Abstract
Purpose
Gastro-esophageal reflux (GER), particularly non-acid reflux, is common in infants and is a known cause of chronic respiratory symptoms in infancy. Recent guidelines recommended empirical acid suppression therapy and the head-up position in patients with suspected GER. However, the efficacy of the upright position in relieving GER and reflux-related respiratory symptoms in infants is unclear. We conducted this study to investigate the efficacy of the upright position on GER and reflux-related respiratory symptoms in infants with chronic respiratory symptoms.
Methods
Thirty-two infants (21 male; median age, 5 months; range, 0 to 19 months) with unexplained chronic respiratory symptoms underwent multi-channel intraluminal esophageal impedance and pH monitoring. We retrospectively compared the frequencies of GER and reflux-related symptoms according to body position.
Results
A mean of 3.30 episodes of reflux per hour was detected. Overall, refluxes were more frequent during the postprandial period than the emptying period (3.77 vs. 2.79 episodes/hour, respectively; P=0.01). Although there was no significant difference in the total refluxes per hour between the upright and recumbent positions (6.12 vs. 3.77 episodes, P=0.10), reflux-related respiratory symptoms per reflux were significantly fewer in infants kept in an upright position than in a recumbent position during the postprandial period (3.07% vs. 14.75%, P=0.016). Non-acid reflux was the predominant type of reflux in infants, regardless of body position or meal time.
Gastro-esophageal reflux (GER) is defined as the retrograde passage of gastric contents into the esophagus.1 GER is physiologically frequent in infants and tends to resolve spontaneously.2,3 However, it frequently causes GER disease (GERD), including esophagitis, failure to thrive, anemia, and respiratory disease. Young children and infants cannot self-detect and explain their symptoms related to reflux. Therefore, silent GER is frequent in children with chronic pulmonary disease.4,5 GER has been accepted as a major cause of chronic respiratory symptoms in young children.3,6
The accurate diagnosis of pathological GER in chronic respiratory disease is important, as it leads to appropriate treatment that has been shown to improve respiratory symptoms7 and curtail malpractice. Conventional pH monitoring has been considered the gold standard for the detection of GER. However, GER frequently occurs in the postprandial period, and conventional pH monitoring does not adequately detect non-acid reflux in a pH range above 4.0.8,9 Thus, it has significant limitations for detecting non-acidic bolus movement in the esophagus, particularly in infants who are frequently fed milk formula, which neutralizes the acidity of gastric contents.8,10 To overcome this limitation, multi-channel intraluminal esophageal impedance and pH (MII-pH) monitoring to detect reflux, regardless of its acidity, was developed.8
Recent guidelines recommended empirical acid suppression therapy and the head-up position in patients with suspected GER.11 Owing to the fact that non-acid reflux cannot be eliminated by antacid therapy and because maintaining the upright position is difficult in early infancy, this recommended therapy often fails to prevent reflux and reflux-related symptoms. The literature on the association between non-acid reflux and respiratory symptoms has been inconsistent; some studies have supported this association,12,13 while others have disputed it.14,15 In addition, there is little information on the efficacy of the upright position on reflux and reflux-related symptoms in infants.2 The efficacy of the upright position on GER (particularly non-acid reflux) and reflux-related respiratory symptoms has important clinical implications.
The aim of our study was to investigate the efficacy of the upright position on GER and reflux-related symptoms as assessed by MII-pH monitoring in infants with chronic respiratory symptoms.
The subjects included in this study were 32 infants who had visited the Pediatric Allergy and Respiratory center in Soonchunhyang University Hospital (a tertiary medical center in Seoul, Korea) from 1 January 2006 to 31 July 2007. All subjects were referred to the center for evaluation of the cause of unexplained respiratory symptoms that lasted for longer than one month. This retrospective study investigated the efficacy of the upright position on GER and reflux-related respiratory symptoms as assessed by MII-pH monitoring. The investigation used a within-subjects design, without controls and without repeated measures. We reviewed the clinical medical records and demographic data included in the electronic and paper charts of all subjects. The MII-pH recordings were manually reviewed by the primary investigator. The study protocol was approved by the Institutional Review Board of Soonchunhyang University Hospital.
