Abstract
Purpose
Aspirin and non-steroidal anti-inflammatory drugs (ASA/NSAIDs) are common causes of drug hypersensitivity. An oral provocation test is the only definitive diagnostic test. This study assessed the reliability of a flow cytometry-assisted basophil activation test (FAST) as a safe diagnostic method for ASA/NSAID-induced hypersensitivity, as its high sensitivity and specificity have been demonstrated for many other drugs.
Methods
Eighteen patients and 11 controls were enrolled. Using a Flow-CAST kit® (Bühlmann Laboratories AG, Schönenbuch, Switzerland), 29 analyses with aspirin, ibuprofen, and diclofenac were performed by flow cytometry to detect double-positive staining of anti-IgE and anti-CD63. The stimulation index was defined as the activated basophil percentage after drug stimulation/basally active basophil percentage. A stimulation index≥2 and an absolute activated basophil percentage≥5 were considered positive.
The prevalence of drug hypersensitivity reactions is increasing. Detection of the culprit drug is a prerequisite for effective prevention by substituting safer alternatives. Aspirin and non-steroidal anti-inflammatory drugs (ASA/NSAIDs) are among the most common causes of hypersensitivity reactions, accounting for 0.6%-2.5% of hypersensitivity reactions in the general population and 10%-20% in asthmatic patients.1,2 A previous study at a tertiary care hospital in Korea reported that ASA/NSAIDs ranked first among the drugs provoking hypersensitivity reactions.3 Nevertheless, a definitive diagnosis of ASA/NSAID-induced hypersensitivity is difficult because these are usually administered in combination with other drugs, making it necessary to test all drugs taken. Although hypersensitivity reactions to some drugs can be detected by topical provocation tests, reactions to ASA/NSAIDs, except for aspirin-induced asthma, can be detected only by an oral provocation test. However, oral provocation tests are contraindicated in subjects who have experienced severe reactions such as anaphylactic shock,4 and many subjects who have experienced drug hypersensitivity reactions are not willing to risk an oral provocation test.
Numerous methods have been proposed to diagnose ASA/NSAIDs hypersensitivity. In vivo methods include the skin prick test (SPT),5 the autologous serum skin test,6,7 and measurement of urine leukotriene E4 before and after ingestion of the suspected drug.8 In vitro, analysis of genetic polymorphisms related to metabolism of arachidonic acid,9,10 measurement of 15-HETE in the reaction between ASA/NSAIDs and leukocytes,11 and the cellular allergen stimulation test (CAST) using basophils12,13 have been investigated.
Here, we used a flow cytometry-assisted basophil activation test (FAST) to analyze CD63 exposure upon basophil degranulation. CD63 is anchored in the basophilic granular membrane and can be detected on the outside of the cell upon the fusion of granules with plasma membranes.14 FAST has high sensitivity and specificity for the diagnosis of hypersensitivity reactions to inhalant allergens, bee venom, and latex.15 Some studies on hypersensitivity to ASA/NSAIDs have found high specificity of FAST,18-20 but reported sensitivities vary.
The present study was conducted to corroborate the applicability of FAST for detecting hypersensitivity to ASA/NSAIDs and to evaluate its efficacy in Koreans by determining its sensitivity, specificity, and positive/negative predictive values.
This study included 18 patients who showed hypersensitivity reactions to ASA/NSAIDs at our allergy clinic between August 2007 and August 2008. Skin reactions were provoked in 13 subjects; respiratory reactions, in two; and anaphylactic shock, in three. The control group comprised 11 subjects who were matched for age and gender (ratio, 2:1) with the study group. The control subjects were patients admitted with other diseases (n=5) or were healthy subjects (n=3). Three subjects who showed hypersensitivity reactions to drugs other than ASA/NSAIDs were also included as controls. We confirmed that the control subjects had experienced no hypersensitivity reactions to ASA/NSAIDs. All subjects were informed orally about the study and provided informed consent. The study was approved by the local institutional review board.
Clinical features, including the types of drugs producing hypersensitivity reactions, time interval from drug ingestion to symptom onset, and types of hypersensitivity reactions, as well as past histories of bronchial asthma, allergic rhinitis, food allergy, and chronic urticaria, were collected for each subject. Serum total IgE was measured, and specific IgE was determined using the multiple allergen simultaneous test (MAST). SPTs were performed for common inhalant and food allergens, and atopy was defined as a positive SPT result.
