Abstract
Rice is the major staple food in a large part of the world, especially in Asia. Hypersensitivity reactions to rice are rare. Moreover, cases of occupational allergies induced by inhalation of rice powder are uncommon. We report a 31-year-old male with work-related rhinitis and conjunctivitis symptoms caused by occupational exposure to rice powder in the grain industry. He showed positive responses to rice extracts on a skin prick test, and a high level of serum specific IgE to rice was detected by ELISA. Occupational rhinitis was confirmed by a nasal provocation test with rice extracts. An IgE ELISA inhibition test showed cross-creativity between rice and various grass pollen extracts. These findings suggest that the inhalation of rice powder can induce IgE-mediated occupational rhino-conjunctivitis, which may be derived from cross-reactivity to major grass pollens.
Rice is one of the most common cereals produced and consumed worldwide. Nevertheless, hypersensitivity reactions to rice are rare. Most of the several reported cases presented as asthma.1,2 Occupational rhinitis (OR) is more prevalent and is considered a major predisposing factor for occupational asthma (OA), although the OR burden remains unknown.3,4 This is the first case of OR induced by rice powder, as confirmed by nasal provocation and immunological tests, in a subject working in the grain industry.
A 31-year-old male was referred to our allergy clinic for a 3-year history of rhinorrhea, sneezing, nasal obstruction, and itchy eyes. He had worked in the grain industry for 4 years, during which he had been exposed to rice powder. Before working at the grain company, he had no symptoms. At the workplace, his symptoms became worse, but they were relieved during holidays. Neither contact nor ingestion of rice caused any allergic reactions. He was atopic and had no history of medical illness. A skin prick test was performed using a battery of common inhalant and food allergens (Bencard Co., Bredford, UK). He showed positive responses to grass pollens, including rye, orchard, and timothy grass, and a strong positive response to the crude rice extracts derived from his workplace (Fig. 1). The serum total IgE level increased to 145 KU/L (0-114 KU/L), and the specific IgE levels to rice, rye, and orchard grass were 2.05, 2.05, and 1.63 KU/L, respectively (0-0.35 KU/L), as measured by the ImmunoCAP system (Phardia, Uppsala, Sweden).
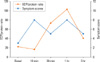
Rice extract was prepared according to a method described previously5 and was used to detect serum specific IgE by enzyme-linked immunosorbent assay (ELISA). The positive cutoff value for a high level of serum specific IgE was defined as the mean absorbance value +3 SD for samples from unexposed, non-atopic healthy controls. The patient showed a high level of IgE specific to the crude rice extract (Fig. 2A). To confirm the binding specificity, an IgE ELISA inhibition test was performed with rice and other grass pollen extracts, including rye, timothy, and orchard grass pollens. Both rice and grass pollen extracts were inhibited up to 40% by serial additions of each extract (1 to 500 µg/mL) in a dose-dependent manner, suggesting cross-creativity between the two (Fig. 2B).
A nasal provocation test was performed to confirm the causal relationship between rhinitis and the work environment.6-8 After a control saline challenge, exposure to 1 mg/mL of rice extract provoked an increase in the nasal symptom score at 10 minutes that persisted for 3 hours; there were no changes in lung function. The eosinophil cationic protein (ECP) level in nasal lavage fluid increased at 30 minutes, and the increase persisted until 3 hours after nasal provocation, as measured by a fluoroimmunoassay using the Pharmacia CAP system (Pharmacia-Upjohn, Uppsala, Sweden) (Fig. 3).
The patient was diagnosed with OR to rice powder. We recommended a job relocation and allergen immunotherapy with grass pollens, as he wanted to continue working.
OR precedes the development of OA, but its incidence is largely underestimated compared with that of OA. Previous studies have shown that high-molecular-weight agents such as laboratory animal allergens, flour, plant allergens, and biological enzymes can cause OR, with a prevalence of 2 to 87%.4,9 Rhinoconjunctivitis symptoms have been confirmed as one of the most significant factors in the development of OA.10 Continued exposure of the patient in the present study to rice powder may lead to the development of asthma, as suggested by previous studies.
