Abstract
Three diisocyanates can cause occupational asthma (OA): toluene diisocyanate (TDI), 4,4 diphenylmethane diisocyanate (MDI), and 1,6-hexamethylene diisocyanate (HDI). We analyzed potential biomarkers of isocyanate-induced OA, based on investigated immunologic, genetic, neurogenic, and protein markers, because there is no serological testing method. The prevalence of serum IgG to cytokeratin (CK)18 and CK19 in TDI-OA was significantly higher than in controls, although the prevalence of these antibodies was too low for them to be used as biomarkers. Another candidate biomarker was serum IgG to tissue transglutaminase (tTG), because the prevalence of serum specific IgG to tTG was significantly higher in patients with TDI-OA than in controls. The human leukocyte antigen (HLA) DRB1*1501-DQB1*0602-DPB1*0501 haplotype may be used as a genetic marker for TDI-OA in Koreans via enhanced specific IgE sensitization in exposed subjects. The genetic polymorphisms of catenin alpha 3, alpha-T catenin (CTNNA3) were significantly associated with TDI-OA. Additionally, examining the neurokinin 2 receptor (NK2R) 7853G>A and 11424 G>A polymorphisms, the NK2R 7853GG genotype had higher serum vascular endothelial growth factor (VEGF) levels than the GA or AA genotypes among Korean workers exposed to TDI. To identify new serologic markers using a proteomic approach, differentially expressed proteins between subjects with MDI-OA and asymptomatic exposed controls in a Korean population showed that the optimal serum cutoff levels were 69.8 ng/mL for ferritin and 2.5 µg/mL for transferrin. When these two parameters were combined, the sensitivity was 71.4% and the specificity was 85.7%. The serum cytokine matrix metalloproteinase-9 (MMP-9) level is a useful biomarker for identifying cases of TDI-OA among exposed workers. Despite these possible biomarkers, more effort should be focused on developing early diagnostic biomarkers using a comprehensive approach based on the pathogenic mechanisms of isocyanate-induced OA.
Three diisocyanates cause occupational asthma (OA): toluene diisocyanate (TDI), 4,4-diphenylmethane diisocyanate (MDI), and 1,6-hexamethylene diisocyanate (HDI).1-3 TDI is the most common cause of OA in developing countries, with a prevalence of 2.9-13% in exposed workers.4 The pathogenic mechanisms of isocyanate-induced asthma remain incompletely understood5 and no reliable method of serological testing has been established.
Because permanent impairment of lung function was noted in long-term follow-up studies of isocyanate-induced asthma, the development of biomarkers to identify susceptible subjects among exposed workers is essential. Previously, we reported on biomarkers of TDI-induced asthma, but no others have been reported. In this review, we summarize potential biomarkers for isocyanate-induced asthma, based on different mechanisms, including immunologic, genetic, neurogenic, and protein markers.
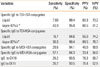
Serum specific IgE and IgG antibodies to TDI-human serum albumin (HSA) conjugate were found to have diagnostic value.6-8 A leading hypothesis concerning the pathogenesis of TDI-OA is that TDI acts as a hapten and undergoes nucleophilic addition reactions (conjugates) in vivo with airway proteins.9 Several groups have detected serum specific IgE antibodies to TDI-HSA conjugate in the sera of workers with a positive bronchial challenge to TDI; the prevalence varied between 0 and 50% of workers,10,11 depending on the conditions used to prepare the conjugate12 and the type of TDI-HSA conjugate used.13 Additionally, TDI-HSA conjugates may undergo changes in their three dimensional configuration, resulting in the generation of new antigenic epitopes. Thus, we used a vapor TDI-HSA conjugate as an antigen, and found the highest sensitivity in comparison with the conventional type (44% vs. 17%), as shown in Table 1.7,8,10,14 The time interval between the date of blood withdrawal for specific IgE testing and the date of last exposure to isocyanate can be an issue. Tee et al.11 reported that the sensitivity of serum specific IgE to isocyanate was the highest when blood was taken less than 30 days after the last exposure. However, serum specific IgG to isocyanate may persist for several years after the last exposure to TDI.15
Regarding MDI-induced asthma, a few studies have measured MDI-specific antibodies in small numbers of subjects.16,17 We measured the level of serum specific IgE and IgG in 58 MDI-exposed workers using an enzyme-linked immunosorbent assay (ELISA).18 The levels of these antibodies were significantly higher than those of the unexposed controls. The prevalence of specific IgG antibody to MDI-HSA conjugate was higher (20.7%) than that of specific IgE antibody (8.6%), indicating that serum specific IgG antibodies to MDI-HSA conjugate may be useful for diagnosing MDI-OA in exposed workers (Table 1). However, these antibodies had a relatively low prevalence and better biomarkers should be identified.
