Abstract
Purpose
Lactobacilli are probiotic bacteria that are effective in the management of allergic diseases or gastroenteritis. It is hypothesized that such probiotics have immunoregulatory properties and promote mucosal tolerance. Our goal was to investigate whether Lactobacillus casei rhamnosus Lcr35 could inhibit airway inflammation in an ovalbumin (OVA)-induced murine model of asthma.
Methods
BALB/c mice aged 6 weeks were used in the present study. Lactobacillus casei rhamnosus Lcr35 was administered daily, starting 1 week prior to the first OVA sensitization (group 1) and 2 days before the first 1% OVA airway challenge (group 2). Mice that received only saline at both sensitization and airway challenge time points were used as negative controls (group 3), and those that had OVA-induced asthma were used as positive controls (group 4). Airway responsiveness to methacholine was assessed, and bronchoalveolar lavage (BAL) was performed. At the endpoint of the study, total IgE as well as OVA-specific IgE, IgG1 and IgG2a in serum was measured by enzyme-linked immunosorbent assay. Lung pathology was also evaluated.
Results
Airway hyperresponsiveness, total cell counts and the proportion of eosinophils in BAL fluid were significantly decreased in group 1 compared with group 4 (P<0.05). Total serum IgE levels were also significantly decreased in group 1 compared with group 4. Serum levels of OVA-specific IgE, IgG1 and IgG2a were not significantly influenced by treatment with Lcr35. There was significantly less peribronchial and perivascular infiltration of inflammatory cells in group 1 compared with group 4; however, there were no significant differences in methacholine challenge, BAL, serology or histology between groups 2 and 4.
Bronchial asthma is characterized by airway hyperresponsiveness, eosinophilic airway inflammation and increased immunoglobulin E (IgE) levels. These effects are mediated mainly by type 2 helper (Th2) cells.1-3 In particular, eotaxin, RANTES, interleukin (IL)-4, IL-5 and IL-13, which are produced by Th2 cells, are all related to airway hyperresponsiveness and inflammatory changes in the airway through the activation of eosinophils and IgE production by B cells.4-6 Because the influx and differentiation of Th2 cells are important factors in the development and aggravation of asthma, increasing interest has been focused on investigations that target the activation of Th2 cells or the modulation of the Th1/Th2 balance to prevent and treat asthma.
Human immune reactions to external antigens are composed of innate and acquired responses. Innate immunity plays a particularly crucial role in primary defense against external pathogens and signaling for the induction of acquired immunity.7,8 Allergic diseases are caused by the abnormal modulation of acquired immunity, which is especially affected by the activation of Th2 cells.9 Recent studies, however, have demonstrated that factors related to innate immunity are involved in early allergic reactions10 and that either a Th2 immune response alone or a combination of Th1 and Th2 immune responses is involved in cases in which allergic diseases do not develop.11 In addition, in animal models of allergic diseases, allergen-specific Th1 cells fail to counterbalance Th2 cell-induced airway hyperresponsiveness.12 These results imply that other mechanisms may be involved in the pathogenesis of allergic diseases through the Th1/Th2 imbalance. Numerous investigators have focused on the activation of regulatory T cells or the induction of immunologic tolerance as factors in the development of allergies.13 Immunologic tolerance induced by oral administration of allergens is effective in the treatment of allergic diseases and has less risk of adverse reactions compared with other administration methods.14,15
Many studies based on the hygiene hypothesis have indicated that alterations in intestinal flora can prevent and treat allergies.14,15 Attention has been given to the use of intestinal flora as probiotics.16-18 Probiotics are usually defined as live microbial food ingredients beneficial to health. These ingredients comprise normal commensal bacteria that are part of the healthy human gut microflora. Bifidobacteria and lactobacilli are representative probiotics. Allergic diseases can be prevented with treatment of intestinal flora with probiotics,15,16 and probiotics can prevent and treat allergic diseases.17-19 In a murine model of asthma, administration of Lactobacillus reuteri and Lactobacillus rhamnosus GG decreased airway hyperresponsiveness, the number of inflammatory cells in bronchoalveolar lavage (BAL) fluid, and inflammation of lung tissue.20,21
This study was conducted to investigate the effects of L. rhamnosus, a probiotic, on the prevention of asthma using a murine model of asthma.