Blood samples were drawn from the subjects at least 2 weeks after hypersensitivity reactions and also at least 1 week after discontinuation of anti-allergic medications such as antihistamines, antileukotrienes, and steroids. The cells were stimulated within 2 hours after blood sampling, or the samples were immediately refrigerated for up to 24 hours. Experiments were performed using a commercially available Flow-CAST kit® (Bühlmann Laboratories AG, Schönenbuch, Switzerland) following the manufacturer's instructions, as has been fully described and discussed elsewhere.14-23
For analysis, blood was collected in an EDTA tube and centrifuged for 5 minutes at 1,100 rpm. The leukocyte-containing plasma fraction was then centrifuged for 10 minutes at 1,700 rpm to obtain a leukocyte pellet, which was carefully resuspended with 100 µL of stimulation buffer per 1 mL of original blood sample. Each patient's cell suspension was divided among five test tubes (50 µL per tube). Stimulation buffer was added to one tube as a negative control; anti-IgE receptor antibody was added to another tube as a positive control. To the remaining three tubes, 50 µL of aspirin (1.25 mg/mL), ibuprofen (50 µg/mL), or diclofenac (12.5 µg/mL) were added. The tubes were vortexed gently and incubated at 37℃ for 40 minutes. The reaction was halted by adding 50 µL of pre-cooled blocking buffer to each tube. Leukocytes were labeled using FITC-conjugated anti-IgE and PE-conjugated anti-CD 63.
The samples were analyzed using CellQuest® containing 488nm argon within 2 hours. The cutoff points for anti-IgE-FITC and anti-CD63-PE were determined for each subject based on the point where the initial fluorescence peak was observed in the positive control (Fig. 1). The percentage of basophils positive for both IgE and CD 63 was obtained. The stimulation index (SI) was calculated using the following formula:
SI=percentage of basophils activated by the drug/percentage of activated basophils in the negative control
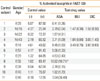
The receiver operating characteristics (ROC) curve was used to determine a cutoff point for the SI. A positive result was defined as a SI≥2 (Fig. 2), which was similar to previous studies.18-21,23 To account for nonspecific activation, only activated basophil percentages≥5% were considered positive.
Statistical analysis was performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). As the number of subjects was small, continuous variables were analyzed using the Mann-Whitey U test, and categorical variables were analyzed using Fisher's exact test. A P value<0.05 was considered to indicate significance. The FAST results are expressed as the percentage of basophils positive for both IgE and CD63.
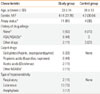
Table 1 presents the demographic and clinical characteristics of the study and control groups. The ratio of males to females in the study group was 1:3.5, and the prevalence of atopy was significantly higher in the study group than in control group (61% vs. 36%; P<0.05). Eight of the 18 study subjects (44%) had previously experienced hypersensitivity reactions to ASA/NSAIDs. Of these eight, one had also experienced hypersensitivity to a drug other than ASA/NSAIDs (an iron preparation). In the control group, two subjects had a history of hypersensitivity to penicillin; and one, to cimetidine. Culprit drugs for the current reactions in the study group were aspirin (n=6), propionic acid derivatives (ibuprofen, naproxen; n=8), acetic acid derivatives (diclofenac, aceclofenac; n=2), piroxicam (n=1), and Joins® (Clematis mandshurica, Trichosanthes kirilowii, Prunella vulgaris; n=1).
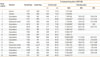
The FAST results are shown in Tables 2 and 3. There was no significant difference in the mean FAST result for the negative test control (3.26%±1.68% vs. 2.25%±1.93%) or positive test control (73.73%±19.78% vs. 63.91%±26.03%) between the study and control groups. The FAST results showed a specificity of 91%, positive predictability of 92%, sensitivity of 61%, and negative predictability of 59%.
For patients with hypersensitivity reactions to salicylate, the FAST results for aspirin were positive in 50%. All patients who showed hypersensitivity to propionic derivatives and acetic acid derivatives showed a negative response to ibuprofen and diclofenac, respectively.
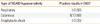
Within the study group, atopy status did not affect the FAST results. The FAST results did not differ significantly between study subjects with cutaneous symptoms and those with respiratory symptoms, or between those with mild symptoms and those with severe symptoms (Table 4).