The monitoring of airborne rice pollen in agricultural fields has revealed a high intensity of the released allergen.11 A cross-sectional study in rice farmers reported the prevalence of upper and lower respiratory symptoms such as hay fever (25.7%), watery eyes (14.9%), chronic cough (7.1%), and physician-diagnosed asthma (7.1%),12 indicating that occupational exposure to rice may trigger a respiratory allergy in workers and people living in the vicinity. However, immunological evaluations were not performed to confirm the causal relationships. In the present study, the patient showed positive responses to a skin prick test and high serum specific IgE to rice extract, as well as work-related symptoms.
Several allergenic components in rice have been described, including Ory s 1 (35 kDa), a 14- to 16-kDa member of the α-amylase/trypsin inhibitor family, a 33-kDa allergen with glyoxalase I activity, and a 9-kDa lipid transfer protein (LTP).5,13 Ory s 1 protein shows cross-reactivity with rye and Bermuda grass pollens in patients with a pollen allergy and shares significant sequence identity with the major pollen allergen of rye grass (Lol p 1; 65.5% identity) and Bermuda grass (Cyn d 1; 62.9% identity). 14 Moreover, LTP is known as a pan-allergen with cross-reactivity to botanically unrelated plants.15 Cross-reactivity between peach and rice LTP has been confirmed in several rice allergies, including anaphylaxis after rice ingestion16 and rhinitis with asthma caused by rice inhalation.15 In the present study, dose-dependent inhibition was observed when rice extracts and grass pollens were added in an IgE ELISA inhibition test, suggesting cross-reactivity. Therefore, immunotherapy with grass pollen allergens may be effective in this patient.
A nasal provocation test with rice extracts showed increased ECP as well as increased symptom scores for 3 hours after provocation. These results are consistent with previous studies demonstrating that a single allergen challenge test can induce a late response characterized by local accumulation of eosinophils and release of various mediators.17 In particular, the ECP level increases 1 or 2 hours after the challenge, reflecting the influx and activation of eosinophils in the late allergic phase. In previous studies, an increased ECP level was paralleled by an increased level of the typical TH2 cytokine interleukin-5,18 and elevated ECP was maintained for 24 hours after provocation, with a significant correlation to nasal symptom intensity,19 similar to the results of the present study.
In conclusion, we confirmed that rice powder inhalation can induce OR, in which an IgE-mediated mechanism was suggested.
Figures and Tables
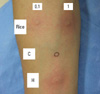 | Fig. 1Result of the skin prick test showing a positive response to rice extracts (C, normal saline; H, histamine). |
 | Fig. 2(A) Specific IgE ELISA to rice extracts in sera from the patient and 10 non-atopic healthy controls. Horizontal bars indicate the positive cutoff value determined from the mean ± 3 SD of the absorbance value of normal controls. (B) Result of the rice IgE-ELISA inhibition test with additions of rice and grass pollen extracts including rye, timothy, and orchard grasses and Dermatophagoides pteronyssinus. |
ACKNOWLEDGMENTS
This work was supported by a Korean Science and Engineering Foundation (KOSEF) grant (MEST, 2009-00786746) funded by the Korean government.
References
1. Orhan F, Sekerel BE. A case of isolated rice allergy. Allergy. 2003. 58:456–457.
2. Lezaun A, Igea JM, Quirce S, Cuevas M, Parra F, Alonso MD, Martin JA, Cano MS. Asthma and contact urticaria caused by rice in a housewife. Allergy. 1994. 49:92–95.
3. Moscato G, Siracusa A. Rhinitis guidelines and implications for occupational rhinitis. Curr Opin Allergy Clin Immunol. 2009. 9:110–115.
4. Malo JL, Lemiere C, Desjardins A, Cartier A. Prevalence and intensity of rhinoconjunctivitis in subjects with occupational asthma. Eur Respir J. 1997. 10:1513–1515.
