects in previous reports were from the general population, whereas our study population was composed of patients with various allergic diseases. Underlying allergic tendencies might influence the sensitization to dog allergens in this study. Thus, our results suggest that dog ownership is positively associated with the sensitization to dog allergen in allergic patients.
The association of cat ownership and development of sensitization to cats remains controversial. Some studies have shown protective effects but others reported an increased risk.9-12 A Danish group reported that current cat ownership was significantly associated with sensitization to cats which was tested by measuring specific IgE to cats in an adult population, in which approximately 40% owned cats previously or currently compared to just 1% in our study.10 This likely could influence the high prevalence of sensitization to cat. The prevalence of sensitization to cat is quite high in the Korean population even though cat ownership is very low,5,6,13-15 which is seemingly attributable to the many stray cats and their high reproduction rate in cities.16 Therefore, cat allergens seem to be common in our environment. People are unavoidably exposed to cat allergens, which might lead to the development of sensitization to cat in non-cat owners.
We also found that sensitizations to house dust mites and cat allergens were also independent risk factors for sensitization to dog allergens with higher odds ratios (OR: 2.4 for D. pteronyssinus, 5.2 for D. farinae, 4.4 for cat) than direct exposure (OR: 1.5). In addition, each sensitization to the other pet allergens or Alternaria was an independent risk factor for the sensitization to each animal (Table 3). Similarly, Linneberg et al.10 demonstrated that an atopic predisposition to allergens other than cat at baseline was an independent risk factor for the development of IgE sensitization to cat. Because house dust mites, Alternaria, and cat allergens are common inhalant allergens in our environment, this result implies that the individual atopic status of patients may play an important role for the sensitization to pets.
Moreover, a significant percentage of the dog (or cat, rabbit)-sensitized patients were co-sensitized to the other pet allergens in our study. It is plausible that these patients are sensitized to dogs by direct dog ownership and are sensitized to cats or rabbits by indirect exposure. However, cross-reactivity among animal allergens may also play a role. Knowledge regarding cross-allergenecity among animal allergens is still limited. Serum albumin has been reported as a major cross-reactive allergen in cat and dog dander (Fel d 2 for cat and Can f 3 for dog).17 Reininger et al.18 demonstrated a Fel d 1-like allergen in dog dander allergen extracts, suggesting a cross-reactive molecule between dog and cat allergens. Recently, the dog lipocalin allergen Can f 2 was reported to have cross-allergenecity with cat allergen Fel d 4.19 Further studies are required to elucidate whether co-sensitization to several pet allergens in a patient is due to direct or indirect exposure to each pet allergen or because of cross-reactivity among animal allergens.
In the current study, the sensitization rate to pet allergens was 20.4% for dog, 15.5% for cat, and 9.0% for rabbit in patients with various allergic diseases. These results were higher than those in other studies that evaluated the sensitization rates for common inhalant allergens in Korea. A recent multi-center study in Korea showed an 8.6% sensitization rate for dog and 9.1% for cat,6 and another study in a large city in southern Korea showed a 5.8% sensitization rate for dog and 10.2% for cat.13 Two studies from rural Korea reported relatively lower sensitization rates for dog and cat allergens, approximately 5% less than the results from the large cities.14,15 These differences may be explained by regional variations such as living environments or the prevalence of pet ownership in a local community. In one report from California, the cat sensitization rate was much higher (37%) than that in Korea, which might be due to the relatively low rate of cat ownership in Korea compared with western countries.5,20 There are limited data about the rabbit sensitization rate in Korea because rabbit has not been considered a common animal allergen. Two previous studies reported 7.8% and 11.8% rates of rabbit sensitization, which were similar with our results.13,14 This relatively high sensitization to rabbit allergens cannot be explained by direct ownership because rabbits are uncommon pets in Korea. However, rabbit has recently been reported to be an important pet allergen in the development of significant respiratory allergic diseases owing to household rabbit exposure.21 Additionally, rabbit ownership is increasing.7,21 Therefore, it is necessary to pay attention to rabbit sensitization in allergic patients. Further study will be needed to elucidate this relationship and determine the cross-allergenecity between rabbit and other animal allergens.