A murine model of asthma was established according to a modification of the methods proposed by Steinmetz et al.22 Briefly, female BALB/c mice aged 6 weeks were sensitized by intraperitoneal administration of a mixture of ovalbumin (OVA; 10 µg; grade V, Sigma Inc., St. Louis, MO, USA) and alum (2.25 mg; Imject®, Pierce, Rockford, IL, USA). One week after the first sensitization, the mixture was administered intraperitoneally a second time. Seven days later, the mice inhaled 1% OVA using an ultrasonic sprayer (Nescosonic UN-511, Alfresa, Osaka, Japan) every day for 3 days (Fig. 1). The mice were divided into four groups of seven mice each: those that received Lactobacillus casei rhamnosus Lcr35 from 1 week before the primary sensitization to the endpoint of the study (group 1), those that received Lactobacillus casei rhamnosus Lcr35 from 2 days before inhalation of 1% OVA to the endpoint of the study (group 2), those that received only saline (instead of OVA) at both sensitization and airway challenge (group 3, negative controls), and those in which asthma was induced (group 4, positive controls). Lactobacillus casei rhamnosus Lcr35 was administered orally at a CFU of 1×109 per day (Fig. 1).20
The mice inhaled normal saline and methacholine aerosol (5, 10, 25 and 50 mg/mL), and a pulmonary function test was performed using an animal airway resistance recorder (body volume change recorder, All Medicus, Seoul, Korea) 24 hours after inhalation of 1% OVA. Enhanced pause (Penh) was measured at 10-s intervals for 3 minutes after inhalation of saline and each concentration of methacholine.
After measurement of airway hyperresponsiveness, the trachea was immediately exposed after anesthesia by intraperitoneal administration of ketamine-xylazine. BAL was performed through a catheter inserted into the exposed trachea following instillation of normal saline (2 mL) at 37℃. The BAL fluid was centrifuged at 1,500 rpm for 2 minutes at 4℃. After discarding the supernatant, we washed the resultant pellet with PBS and resuspended it in 100 µL PBS. Total BAL cell counts were performed using a haemacytometer. A differential cell count was performed using Diff-Quik staining on the basis of morphologic criteria and using a light microscope to evaluate at least 200 cells per slide.
After blood was withdrawn from the orbital venous plexus, serum was separated from the blood clot by centrifugation at 2,500 rpm for 20 minutes at 4℃. Absorbance of OVA-specific IgE, IgG1 and IgG2a, as well as total IgE, was measured using enzyme-linked immunosorbent assay.
The mean Penh value at 50 mg/mL methacholine was 4.87±0.82 in group 1, 6.13±0.97 in group 2, 2.88±0.38 in group 3, and 7.70±1.21 in group 4. The mean Penh value decreased by 37% in group 1 compared with group 4 (P<0.05; Fig. 2).
The mean total number of cells (×105/mL) in the BAL fluid was 3.96±0.46 in group 1, 6.08±0.77 in group 2, 2.37±0.24 in group 3, and 6.21±0.65 in group 4. As with airway hyperresponsiveness, the total number of cells in the BAL fluid was significantly less in group 1 compared with group 4 (P<0.05; Fig. 3). The mean percentage of eosinophils in the BAL fluid was 6.19±1.88% in group 1 and 13.88±2.06% in group 4 (P<0.05; Fig. 4). There were no significant differences in the percentage of eosinophils between groups 2 and 4 (Fig. 4).
Mean total IgE levels (A450nm) were 1.77±0.13 in group 1 and 2.48±0.22 in group 4 (P<0.05; Fig. 5). The total IgE level was 2.12±0.19 in group 2, but the difference between groups 2 and 4 was not statistically significant. Mean OVA-specific IgE levels were 1.04±0.07 in group 1, 1.23±0.07 in group 2 and 1.28±0.12 in group 4; however, the differences were not statistically significant between groups 1 and 4 and groups 2 and 4 (Fig. 5). Serum total IgE levels were significantly lower only in the comparison of groups 1 and 4. In addition, OVA-specific IgE levels tended to decrease, but this trend was not statistically significant.
Mean serum levels of OVA-specific IgG1 (A450nm) were 1.42±0.11 in group 1, 1.36±0.12 in group 2, and 1.55±0.08 in group 4; however, the differences were not statistically significant (Fig. 5). The OVA-specific IgG1 level was 1.06±0.05 in group 3. Mean serum levels of OVA-specific IgG2a (A450nm) were 1.29±0.12 in group 1, 1.49±0.05 in group, 2, 0.79±0.3 in group 3 and 1.58±0.09 in group 4. The differences were not statistically significant between groups 1 and 4 and groups 2 and 4 (Fig. 5).