In conclusion, the detection of serum specific IgE or IgG is helpful for diagnosing isocyanate-induced asthma, although this alone is not sensitive enough to serve as a biomarker. However, it is certainly useful for confirming isocyanate-specific type I hypersensitivity, documenting exposure, and monitoring subclinical conditions. Efforts to generate new volatile isocyanate-albumin conjugates will increase the sensitivity and specificity of serum specific antibody tests, which will have potentially greater biological relevance as serologic biomarkers.
Exposure to TDI increases cytokeratin (CK)19 expression in human airway epithelial cells, initiating an immune response.19 The prevalence of serum IgG to CK18 and CK19 in TDI-OA was significantly higher than in other exposed and unexposed controls. The patients with high serum IgG to CK19 had a significantly lower PC20 methacholine, indicating that it may be involved in airway inflammation. However, the prevalence of these antibodies is not high enough for them to be used as biomarkers, because the prevalence was less than 25% in TDI-OA patients; the differences were significant compared with asymptomatic exposed controls (AECs; Table 1).5
Another candidate biomarker is serum IgG to tissue transglutaminase (tTG), because the prevalence of serum specific IgG to tTG was significantly higher in patients with TDI-OA, compared with AECs, those with allergic asthma, and unexposed normal controls. Moreover, the patients with TDI-OA with high serum IgG to tTG had significantly lower methacholine PC20 values. TDI exposure could increase tTG activity via reactive oxygen species (ROS) production, which was found to cross-link with CK19 on immunoblot analysis, leading to persistent airway inflammation in TDI-OA patients.20 However, the sensitivity of this antibody as a biomarker is far too low.
The reported genetic markers for isocyanate-induced asthma are summarized in Table 2. A study performed in a Korean population found that the frequency of HLA DRB1*1501-DQB1*0602-DPB1* haplotype was significantly higher in TDI-OA patients than in AECs or normal controls. DQB1*0402 was significantly associated with the presence of serum specific IgE to TDI-HSA conjugate. Thus, the HLA DRB1*1501-DQB1*0602-DPB1*0501 haplotype may be a genetic marker for the development of TDI-OA in Koreans via enhanced specific IgE sensitization in exposed subjects.21 A study in a European population suggested an association with HLA DQB1*0503 and an inverse relationship with HLA-DQB1*0501.22-24 Despite some inconsistencies with other studies, our study population is the largest and is based on homogenous patients with TDI-induced asthma. However, larger cohorts should be studied in other homogenous ethnic populations to confirm whether this biomarker is useful.
Another study examined susceptibility genetic markers associated with the TDI-OA phenotype. First, a genome-wide association study was performed in 84 patients with TDI OA compared with 263 unexposed healthy controls using the Affymetrix 500K SNP chip. The genetic polymorphisms of catenin alpha 3, alpha-T catenin (CTNNA3) were significantly associated with TDI-OA. Carriers with the minor haplotype, HT2 [GG], of two genetic polymorphisms (rs10762058 and rs7088181) had significantly lower PC20 methacholine levels and lower mRNA expression of CTNNA3 than non-carriers. A genetic polymorphism in the 3??downstream region of CTNNA3 (rs1786929) was significantly associated with the TDI-OA phenotype and the prevalence of serum specific IgG to CK19.25 The small sample size for genome-wide association is one limitation of this study. Nevertheless, as TDI-OA is quite rare in developed countries, this study should be replicated in other populations. Furthermore, the detailed functions of this gene remain to be determined. In conclusion, this study provides an important contribution for Asian populations by identifying CTNNA3 as a potential biomarker for predicting genetic susceptibility to TDI-induced asthma.