Thirty-two infants (21 [65.6%] males; median age, 5 months; range, 0 to 19 months) with unexplained chronic respiratory symptoms underwent MII-pH monitoring. Unexplained chronic respiratory symptoms were defined as chronic respiratory symptoms (i.e., cough, wheezing, stridor, cyanosis, or apnea) that persisted for longer than one month, despite a full work-up for differential diagnosis (i.e., asthma, pertussis, seizure disorder, inborn error of metabolism, primary immune deficiency, and congenital anomalies of the heart, gastrointestinal system, and lungs) and adequate treatment, including acid suppressants (proton pump inhibitor or H2-blockers) over 2 weeks. The chronic respiratory symptoms in our cohort included: cough in 28/32 (87.5%) patients, dyspnea in 7/32 (21.9%), choking in 2/32 (6.3%), tachypnea in 7/32 (21.9%), apnea in 2/32 (6.3%), cyanosis in 9/32 (28.1%), and recurrent noisy respiration in 16/32 (50.0%) patients.
Exclusion criteria included patients with neurological, metabolic, or chronic respiratory disease; congenital anomaly of the heart, gastrointestinal system, or lungs; acute gastrointestinal infection; known or suspected immunodeficiency; premature birth; pneumonia demonstrated by physical exam or chest radiography; and evidence of upper respiratory infection (fever and rhinorrhea).
All subjects were admitted to the hospital for MII-pH monitoring. For 24 hours during the test, all subjects continued with their regular diet, with the exclusion of very hot or cold beverages and acidic juices. Although MII-pH monitoring was able to differentiate swallows from GER, meal time was excluded from the analysis to avoid confusion. Acid suppressants (proton pump inhibitors or H2-blockers), antacids, and prokinetics were discontinued for at least one week prior to MII-pH monitoring. Subjects were maintained in the upright position by using a baby car seat at a 30-degree angle during the postprandial period (2 hours after feeding) and in the recumbent position during the emptying period. Parents recorded the times of the start and end of feedings and all symptoms (cough, wheezy respiration, cyanosis, dyspnea, apnea, vomiting, rumination, and choking) in a diary and with an event marker before and during MII-pH monitoring.
A MII-pH flexible catheter (diameter, 2.13 mm; Sandhill Scientific, Highlands Ranch, CO, USA), age-appropriate for infants, was used in this study. It had six impedance channels and one antimony pH probe. The pH sensor was calibrated using pH 4.0 and 7.0 standard buffers before starting. The catheter was passed into the esophagus using a transnasal approach, and the pH sensor was located 2 cm above the lower esophageal sphincter. The six impedance channels were located 2.0, 3.5, 5.0, 6.5, 8.0, and 9.5 cm from the distal tip of the MII-pH probe. Esophageal manometry and Strobel's formula were used to determine proper positioning of the catheter.
The catheter was connected to a portable data acquisition system (Sleuth system; Sandhill Scientific), which stored data from all impedance channels at a frequency of 50 Hz. Data were automatically analyzed by a computerized software program (Bio-View; Sandhill Scientific) and manually confirmed by visual analysis by a single investigator.
A reflux episode was defined as a retrograde bolus movement across at least two distal channels, with a drop in baseline impedance of at least 50%.8 Acid reflux was defined as a detected reflux with a drop in intraesophageal pH to <4.0. Non-acid reflux was divided into weakly acidic reflux (4.0≤pH<7.0) and alkaline reflux (≥7.0). For the purpose of this study, we defined both weakly acidic reflux and alkaline reflux as non-acid reflux, as introduced in previous studies.15-17
The symptom index (SI) and symptom sensitivity index (SSI) were calculated for each patient to detect the relationship between reflux and its related symptoms, including respiratory (cough, cyanosis, dyspnea, apnea, and wheezy respiration) and other symptoms (vomiting, choking, and rumination). Symptoms were considered to be associated with reflux when they occurred within 2 minutes following the onset of a reflux episode, to distinguish between reflux-induced symptoms and those possibly induced by cough.18 Thus, symptoms that occurred within 2 minutes after a reflux event were attributed to reflux, while symptoms that occurred before or more than 2 minutes after reflux were not considered to be reflux related. We calculated the SI and SSI using a computerized system, and they were confirmed by visual analysis by a single investigator.