Upon hematoxylin-eosin staining, peribronchial and perivascular infiltration of eosinophils was significantly heavier in group 1 compared with group 4 (Fig. 6D). However, there was no significant difference in eosinophil infiltration between groups 2 and 4. Inflammatory changes such as eosinophil infiltration were not observed in group 3 (Fig. 6B).
The aim of this study was to use a murine model to investigate the effects of L. rhamnosus on the prevention of asthma. Airway hyperresponsiveness was decreased at 50 mg/mL methacholine (maximum concentration) in groups 1 and 2, but the difference was statistically significant only between groups 1 and 4. The total number of cells in BAL fluid was significantly less in group 1 compared with group 4, and the percentage of eosinophils was significantly lower in group 1 compared with group 4. Hematoxylin-eosin staining revealed that peribronchial and perivascular infiltration of inflammatory cells was significantly decreased by treatment with Lactobacillus casei rhamnosus Lcr35. These results are consistent with previous studies that demonstrated that probiotics decrease airway hyperresponsiveness, the number of inflammatory cells in BAL fluid, and inflammatory cell infiltration to lung tissue in murine models of asthma.20,21 Airway hyperresponsiveness, the total number of cells and the percentage of inflammatory cells in BAL fluid, and the degree of inflammatory cell infiltration were not significantly different between groups 2 and 4. This result indicates that Lactobacillus casei rhamnosus Lcr35 may have an overt effect on the prevention of asthma before rather than after OVA sensitization.
In this study, serum IgE levels were significantly lower in group 1 compared with group 4 and serum OVA-specific IgE levels tended to decrease without any statistical significance. However, the serum levels of IgE and OVA-specific IgE were not significantly different between groups 2 and 4. Given these results, we believe that systemic Th2 immune reactions are modified by treatment with Lactobacillus casei rhamnosus Lcr35 before OVA sensitization, whereas antigen-specific immune reactions are not. This is consistent with the result reported by Kalliomaki et al.17 that probiotics administration prevents atopic dermatitis but does not decrease sensitization rates in humans. Meanwhile, serum levels of OVA-specific IgG1 and IgG2a tended to decrease in group 1 without any statistical significance, suggesting that Lactobacillus casei rhamnosus Lcr35 may modify immune reactions by both Th1 and Th2 cells rather than by either alone. Further studies are needed to confirm our results. The mechanism by which probiotics such as Lactobacillus casei rhamnosus Lcr35 modulate allergic diseases may not be via restoration of the Th1/Th2 imbalance but instead by immunologic tolerance induced by the activation of regulatory T cells.23-26
Many studies have used various strains of probiotics in murine models of asthma. Similar to our results, Feleszko et al.20 demonstrated that both Bifidobacterium lactis Bb-12 and Lactobacillus rhamnosus GG decrease airway hyperresponsiveness, the total number of cells, and the percentage of inflammatory cells in BAL fluid. Also consistent with our results, Feleszko et al.20 showed that serum total IgE levels were decreased by the two bacteria. They also reported that the two bacteria significantly decrease serum levels of OVA-specific IgE/IgG1 and prevent asthma before and after OVA sensitization, which is not in accordance with our results. This discrepancy may be explained by differences in initial time points and total duration of probiotics administration. Previous studies used mice aged 1 day and 8 weeks of probiotics administration, whereas our study used mice aged 6 weeks and 3 weeks of probiotics administration. Another explanation for the discrepancy may be the difference in methods of inducing asthma. Forsythe et al.21 suggested that asthma can be prevented by L. reuteri but not by L. salivarius. This implies that specific probiotic species are effective in the prevention and treatment of allergic diseases such as asthma. In our study, we found that Lactobacillus casei rhamnosus Lcr35 prevented asthma. Plausible reasons for this difference may involve (1) the kinds of probiotics used in murine models of asthma, (2) whether the study used live or dead bacteria, (3) the initial time point and total duration of probiotics administration, (4) the concentration of probiotics used, and (5) the method for establishing a murine model of asthma.