5. Monzon S, Lombardero M, Perez-Camo I, Saenz D, Lasanta J. Allergic rhinoconjunctivitis after ingestion of boiled rice. J Investig Allergol Clin Immunol. 2008. 18:487–488.
6. Melillo G, Bonini S, Cocco G, Davies RJ, de Monchy JG, Frolund L, Pelikan Z. EAACI provocation tests with allergens. Report prepared by the European Academy of Allergology and Clinical Immunology Subcommittee on provocation tests with allergens. Allergy. 1997. 52:1–35.
7. Litvyakova LI, Baraniuk JN. Nasal provocation testing: a review. Ann Allergy Asthma Immunol. 2001. 86:355–364.
8. Choi GS, Park HJ, Hur GY, Choi SJ, Shin SY, Ye YM, Park HS. Vascular endothelial growth factor in allergen-induced nasal inflammation. Clin Exp Allergy. 2009. 39:655–661.
9. Moscato G, Vandenplas O, Van Wijk RG, Malo JL, Perfetti L, Quirce S, Walusiak J, Castano R, Pala G, Gautrin D, De Groot H, Folletti I, Yacoub MR, Siracusa A. EAACI position paper on occupational rhinitis. Respir Res. 2009. 10:16.
10. Gautrin D, Ghezzo H, Malo JL. Rhinoconjunctivitis, bronchial responsiveness, and atopy as determinants for incident non-workrelated asthma symptoms in apprentices exposed to high-molecular-weight allergens. Allergy. 2003. 58:608–615.
11. Sen MM, Adhikari A, Gupta-Bhattacharya S, Chanda S. Airborne rice pollen and pollen allergen in an agricultural field: aerobiological and immunochemical evidence. J Environ Monit. 2003. 5:959–962.
12. McCurdy SA, Ferguson TJ, Goldsmith DF, Parker JE, Schenker MB. Respiratory health of California rice farmers. Am J Respir Crit Care Med. 1996. 153:1553–1559.
13. Kumar R, Srivastava P, Kumari D, Fakhr H, Sridhara S, Arora N, Gaur SN, Singh BP. Rice (Oryza sativa) allergy in rhinitis and asthma patients: a clinico-immunological study. Immunobiology. 2007. 212:141–147.
14. Xu H, Theerakulpisut P, Goulding N, Suphioglu C, Singh MB, Bhalla PL. Cloning, expression and immunological characterization of Ory s 1, the major allergen of rice pollen. Gene. 1995. 164:255–259.
15. Enrique E, Ahrazem O, Bartra J, Latorre MD, Castello JV, de Mateo JA, Montoya E, Malek T, Barber D, Salcedo G. Lipid transfer protein is involved in rhinoconjunctivitis and asthma produced by rice inhalation. J Allergy Clin Immunol. 2005. 116:926–928.
16. Asero R, Amato S, Alfieri B, Folloni S, Mistrello G. Rice: another potential cause of food allergy in patients sensitized to lipid transfer protein. Int Arch Allergy Immunol. 2007. 143:69–74.
17. Miadonna A, Milazzo N, Gibelli S, Salmaso C, Lorini M, Tedeschi A. Nasal response to a single antigen challenge in patients with allergic rhinitis - inflammatory cell recruitment persists up to 48 hours. Clin Exp Allergy. 1999. 29:941–949.
18. Kramer MF, Jordan TR, Klemens C, Hilgert E, Hempel JM, Pfrogner E, Rasp G. Factors contributing to nasal allergic late phase eosinophilia. Am J Otolaryngol. 2006. 27:190–199.
19. Rondon C, Fernandez J, Lopez S, Campo P, Dona I, Torres MJ, Mayorga C, Blanca M. Nasal inflammatory mediators and specific IgE production after nasal challenge with grass pollen in local allergic rhinitis. J Allergy Clin Immunol. 2009. 124:1005.e1–1011.e1.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download