Additionally, a study of a Korean population examined two single nucleotide polymorphisms (SNPs) of the neurokinin 2 receptor: NK2R 7853G>A (Gly231Glu) and 11424 G>A (Arg375His). No significant difference in allele, genotype, or haplotype frequencies of these two SNPs was seen, but subjects with the NK2R 7853GG genotype had higher serum vascular endothelial growth factor (VEGF) levels than those with GA or AA among the TDI-exposed workers, suggesting that the NK2R 7853GG genotype contributes to increased serum VEGF levels, resulting in airway inflammation after TDI exposure, which may be mediated by neurogenic ROS.26 These results suggest that the NK2R 7853G>A polymorphism is a candidate biomarker for TDI OA. However, this study needs to be repeated using larger cohorts. Additionally, the indirect relationship between serum VEGF and NK2R 7853G>A needs to be investigated to determine whether there is a functional association between the two, which could assist in determining whether this may be used as a biomarker.
Several studies have focused on anti-oxidant gene markers. Wikman et al.27 showed an association of N-acetyltransferase genotypes as modifiers of the diisocyanate exposure-associated asthma risk. They showed that slow acetylator N-acetyltransferase 1 (NAT1) genotypes had a 2.5-fold greater risk of diisocyanate-induced asthma. This was the first result to suggest that glutathione S-transferases (GSTs) and NATs play an important role in the inception of asthmatic reactions related to occupational exposure to diisocyanates. A study in a Swedish population showed that the glutathione S-transferase pi (GSTP1) genotype should be considered when evaluating biomarkers of TDI exposure in urine and plasma. A protective effect of GSTP1 105 Val was seen in TDI-related asthma.28 As this study has not been replicated, no conclusion can yet be drawn regarding these biomarkers.
More recently, our unpublished data showed that the adrenergic beta-2, ADRB2 46A>G, 252G>A, and 523C>A SNPs and haplotype 1 [TTACGC] were significantly associated with specific IgE antibodies to the TDI-HSA conjugate in TDI-exposed subjects. Exposed workers with the AA genotype of the 46 A>G polymorphism had significantly higher serum specific IgE levels than those with the GG genotype, suggesting that ADRB2 polymorphisms may affect IgE-specific sensitization to TDI-HSA conjugate in TDI exposed workers. As TDI-OA is a complex process, ADRB2 polymorphisms with further environmental or genetic factors may increase TDI-OA susceptibility and should be evaluated further.
Bronchoalveolar lavage (BAL) fluid and plasma are sources of proteins. To identify new serologic markers using a proteomic approach, differentially expressed proteins between subjects with MDI-OA and AECs were studied in a Korean population. Two-dimensional electrophoresis was performed using BAL fluid obtained from subjects after an MDI-specific inhalation challenge and selected protein spots were then identified by matrix-assisted laser desorption/ionization time-of-flight mass spectrometry. In total, 23 protein spots distinguished the subjects with MDI-OA from AECs. Among them, ferritin expression was down-regulated, whereas transferrin expression was up-regulated in subjects with MDI-OA, compared with AECs. The clinical relevance of the differentially expressed spots was evaluated by ELISA using sera from the MDI-OA, AEC, and unexposed healthy control groups. Then, receiver operating characteristic (ROC) curves were plotted, and the sensitivity and specificity were determined. To identify subjects with MDI-OA, the optimal serum cutoff levels were 69.8 ng/mL for ferritin and 2.5 µg/mL for transferrin. When these two parameters were combined, the sensitivity was 71.4% and the specificity was 85.7% (Table 2). Serum ferritin and transferrin levels are associated with the MDI-OA phenotype.29 However, a recent study performed in Spain showed that the serum ferritin and transferrin levels did not differ among TDI-OA, TDI-exposed workers without OA, or healthy controls; therefore, these potential markers need to be studied further before they can be used.30 Another candidate protein as a serologic marker for detecting isocyanate-OA among isocyanate-exposed workers was the serum vitamin D binding protein (VDBP) level.31 To confirm this, additional functional studies are ongoing.
The inflammatory response involves lymphocytes, eosinophils, neutrophils, and bronchial epithelial cells, and related cytokines, such as myeloperoxidase (MPO) and interleukin-8 (IL-8), are involved in the pathogenesis of TDI-OA.32 In particular, increased production of matrix metalloproteinase-9 (MMP-9), tissue inhibitor of metalloproteinase-1 (TIMP-1),33,34 and VEGF35 are thought to play important roles in airway inflammation and airway remodeling.