Our study has several limitations. The first is a relatively small number of study subjects. The second is that the questionnaire did not ask about the timing of past pet ownership and the duration of current pet ownership. Without regard to exposure timing or the duration of pet ownership, we classified all current and past pet ownership into 'direct exposure'. Short current or very remote past exposure to pets might influence the sensitization to animal allergens differently. Furthermore, assessment of pet exposure was based on individual recall, which might have potential bias.22 The third limitation is that our study population included only patients with various allergic diseases. Patients with allergic diseases tend to avoid pets at home, and this could influence our results.23
In conclusion, our results suggest that direct exposure to dog allergens by dog ownership in the past and present contributes to sensitization to dog allergens in adult patients with allergic diseases. Sensitization to cat allergens can develop in non-cat owners without direct exposure, suggesting that cat allergens may be prevalent in our public environment. A prospective study with a larger cohort and more detailed evaluation of pet ownership will be needed to verify our findings.
Figures and Tables
Fig. 1
Questionnaire regarding pet ownership and exposure modality. The questionnaire was modified from a previous report by Liccardi et al.7

Fig. 2
The sensitization rate of common inhalant allergens in the study subjects. Dp, Dermatophagoides pteronyssinus; Df, Dermatophagoides farinae.
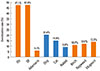
Table 1
Clinical characteristics of subjects sensitized to each animal allergen

Table 2
Modality of exposure to each animal
| Dog (%) | Cat (%) | Rabbit (%) | |
|---|---|---|---|
| Direct* | 72.0 | 18.4 | 16.7 |
| Past and present ownership | 67.1 | 13.4 | 13.9 |
| Occupational | 0 | 1.7 | 0 |
| Occasional | 4.9 | 3.3 | 2.8 |
| Indirect | 1.2 | 3.3 | 0 |
| No exposure | 26.8 | 78.3 | 83.3 |
Table 3
Independent risk factors for sensitization to each animal allergen

ACKNOWLEDGMENTS
This study was supported by the Hallym University Medical Center Research Fund (01-2008-08).
References
1. Bush RK, Wood RA, Eggleston PA. Laboratory animal allergy. J Allergy Clin Immunol. 1998; 102:99–112.
2. Simpson A, Custovic A. Pets and the development of allergic sensitization. Curr Allergy Asthma Rep. 2005; 5:212–220.
3. Noertjojo K, Dimich-Ward H, Obata H, Manfreda J, Chan-Yeung M. Exposure and sensitization to cat dander: asthma and asthma-like symptoms among adults. J Allergy Clin Immunol. 1999; 103:60–65.
4. Plaschke P, Janson C, Norrman E, Björnsson E, Ellbjär S, Järvholm B. Association between atopic sensitization and asthma and bronchial hyperresponsiveness in swedish adults: pets, and not mites, are the most important allergens. J Allergy Clin Immunol. 1999; 104:58–65.
5. Yoo KY, Cho SH, Gin Y, Lee YJ. Strategic guidelines to protect and manage pet animals in Seoul (SDI 04-R-21). Seoul: The Seoul Institute;2004.
6. Kim TB, Kim KM, Kim SH, Kang HR, Chang YS, Kim CW, Bahn JW, Kim YK, Kang HT, Cho SH, Park HS, Lee JM, Choi IS, Min KU, Hong CS, Kim NS, Kim YY. Sensitization rates for inhalant allergens in Korea; a multi-center study. J Asthma Allergy Clin Immunol. 2003; 23:483–493.
7. Liccardi G, Passalacqua G. Sensitization to rabbit allergens in Italy--a multicentre study in atopic subjects without occupational exposure. Int Arch Allergy Immunol. 2006; 141:295–299.
8. Ownby DR, Johnson CC, Peterson EL. Exposure to dogs and cats in the first year of life and risk of allergic sensitization at 6 to 7 years of age. JAMA. 2002; 288:963–972.
9. Van Gysel D, Govaere E, Verhamme K, Doli E, De Baets F. Exposure to pets and the association with sensitization and allergic disease in Belgian schoolchildren. Allergy. 2009; 64:663–664.
