Abstract
Purpose
Asthma-related morbidity and mortality are increasing, and the financial burden imposed by this condition will substantially increase. Nevertheless, little information is available regarding the nature and magnitude of the burden due to asthma at the national level. This study was conducted to characterize the financial burden imposed by asthma in the Republic of Korea at the national level.
Methods
The overall prevalence of asthma and the costs of related medical services were determined using data from the National Health Insurance Corporation, which is responsible for the National Health Insurance scheme. Indirect costs, including expenditures on complementary and alternative medicines, and the economic impact of an impaired quality of life (intangible costs) were estimated by surveying 660 asthmatics, and these estimates were transformed to the national level using the prevalence of asthma.
Results
The prevalence of asthma and total costs related to the disease in 2004 were 4.19% and $2.04 billion, respectively. Direct costs and indirect costs contributed equally to total costs (46.9% and 53.1%, respectively). However, when intangible costs were included, total costs rose to $4.11 billion, which was equivalent to 0.44% of the national gross domestic product in 2004.
The morbidity, mortality, and costs associated with asthma are imposing an ever increasing burden on society. Evidence obtained worldwide indicates that health care costs related to asthma represent a large percentage of health care expenditures.1-7 Nevertheless, little reliable information is available regarding the nature and magnitude of the burden imposed by asthma at the national level in the Republic of Korea. Furthermore, the lack of a unified health care system means that nationwide surveys are not feasible, and as a result, the majority of previous estimations were based on secondary data, expert opinions, or small-scale surveys.1-3,5,6 Consequently, estimations of the cost of asthma vary widely.8
Owing to the chronic and incurable, but not life-threatening, nature of asthma, one goal of asthma control is improving quality of life (QOL).9,10 The use of complementary and alternative medicines (CAMs) is common among asthmatics,11 ranging from 33% to 51% of asthmatics in Europe.12-14 However, the true economic impact of impaired QOL in asthmatics and the amount spent on CAMs beyond the official health care system have not been properly estimated.
The present study was undertaken to determine the financial burden of asthma in the Republic of Korea, where enrollment in the National Health Insurance Corporation [NHIC, a single payer for National Health Insurance (NHI)] is compulsory; thus, the NHIC covers the whole nation.15 The main sources of the information used in this study were health insurance claims data from the NHIC, which enabled us to estimate the nationwide financial burden of asthma. We also estimated the economic impact of impaired QOL (intangible costs) using the willingnessto-pay (WTP) method and the amount spent on CAMs. To our knowledge, this is the first estimate of the economic impacts of impaired QOL and CAMs related to asthma at the national level in the Republic of Korea.
We identified subjects with asthma as a main diagnosis by searching the NHIC data base for codes J45 and J46 of the International Classification of Diseases-Tenth Revision (ICD-10)16 associated with any medical event (i.e., hospitalization, office/clinic visit, emergency room visit, or pharmacy visit). We then analyzed insurance claim data for the period 1 January to 31 December 2003 to determine asthma prevalence.
Asthma was diagnosed and its severity was determined based on spirometry results, in accordance with international guidelines.17 All patients with asthma were randomly recruited by allergy specialists who were chosen to represent a range of professional (university, general, and private clinics) and geographical (metropolitan and non-metropolitan) settings throughout the Republic of Korea. At the initial visit, the patient, or the patient's parent for patients younger than 15 years of age, completed a questionnaire that addressed demographic factors, disease-related variables (symptom severity, current medication, and comorbid conditions), and cost-related variables (recall of medical service usage, expenditure on CAMs, WTP questionnaires, and work loss due to asthma over the previous 12 months). Patients were asked to keep a diary and record absences from school or work, medical services usage, and expenditures related to asthma management for 3 months (from 1 April to 30 June 2004). This prospective evaluation was designed to determine the extent to which recall bias affected questionnaire responses. All patients enrolled in this study provided written informed consent.
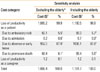
Asthma-related costs were estimated as prevalence-based costs (the cross-sectional costs of all patients per annum) in 2004. All costs are presented in U.S. dollars calculated using the exchange rate for 30 April 2005: 1 U.S. dollar = 1,000 Korean won (₩). Costs before 2004 were extrapolated to 2004 values using the inflation rate of the field-specific price. The cost and source categories for the estimates are presented schematically in Table 1.