Recent studies have revealed that MMP-9 acts on pro-inflammatory cytokines, chemokines, and other proteins to regulate varied aspects of inflammation.36,37 A longitudinal study of patients with diisocyanate-induced asthma showed that inhaled steroid medication increased the BAL levels of MMP-9 and MMP-9/TIMP-1, which were inversely correlated with Th-2 type inflammation, suggesting a protective role of MMP-9.38 To evaluate the clinical significance of these cytokines, we compared the serum cytokine levels in patients with TDI-OA and AECs at the time of diagnosis and AECs and found significant differences in the serum levels of MMP-9, IL-8, and VEGF.39 Of these, MMP-9 was the most prominent cytokine, with the highest sensitivity (79.7%) and specificity (80.8%) using specific cutoff values. When the cytokines were combined to improve the sensitivity and specificity, the combination of MMP-9, VEGF, and IL-8 was the best, with the area under curve (AUC) value increasing to 0.822 (95% CI, 0.752 0.894; P<0.001) and the sensitivity and specificity changing to 82.6% and 75.8%, respectively. Considering the cost-benefit ratio and its applicability in clinical practice, MMP-9 can be considered the best serologic marker for predicting TDI-OA among TDI-exposed workers.
We have identified several potential candidate biomarkers in isocyanate-induced asthma, including serum specific IgE/IgG antibodies to TDI-HSA conjugates, serum specific IgG to CK19 and TG, genetic biomarkers, such as HLA DRB1*1501-DQB1*0602-DPB1*0501 haplotype, and serum levels of VDBP and MMP-9 for TDI-OA. In MDI-OA, serum-specific IgG antibody, ferritin and transferritin levels may be used as serologic markers. Despite these possible biomarkers, more effort should be focused on developing early diagnostic biomarkers, based on a comprehensive approach and the pathogenic mechanisms of isocyanate-induced OA. Because the identification of asymptomatic sensitizers and occupational rhinitis are important and are risk factors for OA, a surveillance system using biomarkers should be initiated for screening susceptible workers.
Figures and Tables
ACKNOWLEDGMENTS
This study was supported by the Korea Science and Engineering Foundation (KOSEF) grant funded by the Korean government (MEST, 2009-0078646).
References
1. Peters JM, Wegman DH. Epidemiology of toluene diisocyanate (TDI)-induced respiratory disease. Environ Health Perspect. 1975. 11:97–100.
2. Park HS, Cho SH, Hong CS, Kim YY. Isocyanate-induced occupational asthma in far-east Asia: pathogenesis to prognosis. Clin Exp Allergy. 2002. 32:198–204.
3. Mapp CE. Agents, old and new, causing occupational asthma. Occup Environ Med. 2001. 58:354–360.
4. Park HS, Park JN, Kim JW, Kim SK. Clinical and immunological evaluation of isocyanate-exposed workers. J Korean Med Sci. 1992. 7:122–127.
5. Ye YM, Nahm DH, Kim CW, Kim HR, Hong CS, Park CS, Suh CH, Park HS. Cytokeratin autoantibodies: useful serologic markers for toluene diisocyanate-induced asthma. Yonsei Med J. 2006. 47:773–781.
6. Park HS, Kim HY, Nahm DH, Son JW, Kim YY. Specific IgG, but not specific IgE, antibodies to toluene diisocyanate-human serum albumin conjugate are associated with toluene diisocyanate bronchoprovocation test results. J Allergy Clin Immunol. 1999. 104:847–851.
7. Ye YM, Kim CW, Kim HR, Kim HM, Suh CH, Nahm DH, Park HS, Redlich CA, Wisnewski AV. Biophysical determinants of toluene diisocyanate antigenicity associated with exposure and asthma. J Allergy Clin Immunol. 2006. 118:885–891.
8. Park HS, Lee SK, Kim HY, Nahm DH, Kim SS. Specific immunoglobulin E and immunoglobulin G antibodies to toluene diisocyanate-human serum albumin conjugate: useful markers for predicting long-term prognosis in toluene diisocyanate-induced asthma. Clin Exp Allergy. 2002. 32:551–555.