The SI was calculated as: (total number of reflux-related symptoms/total number of symptom episodes)×100%. SI values ≥50% were considered positive.19,20 The SSI was defined as the probability of symptoms given a reflux event and was calculated as: (total number of reflux-related symptoms/total number of reflux episodes)×100%. SSI values >10% were considered positive.21 As a normal reference for reflux episodes has not been established in any pediatric age group, GERD was diagnosed when the SI or SSI was positive in the present study.
The primary goal of the data analysis was to estimate the frequency of GER and reflux-related respiratory symptoms according to body position. For normally distributed data, a paired t-test was used to analyze continuous variables. For data that were not normally distributed, the Wilcoxon matched-pairs signed-ranks test was applied. All calculated P values were two-sided, and P values <0.05 were taken to indicate statistical significance. Analyses were performed using SPSS version 15.0 (SPSS Inc., Chicago, IL, USA).
MII-pH monitoring was well tolerated by all of the subjects. Of 32 infants with unexplained chronic respiratory symptoms, 15 were diagnosed with GERD. All subjects successfully underwent MII-pH monitoring for at least 18 hours, a mean time of 20.14 hours. A total of 2,129 episodes of reflux were detected: 34.9% (744 episodes) were acid reflux, and 65.1% (1,385 episodes) were non-acid reflux. In addition, 1,239 (58.2%) of the 2,129 episodes of reflux were detected while in the upright position, and 890 (41.8%) were detected while in the recumbent position. Furthermore, 1,443 (67.8%) reflux episodes were detected in the postprandial period; and 686 (32.2%), during the emptying period. Among a total of 416 recorded symptoms, 231 were related to reflux. Of the reflux-related symptoms, 180 were respiratory symptoms, and 51 were other symptoms. The detailed characteristics of the reflux episodes are summarized in Table 1.
The duration of the postprandial period was longer than that of the emptying period (12.36 vs. 7.78 hours; P<0.01; Table 2). There were more reflux episodes during the postprandial period than during the emptying period (45.09 vs. 21.44 episodes; P<0.01), and non-acid reflux was more frequent during the postprandial period (28.91 vs. 14.38 episodes; P<0.01). However, after adjusting for time, the number of non-acid reflux episodes did not differ significantly between the postprandial and emptying periods (2.38 vs. 1.92 episodes/hour; P=0.07).
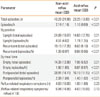
Although both total and non-acid reflux episodes were more frequent in the upright position than in the recumbent position (total reflux: 6.24 vs. 2.06 episodes/hour; P<0.01; non-acid reflux: 4.51 vs. 1.39 episodes/hour; P<0.01), reflux-related respiratory symptoms were less frequent in the upright position (2.54) than the recumbent position (3.03; Table 3). After adjusting for total refluxes, this difference was significant (3.56% vs. 11.36%; P=0.02). In the postprandial period, although the total refluxes per hour did not differ significantly between the upright and recumbent positions (6.12 vs. 3.77 episodes, P=0.10), reflux-related respiratory symptoms per reflux were significantly fewer in the upright than the recumbent position (3.07% vs. 14.75%; P=0.016; Table 4).
Non-acid reflux was more frequent than acid reflux among total episodes (43.28 vs. 23.25; P<0.01), total episodes/hour (2.14 vs. 1.16; P<0.01), episodes/hour in the upright position (4.51 vs. 1.74; P<0.01), and episodes/hour during the postprandial period (2.38 vs. 1.40; P<0.01). Respiratory symptoms related to reflux occurred more frequently with non-acid reflux (4.63) than with acid reflux (1.00; P=0.23; Table 5), although the difference was not significant.
In the present study, we investigated the efficacy of the upright position on GER and reflux-related symptoms as assessed by MII-pH monitoring in 32 infants with chronic respiratory symptoms. Our main findings include the following: (1) overall episodes of reflux were more frequent in the upright position than the recumbent position; (2) despite the high frequency of reflux in the upright position, reflux-related symptoms were more common in the recumbent position; (3) reflux was more frequent during the postprandial period than the emptying period; and (4) non-acid reflux was the predominant form of reflux in infants under 24 months of age.