In this study, the mice were sensitized twice with OVA. Various pathophysiologic parameters were modified in group 1 but not in group 2, which suggests that changes in intestinal flora during early stages or before OVA sensitization may alter innate immunity, subsequently influencing acquired immunity. Furthermore, alterations in systemic immune reactions may prevent asthma.27
Some clinical studies on probiotics in allergic diseases have recently been reported. Rosenfeldt et al.28 demonstrated that administration of L. rhamnosus and L. reuteri improves clinical symptoms in patients with atopic dermatitis. A large cohort study of Lactobacillus GG administration for 4 weeks revealed decreased SCORAD in pediatric patients with atopic dermatitis.29 Other reports, however, have reported little or no therapeutic effects of probiotics on allergic diseases.30-33 This discrepancy may be attributable to the difference in the initial time point of probiotics administration. Quite a few studies on the clinical effects of probiotics in asthma have reported that probiotics have no beneficial effect on asthma.34-37 Some investigations using murine models of asthma have reported beneficial effects of probiotics.20,21 The immunomodulatory mechanisms of probiotics deserve further investigation.
In conclusion, the results of this study suggest that oral treatment with Lactobacillus casei rhamnosus Lcr35 before sensitization can attenuate airway inflammation and hyperresponsiveness in a murine model of asthma. In addition, Lactobacillus casei rhamnosus Lcr35 may have the potential to prevent asthma.
Figures and Tables
Fig. 1
Experimental protocol for the induction of allergic asthma and treatment scheme. Four groups of female BALB/c mice were analyzed. Lactobacillus rhamnosus (Lcr35)-treated groups (group 1 and group 2) were sensitized to OVA with adjuvant via intraperitoneal injections, while the control groups (group 3 and group 4) were sensitized with equivalent amounts of saline and OVA, respectively. Group 1: Lactobacillus rhamnosus (Lcr35)-treated group starting 7-day before first OVA sensitization, Group 2: Lactobacillus rhamnosus (Lcr35)-treated group starting 2-day before first 1% OVA challenge, Group 3: saline-sensitized and -challenged group, Group 4: OVA-sensitized and -challenged group.

Fig. 2
The effects of oral administration of Lactobacillus rhamnosus (Lcr35) on airway hyperresponsiveness. Lactobacillus rhamnosus (Lcr35) administration starting 7-day before first OVA sensitization significantly inhibits OVA-induced airway hyperresponsiveness to MeCh challenge compared with that of positive control group. Data are expressed as the averages of seven mice per group. Values are expressed as mean±SEM. *P<0.05 and **P<0.01, as compared with positive control group (OVA/OVA).

Fig. 3
Total cell counts in BAL fluid. Oral administration of Lactobacillus rhamnosus (Lcr35) starting 7-day before first OVA sensitization significantly decreases total cell counts in BAL fluid compared with that of positive control group. *P<0.05 and **P<0.01, as compared with positive control group (OVA/OVA). Data are expressed as the averages of seven mice per group. Values are expressed as mean±SEM.
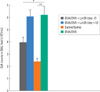
Fig. 4
Differential cell count in BAL fluid. 24 hr after the last OVA challenge mice were sacrificed and tracheas cannulated for BAL. Cells from BALF were counted, spun onto glass slides and stained with Diff-Quik before microscopy. *P<0.05 and **P<0.01. Data are expressed as the averages of seven mice per group. Values are expressed as mean±SEM.

Fig. 5
Levels of total IgE, OVA-specific IgE, OVA-specific IgG1 and OVA-specific IgG2a as determined by ELISA in sera of each group. *P<0.05 and **P<0.01. Data are expressed as the averages of seven mice per group. Values are expressed as mean±SEM.

Fig. 6
Effects of Lactobacillus rhamnosus (Lcr35) treatment on pulmonary inflammation. Representative lung sections from 2-group of Lactobacillus rhamnosus (Lcr35)-treated mice (A: Lcr35 (day -7), B: Lcr35 (day +12)), negative control mice (C: Saline/Saline) and positive control mice (D: OVA/OVA). The data shown are from one representative experiment. Similar results were obtained in three separate experiments using seven mice per group. H&E stain, original magnification: ×100.

ACKNOWLEDGMENTS
Funding source: This study was supported by "Young investigator award of Ahnkook Research Awards" on 2007.
References
1. Robinson DS, Hamid Q, Ying S, Tsicopoulos A, Barkans J, Bentley AM, Corrigan C, Durham SR, Kay AB. Predominant TH2-like bronchoalveolar T-lymphocyte population in atopic asthma. N Engl J Med. 1992. 326:298–304.