10. Linneberg A, Nielsen NH, Madsen F, Frølund L, Dirksen A, Jørgensen T. Pets in the home and the development of pet allergy in adulthood. The Copenhagen Allergy Study. Allergy. 2003; 58:21–26.
11. Roost HP, Künzli N, Schindler C, Jarvis D, Chinn S, Perruchoud AP, Ackermann-Liebrich U, Burney P, Wüthrich B. Role of current and childhood exposure to cat and atopic sensitization. European Community Respiratory Health Survey. J Allergy Clin Immunol. 1999; 104:941–947.
12. Custovic A, Hallam CL, Simpson BM, Craven M, Simpson A, Woodcock A. Decreased prevalence of sensitization to cats with high exposure to cat allergen. J Allergy Clin Immunol. 2001; 108:537–539.
13. Kim KH, Kim KT, Lee SK, Park HS, Lee YM, Nahm DH, Son CH, Yang DK, Roh MS, Choi PJ, Lee JH, Kim KN, Lee KN. Sensitization rates for inhalant allergens in patients with respiratory allergy in Busan. Korean J Asthma Allergy Clin Immunol. 2005; 25:59–63.
14. Lee MK, Lee WY, Yong SJ, Shin KC, Lee SN, Lee SJ, Lee JH, Jung S, Jung YR, Kim SH. Sensitization rates to inhalant allergens in patients visiting a university hospital in Gangwon region. Korean J Asthma Allergy Clin Immunol. 2011; 31:27–32.
15. Yoon BJ, Kim SH, Kim DH, Koh YI. Longitudinal changes of sensitization rates to inhalant allergens in patients with allergic diseases from Gwangju and Chonnam areas: their association with annual changes in temperature. Korean J Asthma Allergy Clin Immunol. 2011; 31:93–104.
16. Kim JY. Serological and molecular biological survey of Toxoplasma gondii infection in neutralized stray and household cats in Seoul [thesis]. Chuncheon: Kangwon National University;2010.
17. Boutin Y, Hébert H, Vrancken ER, Mourad W. Allergenicity and cross-reactivity of cat and dog allergenic extracts. Clin Allergy. 1988; 18:287–293.
18. Reininger R, Varga EM, Zach M, Balic N, Lindemeier AD, Swoboda I, Grönlund H, van Hage M, Rumpold H, Valenta R, Spitzauer S. Detection of an allergen in dog dander that cross-reacts with the major cat allergen, Fel d 1. Clin Exp Allergy. 2007; 37:116–124.
19. Madhurantakam C, Nilsson OB, Uchtenhagen H, Konradsen J, Saarne T, Högbom E, Sandalova T, Grönlund H, Achour A. Crystal structure of the dog lipocalin allergen Can f 2: implications for cross-reactivity to the cat allergen Fel d 4. J Mol Biol. 2010; 401:68–83.
20. Galant S, Berger W, Gillman S, Goldsobel A, Incaudo G, Kanter L, Machtinger S, McLean A, Prenner B, Sokol W, Spector S, Welch M, Ziering W. Prevalence of sensitization to aeroallergens in California patients with respiratory allergy. Allergy Skin Test Project Team. Ann Allergy Asthma Immunol. 1998; 81:203–210.
21. Choi JH, Kim HM, Park HS. Allergic asthma and rhinitis caused by household rabbit exposure: identification of serum-specific IgE and its allergens. J Korean Med Sci. 2007; 22:820–824.
22. Svanes C, Dharmage S, Sunyer J, Zock JP, Norbäck D, Wjst M, Heinrich J, Jarvis D, de Marco R, Plana E, Villani S, Antó JM. Long-term reliability in reporting of childhood pets by adults interviewed twice, 9 years apart. Results from the European Community Respiratory Health Survey I and II. Indoor Air. 2008; 18:84–92.
23. Svanes C, Zock JP, Antó J, Dharmage S, Norbäck D, Wjst M, Heinrich J, Jarvis D, de Marco R, Plana E, Raherison C, Sunyer J. Early Life Working Group of the European Community Respiratory Health Survey. Do asthma and allergy influence subsequent pet keeping? An analysis of childhood and adulthood. J Allergy Clin Immunol. 2006; 118:691–698.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download