Mitchell et al.1 reported that conventional pH monitoring misses the majority of reflux episodes and reflux-related symptoms in milk-fed infants. MII-pH monitoring is a sensitive tool for evaluating overall GERD, particularly for the detection of non-acid reflux, and is considered superior to 24-hours pH monitoring alone for the evaluation of the temporal relationship between symptoms and GER.8,22
Upper esophageal sphincter (UES) contraction during transient relaxation of the lower esophageal sphincter is a key protective mechanism against GER. Demeester et al.23 reported that acid reflux occurred more frequently in the upright position, but cleared rapidly from the esophagus. In addition, Blondeau et al.24 reported that the majority of cough-related reflux occurred in an upright position, whereas 24% occurred while in a recumbent position. Previous studies of postural efficacy on GER have reported that reflux occurred more frequently in premature infants positioned in the right lateral decubitus position than the left lateral decubitus position.25-27 These studies found that the right lateral decubitus position caused gastric contents to be above the level of the esophagogastric junction and increased the number of transient lower esophageal sphincter relaxations. Some investigators have reported that the UES usually contracts during transient relaxation of the lower esophageal sphincter in the supine position, but relaxes in the upright position.28 In addition, rapid dilatation of the esophagus induces UES relaxation, and slow dilatation induces UES contraction.28,29 Babaei et al.30 reported that air reflux in the upright position induces rapid distension of the esophagus and UES relaxation, and liquid reflux in the recumbent position induces slow distension of the esophagus and UES constriction in healthy adults. However, there is little information regarding reflux in young children and infants, who frequently get fed liquid diets and who are most often in a recumbent position.
There are two possible mechanisms to explain the relationship between GER and reflux-related respiratory symptoms: a direct inflammatory effect through microaspiration,31 or an indirect effect through esophageal distension and vagal stimulation.13,32 Rosen et al.13 reported that proximal reflux is strongly associated with respiratory symptoms (OR, 1.31; 95% CI, 1.01-1.69) and that 75% of non-acid reflux, compared with 8.8% of acid reflux, reaches the proximal esophagus in children with persistent respiratory symptoms and who take antacid medications. That study also showed that 13% of proximal reflux was related to symptoms, and 20% of reflux-related symptoms was related to distal reflux. Thus, both mechanisms may have a role in reflux-related symptoms. Another study reported that 33% of acid reflux was associated with symptoms, with a 77% SSI for proximal acid reflux.33 The association between respiratory symptoms and proximal reflux remains unclear.34 In our study, consistent with clinical practice, infants remained in an upright position during the postprandial period in order to investigate its efficacy. In the upright position, reflux was more frequent during the postprandial period, while reflux-related respiratory symptoms were less frequent, indicating that the upright position may reduce reflux-related symptoms, rather than reflux frequency. Although the height of the reflux bolus was not analyzed in our study, our results suggest that the upright position may reduce the height of reflux. The present findings showed a mean of 66.53 episodes of reflux, although a higher prevalence of reflux has been reported in previous studies.15,35 Our results support the idea that the upright position reduces reflux.
Condino et al.22 found that the proportion of non-acid reflux decreased from 61% during the first postprandial hour to 39% during the second postprandial hour and finally to 29% after two hours; in addition, the proportion of non-acid reflux decreased with age. Other studies have reported similar results, including that 37% of cough-related reflux occurs in the first hour after a meal,24 and that non-acid reflux comprises one-third of all reflux events in adults and frequently occurs soon after a meal.36 In infants, gastric acidity is neutralized by milk or milk formula during the postprandial period.8,10 Therefore, detection and analysis of non-acid reflux and its association with symptoms during the postprandial period may be critical in the diagnosis and treatment of infants with suspected GER. Previous studies have shown that non-acid or weakly acidic reflux occurs in 45% and 90% of children and infants.12,13 Rosen et al.13 reported that 45% of GER events were non-acidic and that respiratory symptoms were frequently (38%) associated with reflux, more strongly with non-acid reflux than acid reflux, in children with persistent respiratory symptoms. Wenzl et al.12 also reported that apnea in infants with recurrent respiratory symptoms is associated with GER, particularly with non-acid reflux. However, Mousa et al. reported no difference in the frequency of acid versus non-acid gastroesophageal reflux associated with apnea.14 Thilmany et al.15 reported that in 25 children aged 6 months to 15 years with unexplained chronic cough, non-acid reflux played only a minor role because it was very infrequent.
