1. Ciprandi G, Cirillo I, Tosca MA, Vizzaccaro A. Bronchial hyperreactivity and spirometric impairment in polysensitized patients with allergic rhinitis. Clin Mol Allergy. 2004; 2:3.
2. Prieto L, Gutiérrez V, Liñana J, Marín J. Bronchoconstriction induced by inhaled adenosine 5'-monophosphate in subjects with allergic rhinitis. Eur Respir J. 2001; 17:64–70.
3. Tatar M, Petriskova J, Zucha J, Pecova R, Hutka Z, Raffajova J, Brozmanova M. Induced sputum eosinophils, bronchial reactivity, and cough sensitivity in subjects with allergic rhinitis. J Physiol Pharmacol. 2005; 56:Suppl 4. 227–236.
4. Laprise C, Boulet LP. Asymptomatic airway hyperresponsiveness: a three-year follow-up. Am J Respir Crit Care Med. 1997; 156:403–409.
5. Porsbjerg C, von Linstow ML, Ulrik CS, Nepper-Christensen S, Backer V. Risk factors for onset of asthma: a 12-year prospective follow-up study. Chest. 2006; 129:309–316.
6. Park YM, Bochner BS. Eosinophil survival and apoptosis in health and disease. Allergy Asthma Immunol Res. 2010; 2:87–101.
7. Polosa R, Ciamarra I, Mangano G, Prosperini G, Pistorio MP, Vancheri C, Crimi N. Bronchial hyperresponsiveness and airway inflammation markers in nonasthmatics with allergic rhinitis. Eur Respir J. 2000; 15:30–35.
8. Gutiérrez V, Prieto L, Torres V, Morales C, González E. Peak flow variability and sputum eosinophilia in allergic rhinitis. Ann Allergy Asthma Immunol. 1998; 81:143–150.
9. Park CS. Eosinophilic bronchitis, eosinophilia associated genetic variants, and notch signaling in asthma. Allergy Asthma Immunol Res. 2010; 2:188–194.
10. Brightling CE, Woltmann G, Wardlaw AJ, Pavord ID. Development of irreversible airflow obstruction in a patient with eosinophilic bronchitis without asthma. Eur Respir J. 1999; 14:1228–1230.
11. Halwani R, Al-Muhsen S, Al-Jahdali H, Hamid Q. Role of transforming growth factor-beta in airway remodeling in asthma. Am J Respir Cell Mol Biol. 2011; 44:127–133.
12. Ohbayashi H, Shimokata K. Matrix metalloproteinase-9 and airway remodeling in asthma. Curr Drug Targets Inflamm Allergy. 2005; 4:177–181.
13. Bergeron C, Tulic MK, Hamid Q. Tools used to measure airway remodelling in research. Eur Respir J. 2007; 29:596–604.
14. Cataldo DD, Gueders M, Munaut C, Rocks N, Bartsch P, Foidart JM, Noël A, Louis R. Matrix metalloproteinases and tissue inhibitors of matrix metalloproteinases mRNA transcripts in the bronchial secretions of asthmatics. Lab Invest. 2004; 84:418–424.
15. Brozek JL, Bousquet J, Baena-Cagnani CE, Bonini S, Canonica GW, Casale TB, van Wijk RG, Ohta K, Zuberbier T, Schünemann HJ;. Global Allergy and Asthma European Network. Grading of Recommendations Assessment, Development and Evaluation Working Group. Allergic Rhinitis and its Impact on Asthma (ARIA) guidelines: 2010 revision. J Allergy Clin Immunol. 2010; 126:466–476.
16. Sohn SW, Lee HS, Park HW, Chang YS, Kim YK, Cho SH, Kim YY, Min KU. Evaluation of cytokine mRNA in induced sputum from patients with allergic rhinitis: relationship to airway hyperresponsiveness. Allergy. 2008; 63:268–273.
17. Alvarez MJ, Olaguibel JM, García BE, Rodríquez A, Tabar AI, Urbiola E. Airway inflammation in asthma and perennial allergic rhinitis. Relationship with nonspecific bronchial responsiveness and maximal airway narrowing. Allergy. 2000; 55:355–362.