9. Karol MH, Hauth BA. Use of hexyl isocyanate antigen to detect antibodies to hexamethylene diisocyanate (HDI) in sensitized guinea pigs and in a sensitized worker. Fundam Appl Toxicol. 1982. 2:108–113.
10. Baur X, Dewair M, Fruhmann G. Detection of immunologically sensitized isocyanate workers by RAST and intracutaneous skin tests. J Allergy Clin Immunol. 1984. 73:610–618.
11. Tee RD, Cullinan P, Welch J, Burge PS, Newman-Taylor AJ. Specific IgE to isocyanates: a useful diagnostic role in occupational asthma. J Allergy Clin Immunol. 1998. 101:709–715.
12. Son M, Lee M, Kim YT, Youn JK, Park H. Heterogeneity of IgE response to TDI-HSA conjugates by ELISA in toluene diisocyanate (TDI)-induced occupational asthma (OA) patients. J Korean Med Sci. 1998. 13:147–152.
13. Park HS, Kim HY, Lee SK, Kim SS, Nahm DH. Diverse profiles of specific IgE response to toluene diisocyanate (TDI)-human serum albumin conjugate in TDI-induced asthma patients. J Korean Med Sci. 2001. 16:57–61.
14. Bernstein DI, Cartier A, Cote J, Malo JL, Boulet LP, Wanner M, Milot J, L'Archeveque J, Trudeau C, Lummus Z. Diisocyanate antigen-stimulated monocyte chemoattractant protein-1 synthesis has greater test efficiency than specific antibodies for identification of diisocyanate asthma. Am J Respir Crit Care Med. 2002. 166:445–450.
15. Park HS, Lee SK, Lee YM, Kim SS, Nahm DH. Longitudinal study of specific antibodies to toluene diisocyanate (TDI)-human serum albumin (HSA) conjugate in patients with TDI-induced asthma. Korean J Intern Med. 2002. 17:249–251.
16. Lushniak BD, Reh CM, Bernstein DI, Gallagher JS. Indirect assessment of 4,4'-diphenylmethane diisocyanate (MDI) exposure by evaluation of specific humoral immune responses to MDI conjugated to human serum albumin. Am J Ind Med. 1998. 33:471–477.
17. Aul DJ, Bhaumik A, Kennedy AL, Brown WE, Lesage J, Malo JL. Specific IgG response to monomeric and polymeric diphenylmethane diisocyanate conjugates in subjects with respiratory reactions to isocyanates. J Allergy Clin Immunol. 1999. 103:749–755.
18. Hur GY, Koh DH, Choi GS, Park HJ, Choi SJ, Ye YM, Kim KS, Park HS. Clinical and immunologic findings of methylene diphenyl diisocyanate-induced occupational asthma in a car upholstery factory. Clin Exp Allergy. 2008. 38:586–593.
19. Choi JH, Nahm DH, Kim SH, Kim YS, Suh CH, Park HS, Ahn SW. Increased levels of IgG to cytokeratin 19 in sera of patients with toluene diisocyanate-induced asthma. Ann Allergy Asthma Immunol. 2004. 93:293–298.
20. Hur GY, Kim SH, Park SM, Ye YM, Kim CW, Jang AS, Park CS, Hong CS, Park HS. Tissue transglutaminase can be involved in airway inflammation of toluene diisocyanate-induced occupational asthma. J Clin Immunol. 2009. 29:786–794.
21. Choi JH, Lee KW, Kim CW, Park CS, Lee HY, Hur GY, Kim SH, Hong CS, Jang AS, Park HS. The HLA DRB1*1501-DQB1*0602-DPB1*0501 haplotype is a risk factor for toluene diisocyanate-induced occupational asthma. Int Arch Allergy Immunol. 2009. 150:156–163.
22. Bignon JS, Aron Y, Ju LY, Kopferschmitt MC, Garnier R, Mapp C, Fabbri LM, Pauli G, Lockhart A, Charron D. HLA class II alleles in isocyanate-induced asthma. Am J Respir Crit Care Med. 1994. 149:71–75.
23. Balboni A, Baricordi OR, Fabbri LM, Gandini E, Ciaccia A, Mapp CE. Association between toluene diisocyanate-induced asthma and DQB1 markers: a possible role for aspartic acid at position 57. Eur Respir J. 1996. 9:207–210.