The proportion of episodes of non-acid reflux and its relationship with symptoms is still unclear. As the wide range of findings has been attributed to variations among study cohorts, we conducted the current study using well-defined enrollment and exclusion criteria. Our findings showed that non-acid reflux was the predominant type of reflux in young children and infants, regardless of body position or meal time. The safety concerns for pharmacological therapy in this age group are still unresolved.37 Therefore, non-pharmacological therapy may be considered as the first-line therapeutic strategy in infants with GERD.
The major strengths of our study include applying the proper exclusion criteria and study protocol and including subjects who were resistant to acid suppressants. This allowed us to investigate the efficacy of the upright position on non-acid reflux without confounding factors. In addition, we applied the upright position using a baby car seat at a 30-degree angle, which is considered to be the only possible intervention in clinical practice. Furthermore, the reflux-symptom association was visually analyzed by a primary investigator to confirm the findings. In our study design, cough-induced reflux and non-reflux-related symptoms could be excluded.
Our study has some limitations. There are no normal reference values for reflux in infants to use for comparison.8 Although we diagnosed 15 subjects with GER based on SI or SSI positivity, some infants who exhibited certain reflux-related respiratory symptoms were SI and SSI negative. Owing to a lack of normal references for reflux in any pediatric age group, symptom-reflux association analyses have reported poor inter-parameter associations.38 This limits clinically relevant investigations. Normal MII-pH values in pediatric age groups should be established as the gold standard for a diagnosis of GERD. Another limitation of our study was the small number of subjects, which resulted from our strict enrollment and exclusion criteria. Furthermore, because symptoms during MII-pH monitoring were recorded by the patients' parents, some symptoms might have been missed or recorded late. Blondeau et al.24 suggested that an objective technique for cough detection is necessary to improve symptom association analysis. Finally, although all infants were maintained in the upright position during the postprandial period, the time spent in the upright position differed significantly according to age, such that younger infants (<6 months, n=19) were in the upright position longer than older infants (≥6 months, n=13) (8.4 hours vs. 5.2 hours, P=0.03; data not shown). This may be attributable to an uncomfortable baby car seat or less frequent meal times for older infants. We were unable to analyze the effect of the upright position according to age because of the small sample size of each subset. Future studies should include a larger cohort of patients.
In conclusion, our findings suggest that the upright position reduces reflux-related respiratory symptoms, rather than reflux itself. In addition, reflux-related respiratory symptoms were more frequent with non-acid reflux than with acid reflux. Non-pharmacological interventions such as maintaining an upright position may be useful alternative treatments for infantile GER disease that is resistant to acid suppressants.
Figures and Tables
Table 2
Comparison of reflux characteristics between the postprandial period and empty period in 32 infants with unexplained chronic respiratory symptoms
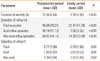
Table 3
Comparison of reflux characteristics between the upright position and recumbent position in 32 infants with unexplained chronic respiratory symptoms

References
1. Mitchell DJ, McClure BG, Tubman TR. Simultaneous monitoring of gastric and oesophageal pH reveals limitations of conventional oesophageal pH monitoring in milk fed infants. Arch Dis Child. 2001. 84:273–276.
2. Thomson M. Disorders of the oesophagus and stomach in infants. Baillieres Clin Gastroenterol. 1997. 11:547–571.
3. Nelson SP, Chen EH, Syniar GM, Christoffel KK. Prevalence of symptoms of gastroesophageal reflux during infancy. A pediatric practice-based survey. Arch Pediatr Adolesc Med. 1997. 151:569–572.
4. Harding SM, Guzzo MR, Richter JE. The prevalence of gastroesophageal reflux in asthma patients without reflux symptoms. Am J Respir Crit Care Med. 2000. 162:34–39.