The aim of the present study was to evaluate the efficacy of FAST for the diagnosis of hypersensitivity to ASA/NSAIDs. There are many reports in the European literature regarding the use of FAST to test reactivity to ASA/NSAIDs,18-21 diclofenac,22 or metamizol.23 These studies applied a SI≥2 as a cutoff on the basis of high specificity under the ROC curve, because the prevalence of hypersensitivity reactions to ASA/NSAIDs was relatively low. Although the specificity and positive predictive value were reported to be 100% in all of these previous studies, the sensitivity varied between 40% and 70%.18-23
In the present study using a SI cutoff of 2, FAST showed a specificity of 91%, positive predictive value of 92%, sensitivity of 6%, and negative predictive value of 59%. The SI cutoff point, sensitivity, and specificity were similar to those in previous studies.18-23 Neither atopy status nor the type and severity of hypersensitivity reactions affected the FAST results, which was also similar to previous results.18,21
Two earlier studies demonstrated that 27%-66% of subjects with hypersensitivity to one ASA/NSAID showed a positive FAST result with other ASA/NSAIDs. However, similar results were not obtained in the present study, probably owing to the small sample size.
In the present study, the specificity was relatively low, and all subjects showed positive FAST results only for aspirin, regardless of the culprit drug. The control subject who showed a positive FAST result had a negative oral aspirin provocation test result. The discrepancy between the results of previous European studies and ours may be explained by differences in race and/or drug concentration.
We employed commercially available concentrations of drugs based on the dose-reaction relationship. The concentrations of aspirin used in this study were similar to those used in previous studies, and the sensitivity and specificity were also similar. Previous studies tested with 1-100 µg/mL of ibuprofen and 1-310 µg/mL of diclofenac, and one study reported a sensitivity of 29% for ibuprofen and 50% for diclofenac at concentrations lower than those used here.21 The maximum blood concentrations in vivo after ingestion of the medications were 15-55 and 0.5-2.5 µg/mL for ibuprofen and diclofenac, respectively.25 These values are lower than those obtained in our study. One report concluded that the use of higher drug concentrations appeared to increase the sensitivity of FAST because the high drug doses induced nonspecific basophil activation.26 We infer that in the present study, the drug concentrations did not affect the FAST results.
The low sensitivity of 65% for ASA/NSAID-induced hypersensitivity may be a drawback of FAST. Two studies from the U.S. and Turkey showed negative FAST results.26,27 The U.S. study reported sensitivities of 30% for aspirin at 0.3-1.25 mg/mL and 80% at 5 mg/mL; however, high aspirin concentrations also stimulated basophils in the control group, indicating poor specificity.26 The Turkish study found very low sensitivity (16.7%-33.3%).27 The low sensitivities may be attributable to the fact that mast cells and eosinophils are also involved in hypersensitivity reactions to ASA/NSAIDs. There is no direct evidence for the involvement of basophils in ASA/NSAIDs hypersensitivity, although many studies have demonstrated increased levels of leukotriene C4 (LTC4) in serum and bronchial and nasal secretions, as well as LTE4 and 15-HETE in urine, after aspirin challenge in hypersensitive patients. LTC4, which is a mainstay of ASA/NSAID-induced hypersensitivity, is produced by LTC4 synthase, which is distributed mainly in mast cells and basophils. These cells contain many glycogen granules filled with various chemical mediators, including histamine, and are degranulated by direct or indirect stimulation, with subsequent induction of immediate-type hypersensitivity reactions.24
There are several confounding factors derived from the heterogeneous study and control subjects in the present study. Further investigations with a larger sample size, particularly including subjects with hypersensitivity reactions of the respiratory system, and studies aiming to establish the relationship between FAST results and ethnic groups are needed to confirm our results.
The sensitivity of FAST must be improved before it can be applied for the clinical evaluation of drug sensitivity reactions. For example, additional studies have been explored the use of a combination of anaphylatoxin12 and simultaneous measurement of CD63 and CD20326-29 or CRTH2/DP2.30 With improved sensitivity, FAST may provide a safe, convenient, and rapid method for the diagnosis of hypersensitivity to ASA/NSAIDs.