Direct formal medical costs were defined as the amounts expended on asthma management within the official health care system and included reimbursed and non-reimbursed costs. Reimbursed costs were payments for ambulatory care visits, hospital outpatient services, hospital inpatient stays, emergency room visits, physician and facility services, and prescribed medicines. These were extracted from NHIC data for the period 1 January to 31 December 2003 and included payments claimed by oriental medicine hospitals, which are regarded as part of the official health care system. Sometimes, because of stringent benefit coverage, patients paid a substantial sum for uninsured (out-of-coverage) services.15 For example, patients must pay in full for uninsured services such as meals during hospitalization and private rooms (rooms with fewer than six beds). In the present study, these were collectively categorized as non-reimbursed costs. The ratio of reimbursed to non-reimbursed costs derived from the patient survey was multiplied by the total amount of reimbursed costs calculated from NHIC data.
Direct informal medical costs were defined as expenditures on CAMs not recompensed by the official health care system. Direct non-medical costs were defined as expenditures on medical-related services such as transport to the hospital and private nursing personnel. These costs were obtained by patient survey. A geometric mean value was calculated from the mean values of three age groups: elderly, ≥65 years old; adults, 20-64 years old; and children, ≤19 years old. These values were extended to the national level by multiplying by the total number of patients with asthma.
Indirect costs were defined as costs incurred due to asthmarelated loss of work and premature death. To estimate the costs of asthma-related loss of work, the average number of absences per patient or caregiver as a result of admission, ambulatory visits, and care was obtained from the patient survey, and this number was multiplied by age- and gender-specific wages and employment rates. The costs of asthma-related premature death were estimated using the calculated number of asthma-related deaths in 2004 and the expected future income based on demographic characteristics.
Enrolled patients responded to a QOL questionnaire, developed by the Korean Society of Allergology,18 using a five-point scale to assess current QOL parameters. The patients also answered WTP questionnaires, which were designed as a bidding game. Patients were each allocated six different random bids, and after responding to yes-or-no questions twice, the patients were asked to evaluate their final WTP to improve their QOL. We used only half of the WTP estimates, because the WTP method generally provides an overestimation.19 Individually measured costs were transformed to the national level by using asthma prevalence.
The overall prevalence of asthma in the Republic of Korea in 2004 was 4.19%, based on NHIC data. Prevalence rates by age group are shown in Table 2. A total of 660 asthma patients from 31 institutions (18 in urban areas, 13 in rural areas) were enrolled in the patient survey. These included 180 elderly asthmatics (≥65 years old), 350 adult asthmatics (20-64 years old), and 130 child asthmatics (≤19 years old). Among these, 314 (47.8%) were male. According to asthma severity, 470 patents (71.2%) were categorized with mild asthma; 130 (19.7%), with moderate asthma; and 60 (9.1%), with severe asthma.
The total direct asthma-related cost in the Republic of Korea in 2004 was approximately $961.9 million. The estimated direct formal medical cost of asthma was $333.4 million in 2004. The largest portion was attributable to medication (35.3%), followed by ambulatory visits and hospitalization (Table 3). Direct informal medical costs amounted to $622.8 million and accounted for 64.7% of total direct medical costs. The direct formal and informal medical costs per patient per annum were $162.20 and $302.80, respectively. Direct non-medical costs were estimated to be $5.7 million, and these were mainly incurred by transportation.
Total costs for asthma-related loss of productivity for patients and caregivers in 2004 were estimated to be $1.18 billion and $66.4 million, respectively (Table 4). Up to 90% of lost productivity was attributable to absence or early leave from work. Individual asthmatics were willing to pay about $151.90 monthly to improve QOL up to a "normal" level. Intangible costs were estimated to be $2.06 billion, almost the same as the sum of the direct and indirect costs.
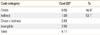
The total costs for asthma in 2004 are summarized by category in Table 5. The total cost of asthma, excluding intangible costs, in 2004 was $2.04 billion, 46.9% of which were direct costs and 53.1% of which were indirect costs. When intangible costs were included, total costs doubled to $4.11 billion, which is equivalent to 0.44% of the gross domestic product of the Republic of Korea in 200420 and 85.7% of all governmental social security expenditures in 2003.
A sensitivity analysis was conducted to evaluate the robustness of the cost estimates when key assumptions were modified. It was believed that productivity loss due to asthma in the elderly group (≥65 years old) was minimal. However, the prevalence of asthma in the elderly is exceptional (12.7% in 200121), and life expectancy is 75.4 years for men and 82.2 years for women.20 Thus, we performed a sensitivity test to evaluate the economic impact of productivity loss in the elderly. Contrary to our expectations, the loss of productivity due to asthma in the elderly had a considerable effect, accounting for $95.3 million (8.8%) of the indirect costs (Table 4). This amount was nearly twice the direct medical costs of hospitalization in the elderly.
The overall prevalence of asthma and the total costs related to asthma in 2004 were 4.19% and $2.04 billion, respectively, in the Republic of Korea. Direct and indirect costs contributed equally to total costs (46.9% and 53.1%, respectively). Furthermore, when intangible costs were included, the total cost increased to $4.11 billion, which is nearly equivalent to 0.44% of the gross domestic product in 2004.
