Abstract
Purpose
Aspirin-intolerant asthma (AIA) is characterized by moderate to severe asthma that is aggravated by aspirin or other non-steroidal anti-inflammatory drugs. Affected patients frequently have chronic rhinosinusitis and nasal polyposis due to persistent upper and lower airway inflammation with marked eosinophilia. IL-13 plays a crucial role in the development of allergic asthma by inducing airway eosinophilia and hyper-reactivity and it has been correlated with an increased eosinophil count.
Methods
Two promoter polymorphisms of the IL-13 gene (-1510 A>C and -1055C>T) and one coding nonsynonymus Arg110Gln (110G>A) polymorphism were genotyped using primer extension methods in 162 patients with AIA, 301 patients with aspirin-tolerant asthma (ATA), and 430 normal healthy controls (NC).
Results
There was no significant difference in the genotype, allele, and haplotype frequencies of the three polymorphisms among the three groups. AIA patients with the AA genotype -1510A>C (P=0.012) and CC genotype -1055C>T (P<0.001) had a significantly higher frequency of rhinosinusitis, as compared to those with the minor alleles of these two single nucleotide polymorphisms. AIA patients with the GG genotype had a higher peripheral eosinophil count (P=0.025) and a higher serum eotaxin-1 level (P=0.044), as compared to patients with the AA genotype IL-13 Arg110Gln (110G>A).
Conclusions
These findings suggest that the IL-13 polymorphisms at -1510A>C and 1055C>T are associated with the development of rhinosinusitis in AIA patients. IL-13 Arg110Gln may be associated with an increased eosinophil count and eotaxin-1 level and could increase eosinophilic inflammation in the upper and lower airways of patients with AIA.
Aspirin-intolerant asthma (AIA) is characterized by moderate to severe asthma and aggravated by aspirin or non-steroidal anti-inflammatory drug (NSAID) ingestion. Affected patients frequently have chronic rhinosinusitis and nasal polyposis associated with persistent eosinophilic infiltration in the upper and lower airway mucosa.1 AIA patients also have a higher peripheral eosinophil count than patients with aspirin-tolerant asthma (ATA) and other types of asthma.2
The Th2 cytokine IL-13, which shares significant pathways and many biological activities with IL-4, plays an important role in the development of allergic airway inflammation. IL-13 is a critical cytokine in the pathogenesis of allergic asthma in a mouse model of asthma,3 and is involved in several physiological changes, such as airway eosinophilia and hyper-responsiveness.4 In humans, CD4+T cells, eosinophils, mast cells, basophils, and natural killer T cells produce IL-13, inducing IgG4 and IgE synthesis in cultured B cells.5 IL-13 mRNA and protein are increased in the sputum of asthmatics and have been correlated with an increased eosinophil count6 and airway hyper-responsiveness (AHR).7 In addition, the expression of vascular cell adhesion molecule-1 (VCAM-I) is upregulated in endothelial cells, which may contribute to eosinophil migration into airway tissues.8
The IL-13 gene is located in the chromosome 5q31-q33 region. Evidence suggests that this location is associated with AHR and the severity of asthma.9-11 Genetic analyses have implicated the human IL-13 gene in the development of atopy and asthma. In human populations, genetic polymorphisms of IL-13, its receptor components, or the essential signaling element STAT6, are all associated with increased risks for atopy and asthma. Arg110Gln (rs 20541) is a functional single nucleotide polymorphism (SNP) in the coding region involved in the amino acid change from arginine (Arg) to glutamine (Gln) at position 110; such changes have been studied comprehensively. The Arg110Gln polymorphism is associated with elevated eosinophil counts and with mild to moderate asthma during childhood. Several studies have shown an association between IL-13 and high serum total IgE levels, bronchial hyper-responsiveness, and asthma.10,12 IL-13 polymorphisms have population-specific effects. In ethnic German populations, the IL-13 Arg110Gln variant has a significant association with high IgE levels.13 In addition, this allele was associated with the asthma phenotype in British and Japanese populations.14 Moreover, IL-13 is necessary and sufficient for the induction of AHR eosinophilic airway inflammation; in the absence of IL-13, this does not progress to AHR. Therefore, treatment of human asthma with IL-13 antagonists may be very effective.15
Although IL-13 is associated with asthma and atopy, no studies have evaluated its association with AIA. To address whether genetic polymorphisms of the IL-13 gene are associated with susceptibility to AIA, we performed a case-control study in a Korean population.