Figures and Tables
Fig. 1
Representative aspirin hypersensitivity results. (A) The cutoff point (arrow) for anti-CD63-PE was established according to the initiation of a fluorescence peak in the positive control. Shaded histogram, negative control (stimulation buffer); solid gray lines, positive control (anti-FcεRI antibody). (B) A sample stimulated with aspirin showing activation of 25.69% of basophils. (C) A sample stimulated with ibuprofen showing activation of 2.11% of basophils. (D) A sample stimulated with diclofenac showing activation of 4.57% of basophils. The SI of aspirin was >2, indicating a positive result. The percentage of activated basophils was low (<5%) upon stimulation with ibuprofen or diclofenac, indicating a negative result for each.

Fig. 2
The receiver operating characteristics (ROC) curve. According to the ROC curve, the optimal cutoff point for the stimulation index was 1.9 (arrow). The observed area under the curve was 0.72 (95% Confidence Interval, 0.53-0.93; P=0.039), which is considered fair.

References
1. Szczeklik A, Stevenson DD. Aspirin-induced asthma: advances in pathogenesis, diagnosis, and management. J Allergy Clin Immunol. 2003. 111:913–921.
2. Kasper L, Sladek K, Duplaga M, Bochenek G, Liebhart J, Gladysz U, Malolepszy J, Szczeklik A. Prevalence of asthma with aspirin hypersensitivity in the adult population of Poland. Allergy. 2003. 58:1064–1066.
3. Choi JH, Shin YS, Suh CH, Nahm DH, Park HS. The frequency of adverse drug reactions in a tertiary care hospital in Korea. Korean J Med. 2004. 67:290–296.
4. Nizankowska-Mogilnicka E, Bochenek G, Mastalerz L, Swierczyńska M, Picado C, Scadding G, Kowalski ML, Setkowicz M, Ring J, Brockow K, Bachert C, Wöhrl S, Dahlén B, Szczeklik A. EAACI/GA2LEN guideline: aspirin provocation tests for diagnosis of aspirin hypersensitivity. Allergy. 2007. 62:1111–1118.
5. Palma-Carlos AG, Medina M, Palma-Carlos ML. Skin tests in NSAIDS hypersensitivity. Eur Ann Allergy Clin Immunol. 2006. 38:182–185.
6. Asero R. Predictive value of autologous plasma skin test for multiple nonsteroidal anti-inflammatory drug intolerance. Int Arch Allergy Immunol. 2007. 144:226–230.
7. Asero R, Tedeschi A, Lorini M. Autoreactivity is highly prevalent in patients with multiple intolerances to NSAIDs. Ann Allergy Asthma Immunol. 2002. 88:468–472.
8. Mastalerz L, Setkowicz M, Sanak M, Szczeklik A. Hypersensitivity to aspirin: common eicosanoid alterations in urticaria and asthma. J Allergy Clin Immunol. 2004. 113:771–775.
9. Kim SH, Jeong HH, Cho BY, Kim M, Lee HY, Lee J, Wee K, Park HS. Association of four-locus gene interaction with aspirin-intolerant asthma in Korean asthmatics. J Clin Immunol. 2008. 28:336–342.
10. Choi JH, Lee KW, Oh HB, Lee KJ, Suh YJ, Park CS, Park HS. HLA association in aspirin-intolerant asthma: DPB1*0301 as a strong marker in a Korean population. J Allergy Clin Immunol. 2004. 113:562–564.
11. Kowalski ML, Ptasinska A, Jedrzejczak M, Bienkiewicz B, Cieslak M, Grzegorczyk J, Pawliczak R, Dubuske L. Aspirin-triggered 15-HETE generation in peripheral blood leukocytes is a specific and sensitive Aspirin-Sensitive Patients Identification Test (ASPITest). Allergy. 2005. 60:1139–1145.
12. May A, Weber A, Gall H, Kaufmann R, Zollner TM. Means of increasing sensitivity of an in vitro diagnostic test for aspirin intolerance. Clin Exp Allergy. 1999. 29:1402–1411.
13. Pierzchalska M, Mastalerz L, Sanak M, Zazula M, Szczeklik A. A moderate and unspecific release of cysteinyl leukotrienes by aspirin from peripheral blood leucocytes precludes its value for aspirin sensitivity testing in asthma. Clin Exp Allergy. 2000. 30:1785–1791.
14. Boumiza R, Debard AL, Monneret G. The basophil activation test by flow cytometry: recent developments in clinical studies, standardization and emerging perspectives. Clin Mol Allergy. 2005. 3:9.