The present study was performed using NHIC data, which has both advantages and disadvantages. Since 2000, the health insurance system in the Republic of Korea has provided coverage for the entire population.22 Under this system, all medical costs incurred for prescriptions, hospital admissions, and ambulatory visits are reimbursed by the NHIC. Thus, NHIC data provide nationwide, comprehensive estimates of disease-related costs, which cannot be acquired by secondary analysis of data or smallscale surveys. However, there are some concerns regarding NHIC data, particularly the possible misclassification of asthma listed as J45 or J46. For example, in children younger than 10 years of age, a wheezing episode caused by a non-asthmatic condition such as bronchiolitis is frequently diagnosed as asthma. Accordingly, this may limit the generalization of our results. Nevertheless, whether or not those listed by the NHIC as J45 or J46 were actually asthmatics, the estimated costs in this study represent the financial burden imposed on society by those diagnosed as having asthma. Thus, the estimations provide valuable information regarding health service planning.
Direct costs are usually determined by disease severity, medication compliance, overall prevalence of a disease, and health care costs. For example, in the US in 1994, direct costs represented the majority (88%) of the total costs, while indirect costs comprised only 12%, because health care costs are higher in the US.23 The health insurance system in the Republic of Korea relies on a fee scheduling system for reimbursement of health care providers, and the government scrupulously regulates this system, to the extent that reimbursements at best barely cover the cost of providing medical care.15 This regulated fee-for-service system is probably one reason for the difference in the proportion of direct costs between the US and the Republic of Korea.
Although many reports have mentioned the high prevalence of CAMs among asthmatics,11-13,24 little information is available regarding the costs at the national level. Surprisingly, the total expenditure on CAMs for asthmatics, presented as direct informal medical costs in the present study, was almost double the direct formal medical costs. Although there are undoubtedly national differences regarding individual methods and providers, CAMs for asthma should be recognized as a considerable cost burden on society and on individual patients.
One important challenge faced by those studying the financial burden of disease is how to precisely measure, value, and incorporate health-related QOL changes into an economic analysis. A cost-benefit analysis, also known as WTP, is one method of performing these evaluations. This type of analysis involves the use of survey techniques to elicit the amount of money an individual would be willing to pay for a specified health change.25,26 Zillich et al.27 demonstrated that WTP for an asthma cure is related to both objective and subjective disease severity. The mean monthly WTPs were $90, $131, and $331 for individual mild, moderate, and severe asthmatics, respectively.27 A similar trend was also found in the present study, but the differences by severity were smaller (the corresponding numbers were $137, $143, and $183). These findings suggest that some asthmatics in the Republic of Korea, although classified as mild by physicians, have an unsatisfied desire for a better QOL, matching the desire of severe asthmatics. Overall, the economic impact of impaired QOL, presented as intangible costs in this study, was tremendous and almost as large as the sum of direct and indirect costs.
The potential for cost savings based on reducing direct informal costs becomes readily apparent from our results. In this regard, the public health implications of CAMs should be viewed in the context of the limited evidence of their efficacy and their huge financial burden. In addition, considering that the economic impact of impaired QOL in asthmatics is as great as total asthma costs, improvements in QOL should be a goal of asthma control or a target of public programs for asthma care.
Figures and Tables
ACKNOWLEDGMENTS
This study was funded by the Korea Asthma Foundation. The authors thank the following physicians who participated in this study: Jung-Won Park, Kang-Mo Ahn, Jae-Young Lee, Sook-Hee Song, Soo-Keol Lee, Young-Joo Cho, Byoung-Whui Choi, Ho-Joo Yoon, Sang-Hoon Kim, Young-Koo Jee, Mee-Kyung Kim, Yong-Chul Lee, Choon-Sik Park, Joon-Woo Bahn, Sang-Rok Lee, Yoon-Seok Chang, In-Sun Choi, Woo-Kyung Kim, Soo-Jong Hong, Young-Ho Rha, Bok-Yang Pyun, Seung-Yeon Nam, Soo-Young Lee, Jae-Won Oh, Myung-Hyun Sohn, Bong-Choon Lee, and Jung-Keun Kim.
References
1. Mellis CM, Peat JK, Bauman AE, Woolcock AJ. The cost of asthma in New South Wales. Med J Aust. 1991. 155:522–528.
2. Krahn MD, Berka C, Langlois P, Detsky AS. Direct and indirect costs of asthma in Canada, 1990. CMAJ. 1996. 154:821–831.
3. Szucs TD, Anderhub H, Rutishauser M. The economic burden of asthma: direct and indirect costs in Switzerland. Eur Respir J. 1999. 13:281–286.