Three study groups including 162 patients with AIA, 301 patients with ATA, and 430 normal healthy controls (NC) were recruited from Ajou University Hospital, Suwon, Korea. The diagnosis of AIA was based on a positive response to a lysine-acetyl salicylic acid (ASA) bronchoprovocative test, which was performed on all study subjects according to a described method.16 The change in the forced expiratory volume in 1 sec (FEV1) was followed for 7 hours after the final dose of the ASA challenge. The ASA-induced change (%) in FEV1 was calculated as the percent of the post-challenge FEV1 relative to the pre-challenge FEV1, and defined as a positive reaction if the FEV1 level declined more than 20% from the baseline value.
Methacholine bronchial challenge tests were performed as described previously.17 The NC subjects were chosen from the general population using a screening questionnaire to confirm that they had no history of respiratory symptoms or ASA hypersensitivity. All NC subjects had an FEV1 greater than 80% of predicted, a methacholine provocation concentration (PC20) greater than 25 mg/mL, and normal findings on simple chest radiograms. Atopy was defined as one or more positive reactions on a skin prick test using 12 common aeroallergens (Bencard, Brendford, UK), with histamine and saline controls. The serum was aspirated, separated, and stored in aliquots at -20℃ until analyzed. Serum total IgE was measured using the UniCAP system (Phadia, Valinge, Sweden), according to the manufacturer's instructions. The threshold cutoff value for a specific IgE level was 0.35 KU/L as measured by UniCAP.
The presence of rhinosinusitis and nasal polyps was evaluated using paranasal sinus x-rays and rhinoscopy. Serum eotaxin-1 levels were measured using a quantitative sandwich enzyme immunoassay kit (ELISA) (R&D Systems, Minneapolis, MN, USA). Peripheral blood total eosinophil counts were measured from the collected blood samples. Eosinophil counts were transformed to a log10 scale for the analysis.
Informed consent was obtained from all subjects, and the institutional review board of Ajou University Hospital (Suwon, Korea) approved the study.
Forty healthy Korean volunteers were examined for SNPs. Genomic DNA was prepared from peripheral blood samples using the Puregene DNA purification kit (Gentra, Minneapolis, MN, USA) according to the manufacturer's protocol.
The IL-13 gene was examined for SNPs using an ABI Prism 3100 DNA analyzer (Applied Biosystems, Foster City, CA, USA). Three polymorphisms of IL-13 (-1510 A>C [rs1881457], -1055C>T [rs1800925], and Arg110Gln (110G>A) [rs20541]) were genotyped using a primer extension method and the SNAPshot ddNTP primer extension kit (Applied Biosystems, Foster City, CA, USA). The sequences of the amplifying and extension primers for IL-13 are shown in Table 1.
Differences in the genotype frequency between the two groups were examined with the chi-square test. Three logistic regression models (co-dominant, dominant, and recessive) were used to account for age and gender covariates. Differences in the mean values of the phenotypic characteristics among the AIA patients, according to genotype, were compared by analysis with chi-square (categorical variable) and independent t-tests (continuous variable) using a homozygous co-dominant model. The haplotypes of the IL-13 gene were analyzed using Haploview v2.0 based on the expectation maximization (EM) algorithm. The level of statistical significance was set at P<0.05.