24. Mapp CE, Beghe B, Balboni A, Zamorani G, Padoan M, Jovine L, Baricordi OR, Fabbri LM. Association between HLA genes and susceptibility to toluene diisocyanate-induced asthma. Clin Exp Allergy. 2000. 30:651–656.
25. Kim SH, Cho BY, Park CS, Shin ES, Cho EY, Yang EM, Kim CW, Hong CS, Lee JE, Park HS. Alpha-T-catenin (CTNNA3) gene was identified as a risk variant for toluene diisocyanate-induced asthma by genome-wide association analysis. Clin Exp Allergy. 2009. 39:203–212.
26. Ye YM, Kang YM, Kim SH, Kim CW, Kim HR, Hong CS, Park CS, Kim HM, Nahm DH, Park HS. Relationship between neurokinin 2 receptor gene polymorphisms and serum vascular endothelial growth factor levels in patients with toluene diisocyanate-induced asthma. Clin Exp Allergy. 2006. 36:1153–1160.
27. Wikman H, Piirila P, Rosenberg C, Luukkonen R, Kaaria K, Nordman H, Norppa H, Vainio H, Hirvonen A. N-Acetyltransferase genotypes as modifiers of diisocyanate exposure-associated asthma risk. Pharmacogenetics. 2002. 12:227–233.
28. Broberg KE, Warholm M, Tinnerberg H, Axmon A, Jonsson BA, Sennbro CJ, Littorin M, Rannug A. The GSTP1 Ile105 Val polymorphism modifies the metabolism of toluene di-isocyanate. Pharmacogenet Genomics. 2010. 20:104–111.
29. Hur GY, Choi GS, Sheen SS, Lee HY, Park HJ, Choi SJ, Ye YM, Park HS. Serum ferritin and transferrin levels as serologic markers of methylene diphenyl diisocyanate-induced occupational asthma. J Allergy Clin Immunol. 2008. 122:774–780.
30. Sastre J, Sastre B, Fernandez-Nieto M, Perez-Camo I, Sanchez JJ, del Pozo V. Serum ferritin and transferrin levels are not serologic markers of toluene diisocyanate-induced occupational asthma. J Allergy Clin Immunol. 2010. 125:762–764.
31. Choi G, Hur G, Kim J, Sung J, Palikhe N, Jeon I, Ye Y, Park H. Vit. D binding protein as a diagnostic marker for isocyanate-induced occupational asthma [abstract]. J Allergy Clin Immunol. 2009. 123:S267.
32. Jung KS, Park HS. Evidence for neutrophil activation in occupational asthma. Respirology. 1999. 4:303–306.
33. Park HS, Kim HA, Jung JW, Kim YK, Lee SK, Kim SS, Nahm DH. Metalloproteinase-9 is increased after toluene diisocyanate exposure in the induced sputum from patients with toluene diisocyanate-induced asthma. Clin Exp Allergy. 2003. 33:113–118.
34. Lee YC, Song CH, Lee HB, Oh JL, Rhee YK, Park HS, Koh GY. A murine model of toluene diisocyanate-induced asthma can be treated with matrix metalloproteinase inhibitor. J Allergy Clin Immunol. 2001. 108:1021–1026.
35. Choi JH, Suh YJ, Lee SK, Suh CH, Nahm DH, Park HS. Acute and chronic changes of vascular endothelial growth factor (VEGF) in induced sputum of toluene diisocyanate (TDI)-induced asthma patients. J Korean Med Sci. 2004. 19:359–363.
36. Parks WC, Wilson CL, Lopez-Boado YS. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol. 2004. 4:617–629.
37. Kelly EA, Jarjour NN. Role of matrix metalloproteinases in asthma. Curr Opin Pulm Med. 2003. 9:28–33.
38. Piirila PL, Nordman H, Keskinen HM, Luukkonen R, Salo SP, Tuomi TO, Tuppurainen M. Long-term follow-up of hexamethylene diisocyanate-, diphenylmethane diisocyanate-, and toluene diisocyanate-induced asthma. Am J Respir Crit Care Med. 2000. 162:516–522.
39. Kim J, Kim J, Choi G, Jin H, Lee J, Sung J, Ye Y, Nahm D, Park H. Serum cytokine levels as serologic markers of toluene diisocyanate-induced occupational asthma [abstract]. J Allergy Clin Immunol. 2010. 125:AB82.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download