5. Buts JP, Barudi C, Moulin D, Claus D, Cornu G, Otte JB. Prevalence and treatment of silent gastro-oesophageal reflux in children with recurrent respiratory disorders. Eur J Pediatr. 1986. 145:396–400.
6. Tolia V, Vandenplas Y. Systematic review: the extra-oesophageal symptoms of gastro-oesophageal reflux disease in children. Aliment Pharmacol Ther. 2009. 29:258–272.
7. Kiljander TO, Salomaa ER, Hietanen EK, Terho EO. Chronic cough and gastro-oesophageal reflux: a double-blind placebo-controlled study with omeprazole. Eur Respir J. 2000. 16:633–638.
8. Mousa HM, Rosen R, Woodley FW, Orsi M, Armas D, Faure C, Fortunato J, O'Connor J, Skaggs B, Nurko S. Esophageal impedance monitoring for gastroesophageal reflux. J Pediatr Gastroenterol Nutr. 2011. 52:129–139.
9. Washington N, Steele RJ, Jackson SJ, Washington C, Bush D. Patterns of food and acid reflux in patients with low-grade oesophagitis--the role of an anti-reflux agent. Aliment Pharmacol Ther. 1998. 12:53–58.
10. Del Buono R, Wenzl TG, Ball G, Keady S, Thomson M. Effect of Gaviscon Infant on gastro-oesophageal reflux in infants assessed by combined intraluminal impedance/pH. Arch Dis Child. 2005. 90:460–463.
11. DeVault KR, Castell DO. Updated guidelines for the diagnosis and treatment of gastroesophageal reflux disease. Am J Gastroenterol. 2005. 100:190–200.
12. Wenzl TG, Schenke S, Peschgens T, Silny J, Heimann G, Skopnik H. Association of apnea and nonacid gastroesophageal reflux in infants: Investigations with the intraluminal impedance technique. Pediatr Pulmonol. 2001. 31:144–149.
13. Rosen R, Nurko S. The importance of multichannel intraluminal impedance in the evaluation of children with persistent respiratory symptoms. Am J Gastroenterol. 2004. 99:2452–2458.
14. Mousa H, Woodley FW, Metheney M, Hayes J. Testing the association between gastroesophageal reflux and apnea in infants. J Pediatr Gastroenterol Nutr. 2005. 41:169–177.
15. Thilmany C, Beck-Ripp J, Griese M. Acid and non-acid gastro-esophageal refluxes in children with chronic pulmonary diseases. Respir Med. 2007. 101:969–976.
16. Vela MF, Camacho-Lobato L, Srinivasan R, Tutuian R, Katz PO, Castell DO. Simultaneous intraesophageal impedance and pH measurement of acid and nonacid gastroesophageal reflux: effect of omeprazole. Gastroenterology. 2001. 120:1599–1606.
17. Sifrim D, Castell D, Dent J, Kahrilas PJ. Gastro-oesophageal reflux monitoring: review and consensus report on detection and definitions of acid, non-acid, and gas reflux. Gut. 2004. 53:1024–1031.
18. Laukka MA, Cameron AJ, Schei AJ. Gastroesophageal reflux and chronic cough: which comes first? J Clin Gastroenterol. 1994. 19:100–104.
19. Aanen MC, Bredenoord AJ, Numans ME, Samson M, Smout AJ. Reproducibility of symptom association analysis in ambulatory reflux monitoring. Am J Gastroenterol. 2008. 103:2200–2208.
20. Bredenoord AJ, Weusten BL, Smout AJ. Symptom association analysis in ambulatory gastro-oesophageal reflux monitoring. Gut. 2005. 54:1810–1817.
21. Breumelhof R, Smout AJ. The symptom sensitivity index: a valuable additional parameter in 24-hour esophageal pH recording. Am J Gastroenterol. 1991. 86:160–164.
22. Condino AA, Sondheimer J, Pan Z, Gralla J, Perry D, O'Connor JA. Evaluation of infantile acid and nonacid gastroesophageal reflux using combined pH monitoring and impedance measurement. J Pediatr Gastroenterol Nutr. 2006. 42:16–21.