The characteristics of the study subjects are presented in Table 2. The frequency of atopy was significantly higher in the subjects with AIA, as compared to the NCs (P<0.001). The percent decrease in the FEV1 after lysine ASA inhalation was significantly lower in the AIA patients, as compared to the ATA patients (P<0.001). The AIA patients had a significantly higher frequency of rhinosinusitis, as compared to the ATA patients (P<0.001). The log PC20 methacholine level was significantly lower in the AIA, as compared to the ATA patients (P=0.001).
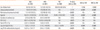
Genetic associations were examined among the three genetic polymorphisms of IL-13 (1510A>C, 1055C>T, and Arg110Gln (110G>A)) in the three study groups (AIA, ATA, and NC). The allele and genotype frequencies of the three polymorphisms did not differ significantly between the AIA and ATA patients (Table 3). In addition, there was no significant difference in the haplotype frequencies of the three polymorphisms among the study groups (data not shown).
Significant associations were noted between Arg110Gln (110G>A) and the total peripheral eosinophil counts. The AIA patients with the GG genotype had significantly higher peripheral eosinophil counts than those with the AA genotype (GG vs. AA, P=0.025, Fig. 1A). A significant association was detected between the IL-13 -1510A>C and IL-13 -1055C>T polymorphisms in AIA, but not in ATA, and the prevalence of rhinosinusitis tended to be higher with IL-13 Arg110Gln (110G>A). More specifically, AIA patients with the AA genotype of the 1510A>C polymorphism had a higher frequency of rhinosinusitis, as compared to patients with the CC genotype (P=0.012). In cases with 1055C>T, the AIA patients with the homozygous CC genotype had a higher frequency of rhinosinusitis and FEV1 than those with the TT genotype (P=0.001 and P=0.017, respectively; Table 4). Similarly, the homozygous GG genotype of Arg110Gln (110G>A) tended to be more frequent in rhinosinusitis than the homozygous minor AA genotype (P=0.058). No such association was found when compared with the phenotype of ATA (P>0.05) (Table 5). Furthermore, the GG genotype of AIA patients was associated with a significantly higher serum eotaxin-1 level, as compared to the AA genotype (P=0.044), but this was not seen in ATA (Fig. 1B and 1C). Other AIA-related phenotypes, such as the total serum IgE level and log PC20 methacholine, were not associated with the three polymorphisms of the IL-13 gene.
We evaluated the associations of three genetic polymorphisms of IL-13 with AIA, ATA, and NCs in a Korean population. This is the first study to investigate the genetic polymorphisms of two promoters of IL-13 at -1510A>C, -1055C>T and one coding region of Arg110Gln (110G>A) in AIA patients. No significant differences were found in the allele and genotype frequencies of these three SNPs, and their haplotypes, among the study groups. Our recent study also found no significant associations of the IL-13 gene polymorphism with the phenotypes of aspirin intolerant chronic urticaria.18 These findings suggest that these polymorphisms are not associated with the AIA phenotype in this Korean population.