15. Ebo DG, Bridts CH, Hagendorens MM, Aerts NE, De Clerck LS, Stevens WJ. Basophil activation test by flow cytometry: present and future applications in allergology. Cytometry B Clin Cytom. 2008. 74:201–210.
16. Torres MJ, Padial A, Mayorga C, Fernández T, Sanchez-Sabate E, Cornejo-García JA, Antúnez C, Blanca M. The diagnostic interpretation of basophil activation test in immediate allergic reactions to betalactams. Clin Exp Allergy. 2004. 34:1768–1775.
17. Monneret G, Benoit Y, Debard AL, Gutowski MC, Topenot I, Bienvenu J. Monitoring of basophil activation using CD63 and CCR3 in allergy to muscle relaxant drugs. Clin Immunol. 2002. 102:192–199.
18. Gamboa P, Sanz ML, Caballero MR, Urrutia I, Antépara I, Esparza R, de Weck AL. The flow-cytometric determination of basophil activation induced by aspirin and other non-steroidal anti-inflammatory drugs (NSAIDs) is useful for in vitro diagnosis of the NSAID hypersensitivity syndrome. Clin Exp Allergy. 2004. 34:1448–1457.
19. Sanz ML, Gamboa P, de Weck AL. A new combined test with flowcytometric basophil activation and determination of sulfidoleukotrienes is useful for in vitro diagnosis of hypersensitivity to aspirin and other nonsteroidal anti-inflammatory drugs. Int Arch Allergy Immunol. 2005. 136:58–72.
20. Sainte-Laudy J, Touraine F, Boumediene A, Bonnaud F, Cogné M. Clinico-biological characteristics of flow cytometry applied to hypersensitivity to NSAIDs. Inflamm Res. 2007. 56:Suppl 1. S63–S64.
21. Rodríguez-Trabado A, Cámara-Hijón C, Ramos-Cantariño A, Porcel-Carreño SL, Jiménez-Timón S, Pereira-Navarro G, Hernández-Arbeiza FJ, Fernández-Pereira L. Basophil activation test for the in vitro diagnosis of nonsteroidal anti-inflammatory drug hypersensitivity. Allergy Asthma Proc. 2008. 29:241–249.
22. Malbrán A, Yeyati E, Rey GL, Galassi N. Diclofenac induces basophil degranulation without increasing CD63 expression in sensitive patients. Clin Exp Immunol. 2007. 147:99–105.
23. Gamboa PM, Sanz ML, Caballero MR, Antépara I, Urrutia I, Jáuregui I, González G, Diéguez I, De Weck AL. Use of CD63 expression as a marker of in vitro basophil activation and leukotriene determination in metamizol allergic patients. Allergy. 2003. 58:312–317.
24. Adkinson NF, Yunginger JW, Busse WW, Bochner BS, Holgate ST, Simons FER. Middleton's allergy: principles & practice. 2003. 6th ed. Philadelphia: Mosby;1695–1710.
25. McEvoy GK. AHFS drug information. 2006. Wisconsin: American Society of Health-System Pharmacists;2010. 2021. 2038.
26. Celik GE, Schroeder JT, Hamilton RG, Saini SS, Adkinson NF. Effect of in vitro aspirin stimulation on basophils in patients with aspirin-exacerbated respiratory disease. Clin Exp Allergy. 2009. 39:1522–1531.
27. Bavbek S, Ikincioğullari A, Dursun AB, Guloğlu D, Arikan M, Elhan AH, Misirligil Z. Upregulation of CD63 or CD203c alone or in combination is not sensitive in the diagnosis of nonsteroidal anti-inflammatory drug intolerance. Int Arch Allergy Immunol. 2009. 150:261–270.
28. Boumiza R, Monneret G, Forissier MF, Savoye J, Gutowski MC, Powell WS, Bienvenu J. Marked improvement of the basophil activation test by detecting CD203c instead of CD63. Clin Exp Allergy. 2003. 33:259–265.
29. Sainte-Laudy J, Belon P. Improvement of flow cytometric analysis of basophil activation inhibition by high histamine dilutions. A novel basophil specific marker: CD 203c. Homeopathy. 2006. 95:3–8.
30. Ebo DG, Sainte-Laudy J, Bridts CH, Mertens CH, Hagendorens MM, Schuerwegh AJ, De Clerck LS, Stevens WJ. Flow-assisted allergy diagnosis: current applications and future perspectives. Allergy. 2006. 61:1028–1039.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download