4. Chew FT, Goh DY, Lee BW. The economic cost of asthma in Singapore. Aust N Z J Med. 1999. 29:228–233.
5. Weiss KB, Sullivan SD, Lyttle CS. Trends in the cost of illness for asthma in the United States, 1985-1994. J Allergy Clin Immunol. 2000. 106:493–499.
6. Gupta R, Sheikh A, Strachan DP, Anderson HR. Burden of allergic disease in the UK: secondary analyses of national databases. Clin Exp Allergy. 2004. 34:520–526.
7. Poulos LM, Toelle BG, Marks GB. The burden of asthma in children: an Australian perspective. Paediatr Respir Rev. 2005. 6:20–27.
8. Barnes PJ, Jonsson B, Klim JB. The costs of asthma. Eur Respir J. 1996. 9:636–642.
9. Expert panel report 3: guidelines for the diagnosis and management of asthma [Internet]. National Heart, Lung, and Blood Institute. 2007. updated 2007 Aug 28; cited 2010 Feb 1. Bethesda (MD): U.S. Dept. of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute;Available from: http://www.nhlbi.nih.gov/guidelines/asthma/asthgdln.pdf.
10. British Thoracic Society Scottish Intercollegiate Guidelines Network. British Guideline on the Management of Asthma. Thorax. 2008. 63:Suppl 4. iv1–iv121.
11. Bielory L. Complementary and alternative interventions in asthma, allergy, and immunology. Ann Allergy Asthma Immunol. 2004. 93:S45–S54.
12. Schäfer T. Epidemiology of complementary alternative medicine for asthma and allergy in Europe and Germany. Ann Allergy Asthma Immunol. 2004. 93:S5–S10.
13. Ernst E. Complementary therapies for asthma: what patients use. J Asthma. 1998. 35:667–671.
14. Senna G, Passalacqua G, Crivellaro M, Bonadonna P, Gani F, Dorizzi R, Dama A, Canonica GW, Lombardi C. Unconventional medicine: a risk of undertreatment of allergic patients. Allergy. 1999. 54:1117–1119.
15. Kwon S. Payment system reform for health care providers in Korea. Health Policy Plan. 2003. 18:84–92.
16. International classification of diseases [Internet]. World Health Organization. cited 2010 Feb 1. Available from: http://www.who.int/classifications/icd/en/.
17. Global strategy for asthma management and prevention [Internet]. Global Initiative for Asthma. GINA Workshop Report. cited 2010 Feb 1. Available from: http://www.ginasthma.com.
18. Park JW, Cho YS, Lee SY, Nahm DH, Kim YK, Kim DK, Sohn JW, Park JK, Jee YK, Cho YJ, Yoon HJ, Kim MK, Park HS, Choi BW, Choi IS, Park CS, Min KU, Moon HB, Park SH, Lee YK, Kim NS, Hong CS. Multi-center study for the utilization of quality of life questionnaire for adult Korean asthmatics (QLQAKA). J Asthma Allergy Clin Immunol. 2000. 20:467–480.
19. Johannesson M, Jönsson B, Borgquist L. Willingness to pay for antihypertensive therapy--results of a Swedish pilot study. J Health Econ. 1991. 10:461–473.
20. The World Factbook 2010 - Korea, South [Internet]. Central Intelligence Agency. cited 2010 Sep 17. Available from: https://www.cia.gov/library/publications/the-world-factbook/geos/ks.html.
21. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Park HW, Jung JW, Bahn JW, Chang YS, Choi DC, Chang SI, Min KU, Kim YY, Cho SH. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002. 32:1706–1712.
22. Peabody JW, Lee SW, Bickel SR. Health for all in the Republic of Korea: one country's experience with implementing universal health care. Health Policy. 1995. 31:29–42.
23. Smith DH, Malone DC, Lawson KA, Okamoto LJ, Battista C, Saunders WB. A national estimate of the economic costs of asthma. Am J Respir Crit Care Med. 1997. 156:787–793.
24. Schäfer T, Riehle A, Wichmann HE, Ring J. Alternative medicine in allergies - prevalence, patterns of use, and costs. Allergy. 2002. 57:694–700.
25. Blumenschein K, Johannesson M. Relationship between quality of life instruments, health state utilities, and willingness to pay in patients with asthma. Ann Allergy Asthma Immunol. 1998. 80:189–194.
26. Lundberg L, Johannesson M, Silverdahl M, Hermansson C, Lindberg M. Quality of life, health-state utilities and willingness to pay in patients with psoriasis and atopic eczema. Br J Dermatol. 1999. 141:1067–1075.
27. Zillich AJ, Blumenschein K, Johannesson M, Freeman P. Assessment of the relationship between measures of disease severity, quality of life, and willingness to pay in asthma. Pharmacoeconomics. 2002. 20:257–265.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download