Eosinophils are key mediators of the inflammation observed in patients with chronic rhinosinusitis. IL-13 is a unique mediator of eosinophilic inflammation, mucus hypersecretion, and AHR.19 IL-13 plays a major role in allergic inflammation by regulating the recruitment, homing, and activation of inflammatory cells. IL-13 has several functions relevant to the recruitment of T cells and eosinophils into the lung. These functions include the upregulation of VCAM1 expression, prolongation of eosinophil survival, eosinophil activation, and as a chemotactic agent. Eosinophils and mast cells release IL-13, which induces IgE synthesis in cultured B cells. The increased levels of IL-13 mRNA and protein in the sputum of subjects with asthma have been correlated with an increased eosinophil count6 and airway hyper-responsiveness.7 It is generally agreed that many allergic disorders are associated with hypereosinophilia, including asthma and atopic dermatitis. Recently, polymorphisms in IL-13 have been associated with the serum total IgE and eosinophil count and may be associated with asthma exacerbations.20 However, we did not find any significant result in terms of the IL-13 gene polymorphism and sputum eosinophil count in our study. Moreover, eosinophilic inflammation is one of the phenomena underlying AIA. Therefore, we also investigated the number of blood eosinophils in the patients with AIA associated with the IL-13 polymorphisms. The higher peripheral eosinophil counts in the homozygous GG genotype patients showed that this genotype was associated with moderate to severe eosinophilic inflammation in the patients with AIA in the Korean population. By contrast, the minor allele A of Arg110Gln (110G>A) was significantly associated with increased eosinophil counts in Costa Rica and among Caucasian children in the Childhood Asthma Management Program (CAMP).20 These findings suggest a regulatory role associated with the Arg-110Gln polymorphism that results from the substitution of Gln and is involved in eosinophilic infiltration in our study subjects. However, further study of a larger cohort is needed to confirm this. This SNP was also reported to be associated with methacholine AHR and asthma development in a childhood asthma cohort based on a Korean population.21 Specifically, IL-13 110AA was associated with increased total IgE levels and asthma development in children. Functional studies have demonstrated a regulatory role of substituted 110Gln in addition to the involvement of Stat-6 in monocytes, decreased IL-13 receptor alpha-2 affinity for IL-13, and increased expression of IL-13 in patients with asthma,22,23 as well as AHR induction in a murine model of asthma.24 By contrast, our findings suggest that the GG genotype is associated with a risk of eosinophilic infiltration and the development of AIA.
Chronic rhinosinusitis is central to the AIA phenotype. Previously, the TGFβ1-509C>T polymorphism was reported to have a significant association with the frequency of rhinosinusitis in AIA patients.25 Furthermore, our data on the gene-gene interaction between IL-10 and TGFb1 suggest its association with the development of AIA with rhinosinusitis.26 In this study, we found a significantly higher frequency of rhinosinusitis in AIA associated with the three IL-13 polymorphisms. IL-13 is an important marker for chronic eosinophilic rhinosinusitis.27 A recent study of the functional effects of the SNP -1055C>T suggests that although the minor allele is associated with enhanced promoter activity, in polarized human and murine CD4+ Th2 lymphocytes, this polymorphism may have the opposite effect on non-polarized CD4+ lymphocytes.28 Many examples of established associations, with different functional variants within the same gene or with opposite alleles at the same SNP in different populations, have been reported.29 Therefore, the higher frequency of rhinosinusitis in patients with AIA with the homozygous AA genotype of 1510A>C and the CC genotype of 1055C>T may be associated with the development of AIA. No statistically significant association was found in the case of IL-13 Arg110Gln and rhinosinusitis.
IL-13 is reported to induce eosinophil recruitment into the lung via an IL-5- and eotaxin-dependent mechanism.30 Indeed, several studies have reported that IL-13 induces eotaxin production in epithelial and smooth muscle cells.31,32 In-vivo data have shown that IL-13 stimulates eotaxin in IL-13 transgenic mice.33 The increase in eotaxin-1 levels was proportional to the impaired lung function and bronchial hyper-reactivity in asthmatics, as shown in previous studies.34,35 In this study, we found that the GG genotype of the Arg110Gln (110G>A) polymorphism was associated with a significantly higher eotaxin-1 level, as compared to the AA type; these findings suggest that the 110G allele is associated with eotaxin-1-mediated eosinophilic inflammation. Therefore, the IL-13 Arg110Gln polymorphism was found to be specifically associated with eotaxin-1 alterations during eosinophilic infiltration and is likely to be involved in the pathogenesis of AIA. However, there are a few limitations to our study, such as the sample size and lack of an in vitro functional study and the results need to be verified.
In conclusion, this study showed that the AA genotype of -1510A>C, and the CC genotype of -1055C>T are associated with a higher frequency of rhinosinusitis. Moreover, the GG genotype of Arg110Gln (110G>A) increased eotaxin-1 production, which might increase eosinophilic inflammation in the upper and lower airways of AIA patients.