23. Demeester TR, Johnson LF, Joseph GJ, Toscano MS, Hall AW, Skinner DB. Patterns of gastroesophageal reflux in health and disease. Ann Surg. 1976. 184:459–470.
24. Blondeau K, Mertens V, Dupont L, Pauwels A, Farré R, Malfroot A, De Wachter E, De Schutter I, Hauser B, Vandenplas Y, Sifrim D. The relationship between gastroesophageal reflux and cough in children with chronic unexplained cough using combined impedance-pH-manometry recordings. Pediatr Pulmonol. 2011. 46:286–294.
25. Omari TI, Rommel N, Staunton E, Lontis R, Goodchild L, Haslam RR, Dent J, Davidson GP. Paradoxical impact of body positioning on gastroesophageal reflux and gastric emptying in the premature neonate. J Pediatr. 2004. 145:194–200.
26. van Wijk MP, Benninga MA, Dent J, Lontis R, Goodchild L, McCall LM, Haslam R, Davidson GP, Omari T. Effect of body position changes on postprandial gastroesophageal reflux and gastric emptying in the healthy premature neonate. J Pediatr. 2007. 151:585–590. 590.e1–590.e2.
27. Corvaglia L, Rotatori R, Ferlini M, Aceti A, Ancora G, Faldella G. The effect of body positioning on gastroesophageal reflux in premature infants: evaluation by combined impedance and pH monitoring. J Pediatr. 2007. 151:591–596. 596.e1
28. Gerhardt DC, Shuck TJ, Bordeaux RA, Winship DH. Human upper esophageal sphincter. Response to volume, osmotic, and acid stimuli. Gastroenterology. 1978. 75:268–274.
29. Kahrilas PJ, Dodds WJ, Dent J, Wyman JB, Hogan WJ, Arndorfer RC. Upper esophageal sphincter function during belching. Gastroenterology. 1986. 91:133–140.
30. Babaei A, Bhargava V, Mittal RK. Upper esophageal sphincter during transient lower esophageal sphincter relaxation: effects of reflux content and posture. Am J Physiol Gastrointest Liver Physiol. 2010. 298:G601–G607.
31. Oue K, Mukaisho K, Higo T, Araki Y, Nishikawa M, Hattori T, Yamamoto G, Sugihara H. Histological examination of the relationship between respiratory disorders and repetitive microaspiration using a rat gastro-duodenal contents reflux model. Exp Anim. 2011. 60:141–150.
32. Canning BJ. Role of nerves in asthmatic inflammation and potential influence of gastroesophageal reflux disease. Am J Med. 2001. 111:Suppl 8A. 13S–17S.
33. Jadcherla SR, Gupta A, Fernandez S, Nelin LD, Castile R, Gest AL, Welty S. Spatiotemporal characteristics of acid refluxate and relationship to symptoms in premature and term infants with chronic lung disease. Am J Gastroenterol. 2008. 103:720–728.
34. Condino AA, Sondheimer J, Pan Z, Gralla J, Perry D, O'Connor JA. Evaluation of gastroesophageal reflux in pediatric patients with asthma using impedance-pH monitoring. J Pediatr. 2006. 149:216–219.
35. Patra S, Singh V, Chandra J, Kumar P, Tripathi M. Gastro-esophageal reflux in early childhood wheezers. Pediatr Pulmonol. 2011. 46:272–277.
36. Sifrim D, Holloway R, Silny J, Tack J, Lerut A, Janssens J. Composition of the postprandial refluxate in patients with gastroesophageal reflux disease. Am J Gastroenterol. 2001. 96:647–655.
37. Orenstein SR, Shalaby TM, Devandry SN, Liacouras CA, Czinn SJ, Dice JE, Simon TJ, Ahrens SP, Stauffer LA. Famotidine for infant gastro-oesophageal reflux: a multi-centre, randomized, placebo-controlled, withdrawal trial. Aliment Pharmacol Ther. 2003. 17:1097–1107.
38. Lüthold SC, Rochat MK, Bähler P. Disagreement between symptom-reflux association analysis parameters in pediatric gastroesophageal reflux disease investigation. World J Gastroenterol. 2010. 16:2401–2406.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download