2. Walker C, Bode E, Boer L, Hansel TT, Blaser K, Virchow JC Jr. Allergic and nonallergic asthmatics have distinct patterns of T-cell activation and cytokine production in peripheral blood and bronchoalveolar lavage. Am Rev Respir Dis. 1992. 146:109–115.
3. Del Prete GF, De Carli M, D'Elios MM, Maestrelli P, Ricci M, Fabbri L, Romagnani S. Allergen exposure induces the activation of allergen-specific Th2 cells in the airway mucosa of patients with allergic respiratory disorders. Eur J Immunol. 1993. 23:1445–1449.
4. Lopez AF, Sanderson CJ, Gamble JR, Campbell HD, Young IG, Vadas MA. Recombinant human interleukin 5 is a selective activator of human eosinophil function. J Exp Med. 1988. 167:219–224.
5. Wang JM, Rambaldi A, Biondi A, Chen ZG, Sanderson CJ, Mantovani A. Recombinant human interleukin 5 is a selective eosinophil chemoattractant. Eur J Immunol. 1989. 19:701–705.
6. Finkelman FD, Katona IM, Urban JF Jr, Holmes J, Ohara J, Tung AS, Sample JV, Paul WE. IL-4 is required to generate and sustain in vivo IgE responses. J Immunol. 1988. 141:2335–2341.
7. Check W. Innate immunity depends on Toll-like receptors. ASM News. 2004. 70:317–322.
8. Boman HG. Antibacterial peptides: basic facts and emerging concepts. J Intern Med. 2003. 254:197–215.
9. Abreu MT, Arditi M. Innate immunity and toll-like receptors: clinical implications of basic science research. J Pediatr. 2004. 144:421–429.
10. Yazdanbakhsh M, Kremsner PG, van Ree R. Allergy, parasites, and the hygiene hypothesis. Science. 2002. 296:490–494.
11. Bach JF. The effect of infections on susceptibility to autoimmune and allergic diseases. N Engl J Med. 2002. 347:911–920.
12. Hansen G, Berry G, DeKruyff RH, Umetsu DT. Allergen-specific Th1 cells fail to counterbalance Th2 cell-induced airway hyperreactivity but cause severe airway inflammation. J Clin Invest. 1999. 103:175–183.
13. Akbari O, Stock P, DeKruyff RH, Umetsu DT. Role of regulatory T cells in allergy and asthma. Curr Opin Immunol. 2003. 15:627–633.
14. Wills-Karp M, Santeliz J, Karp CL. The germless theory of allergic disease: revisiting the hygiene hypothesis. Nat Rev Immunol. 2001. 1:69–75.
15. Kalliomaki M, Isolauri E. Role of intestinal flora in the development of allergy. Curr Opin Allergy Clin Immunol. 2003. 3:15–20.
16. Fuller R. Probiotics in man and animals. J Appl Bacteriol. 1989. 66:365–378.
17. Kalliomaki M, Salminen S, Arvilommi H, Kero P, Koskinen P, Isolauri E. Probiotics in primary prevention of atopic disease: a randomised placebo-controlled trial. Lancet. 2001. 357:1076–1079.
18. Kalliomaki M, Salminen S, Poussa T, Arvilommi H, Isolauri E. Probiotics and prevention of atopic disease: 4-year follow-up of a randomised placebo-controlled trial. Lancet. 2003. 361:1869–1871.
19. Isolauri E, Arvola T, Sutas Y, Moilanen E, Salminen S. Probiotics in the management of atopic eczema. Clin Exp Allergy. 2000. 30:1604–1610.
20. Feleszko W, Jaworska J, Rha RD, Steinhausen S, Avagyan A, Jaudszus A, Ahrens B, Groneberg DA, Wahn U, Hamelmann E. Probiotic-induced suppression of allergic sensitization and airway inflammationis associated with an increase of T regulatory-dependent mechanisms in a murine model of asthma. Clin Exp Allergy. 2007. 37:498–498.
21. Forsythe P, Inman MD, Bienenstock J. Oral treatment with live Lactobacillus reuteri inhibits the allergic airway response in mice. Am J Respir Crit Care Med. 2007. 175:561–569.
22. Neuhaus-Steinmetz U, Glaab T, Daser A, Braun A, Lommatzsch M, Herz U, Kips J, Alarie Y, Renz H. Sequential development of airway hyperresponsiveness and acute airway obstruction in a mouse model of allergic inflammation. Int Arch Allergy Immunol. 2000. 121:57–67.