18. Leone C, Teodoro C, Pelucchi A, Mastropasqua B, Cavigioli G, Marazzini L, Foresi A. Bronchial responsiveness and airway inflammation in patients with nonallergic rhinitis with eosinophilia syndrome. J Allergy Clin Immunol. 1997; 100:775–780.
19. Ciprandi G, Cirillo I. The lower airway pathology of rhinitis. J Allergy Clin Immunol. 2006; 118:1105–1109.
20. Kessel A, Halloun H, Bamberger E, Kugelman A, Toubi E. Abnormal spirometry in children with persistent allergic rhinitis due to mite sensitization: the benefit of nasal corticosteroids. Pediatr Allergy Immunol. 2008; 19:61–66.
21. Brightling CE. Chronic cough due to nonasthmatic eosinophilic bronchitis: ACCP evidence-based clinical practice guidelines. Chest. 2006; 129:116S–121S.
22. Park SW, Lee YM, Jang AS, Lee JH, Hwangbo Y, Kim DJ, Park CS. Development of chronic airway obstruction in patients with eosinophilic bronchitis: a prospective follow-up study. Chest. 2004; 125:1998–2004.
23. Brightling CE, Bradding P, Symon FA, Holgate ST, Wardlaw AJ, Pavord ID. Mast-cell infiltration of airway smooth muscle in asthma. N Engl J Med. 2002; 346:1699–1705.
24. Chakir J, Laviolette M, Boutet M, Laliberté R, Dubé J, Boulet LP. Lower airways remodeling in nonasthmatic subjects with allergic rhinitis. Lab Invest. 1996; 75:735–744.
25. Demedts IK, Brusselle GG, Bracke KR, Vermaelen KY, Pauwels RA. Matrix metalloproteinases in asthma and COPD. Curr Opin Pharmacol. 2005; 5:257–263.
26. Atkinson JJ, Senior RM. Matrix metalloproteinase-9 in lung remodeling. Am J Respir Cell Mol Biol. 2003; 28:12–24.
27. Watson WT, Becker AB, Simons FE. Treatment of allergic rhinitis with intranasal corticosteroids in patients with mild asthma: effect on lower airway responsiveness. J Allergy Clin Immunol. 1993; 91:97–101.
28. Dahl R, Nielsen LP, Kips J, Foresi A, Cauwenberge P, Tudoric N, Howarth P, Richards DH, Williams M, Pauwels R. SPIRA Study Group. Intranasal and inhaled fluticasone propionate for pollen-induced rhinitis and asthma. Allergy. 2005; 60:875–881.
29. Orhan F, Sekerel BE, Adalioglu G, Pinar M, Tuncer A. Effect of nasal triamcinolone acetonide on seasonal variations of bronchial hyperresponsiveness and bronchial inflammation in nonasthmatic children with seasonal allergic rhinitis. Ann Allergy Asthma Immunol. 2004; 92:438–445.
30. van Rensen EL, Straathof KC, Veselic-Charvat MA, Zwinderman AH, Bel EH, Sterk PJ. Effect of inhaled steroids on airway hyperresponsiveness, sputum eosinophils, and exhaled nitric oxide levels in patients with asthma. Thorax. 1999; 54:403–408.
31. Mattos W, Lim S, Russell R, Jatakanon A, Chung KF, Barnes PJ. Matrix metalloproteinase-9 expression in asthma: effect of asthma severity, allergen challenge, and inhaled corticosteroids. Chest. 2002; 122:1543–1552.
32. Chakir J, Shannon J, Molet S, Fukakusa M, Elias J, Laviolette M, Boulet LP, Hamid Q. Airway remodeling-associated mediators in moderate to severe asthma: effect of steroids on TGF-β, IL-11, IL-17, and type I and type III collagen expression. J Allergy Clin Immunol. 2003; 111:1293–1298.

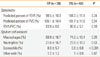
 ) represent mean mRNA levels, and vertical bars indicate standard deviations.
) represent mean mRNA levels, and vertical bars indicate standard deviations.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download