23. Hart AL, Lammers K, Brigidi P, Vitali B, Rizzello F, Gionchetti P, Campieri M, Kamm MA, Knight SC, Stagg AJ. Modulation of human dendritic cell phenotype and function by probiotic bacteria. Gut. 2004. 53:1602–1609.
24. von der Weid T, Bulliard C, Schiffrin EJ. Induction by a lactic acid bacterium of a population of CD4(+) T cells with low proliferativecapacity that produce transforming growth factor beta and interleukin-10. Clin Diagn Lab Immunol. 2001. 8:695–701.
25. Pochard P, Gosset P, Grangette C, Andre C, Tonnel AB, Pestel J, Mercenier A. Lactic acid bacteria inhibit TH2 cytokine production by mononuclear cells from allergic patients. J Allergy Clin Immunol. 2002. 110:617–623.
26. Smits HH, Engering A, van der Kleij D, de Jong EC, Schipper K, van Capel TM, Zaat BA, Yazdanbakhsh M, Wierenga EA, van Kooyk Y, Kapsenberg ML. Selective probiotic bacteria induce IL-10-producing regulatory T cells in vitro by modulating dendritic cell function through dendritic cell-specific intercellular adhesion molecule 3-grabbing nonintegrin. J Allergy Clin Immunol. 2005. 115:1260–1267.
27. Gill HS, Rutherfurd KJ, Prasad J, Gopal PK. Enhancement of natural and acquired immunity by Lactobacillus rhamnosus (HN001), Lactobacillus acidophilus (HN017) and Bifidobacterium lactis (HN019). Br J Nutr. 2000. 83:167–176.
28. Rosenfeldt V, Benfeldt E, Nielsen SD, Michaelsen KF, Jeppesen DL, Valerius NH, Paerregaard A. Effect of probiotic Lactobacillus strains in children with atopic dermatitis. J Allergy Clin Immunol. 2003. 111:389–395.
29. Viljanen M, Savilahti E, Haahtela T, Juntunen-Backman K, Korpela R, Poussa T, Tuure T, Kuitunen M. Probiotics in the treatment ofatopic eczema/dermatitis syndrome in infants: a double-blind placebo-controlled trial. Allergy. 2005. 60:494–500.
30. Brouwer ML, Wolt-Plompen SA, Dubois AE, van der Heide S, Jansen DF, Hoijer MA, Kauffman HF, Duiverman EJ. No effects of probiotics on atopic dermatitis in infancy: a randomized placebo-controlled trial. Clin Exp Allergy. 2006. 36:899–906.
31. Wheeler JG, Shema SJ, Bogle ML, Shirrell MA, Burks AW, Pittler A, Helm RM. Immune and clinical impact of Lactobacillus acidophilus on asthma. Ann Allergy Asthma Immunol. 1997. 79:229–233.
32. Helin T, Haahtela S, Haahtela T. No effect of oral treatment with an intestinal bacterial strain, Lactobacillus rhamnosus (ATCC 53103), on birch-pollen allergy: a placebo-controlled double-blind study. Allergy. 2002. 57:243–246.
33. Wang MF, Lin HC, Wang YY, Hsu CH. Treatment of perennial allergic rhinitis with lactic acid bacteria. Pediatr Allergy Immunol. 2004. 15:152–158.
34. Vliagoftis H, Kouranos VD, Betsi GI, Falagas ME. Probiotics for the treatment of allergic rhinitis and asthma: systematic review of randomized controlled trials. Ann Allergy Asthma Immunol. 2008. 101:570–579.
35. Kopp MV, Hennemuth I, Heinzmann A, Urbanek R. Randomized, double-blind, placebo-controlled trial of probiotics for primary prevention: no clinical effects of Lactobacillus GG supplementation. Pediatrics. 2008. 121:e850–e856.
36. Kalliomaki M, Salminen S, Poussa T, Isolauri E. Probiotics during the first 7 years of life: a cumulative risk reduction of eczema in a randomized, placebo-controlled trial. J Allergy Clin Immunol. 2007. 119:1019–1021.
37. Giovannini M, Agostoni C, Riva E, Salvini F, Ruscitto A, Zuccotti GV, Radaelli G. A randomized prospective double blind controlled trial on effects of long-term consumption of fermented milk containing Lactobacillus casei in pre-school children with allergic asthma and/or rhinitis. Pediatr Res. 2007. 62:215–220.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download