Figures and Tables
 | Fig. 1
A: The peripheral log total eosinophilic count (TEC) according to IL-13 Arg110Gln (110G>A) polymorphism. B: The serum eotaxin-1 level according to IL-13 Arg110Gln (110G>A) gene polymorphism in AIA patients. C: The serum eotaxin-1 level according to IL-13 Arg110Gln (110G>A) gene polymorphism in ATA patients. |
Table 3
Allele and genotype frequencies of the IL-13 gene

*Each P value was calculated with co-dominant, dominant, and recessive models. Logistic regression analysis was applied to control for age and sex as covariables. q: minor allele frequency. AIA, aspirin-intolerant asthma; ATA, aspirin-tolerant asthma; NC, normal controls; n, number of patients.
Values in bold indicate significant P value.
ACKNOWLEDGMENTS
This study was supported by the Korea Health 21 R&D Project, Ministry for Health, Welfare and Family Affairs, Republic of Korea (A050571 and A030001).
References
1. Nasser SM, Pfister R, Christie PE, Sousa AR, Barker J, Schmitz-Schumann M, Lee TH. Inflammatory cell populations in bronchial biopsies from aspirin-sensitive asthmatic subjects. Am J Respir Crit Care Med. 1996. 153:90–96.
2. Sampson AP, Cowburn AS, Sladek K, Adamek L, Nizankowska E, Szczeklik A, Lam BK, Penrose JF, Austen KF, Holgate ST. Profound overexpression of leukotriene C4 synthase in bronchial biopsies from aspirin-intolerant asthmatic patients. Int Arch Allergy Immunol. 1997. 113:355–357.
3. Wills-Karp M, Luyimbazi J, Xu X, Schofield B, Neben TY, Karp CL, Donaldson DD. Interleukin-13: central mediator of allergic asthma. Science. 1998. 282:2258–2261.
4. van der Pouw Kraan TC, van Veen A, Boeije LC, van Tuyl SA, de Groot ER, Stapel SO, Bakker A, Verweij CL, Aarden LA, van der Zee JS. An IL-13 promoter polymorphism associated with increased risk of allergic asthma. Genes Immun. 1999. 1:61–65.
5. Punnonen J, Aversa G, Cocks BG, McKenzie AN, Menon S, Zurawski G, de Waal Malefyt R, de Vries JE. Interleukin 13 induces interleukin 4-independent IgG4 and IgE synthesis and CD23 expression by human B cells. Proc Natl Acad Sci U S A. 1993. 90:3730–3734.
6. Truyen E, Coteur L, Dilissen E, Overbergh L, Dupont LJ, Ceuppens JL, Bullens DM. Evaluation of airway inflammation by quantitative Th1/Th2 cytokine mRNA measurement in sputum of asthma patients. Thorax. 2006. 61:202–208.
7. Park SW, Jangm HK, An MH, Min JW, Jang AS, Lee JH, Park CS. Interleukin-13 and interleukin-5 in induced sputum of eosinophilic bronchitis: comparison with asthma. Chest. 2005. 128:1921–1927.
8. Rankin SM, Conroy DM, Williams TJ. Eotaxin and eosinophil recruitment: implications for human disease. Mol Med Today. 2000. 6:20–27.
9. Marsh DG, Neely JD, Breazeale DR, Ghosh B, Freidhoff LR, Ehrlich-Kautzky E, Schou C, Krishnaswamy G, Beaty TH. Linkage analysis of IL4 and other chromosome 5q31.1 markers and total serum immunoglobulin E concentrations. Science. 1994. 264:1152–1156.
10. Noguchi E, Shibasaki M, Arinami T, Takeda K, Maki T, Miyamoto T, Kawashima T, Kobayashi K, Hamaguchi H. Evidence for linkage between asthma/atopy in childhood and chromosome 5q31-q33 in a Japanese population. Am J Respir Crit Care Med. 1997. 156:1390–1393.
11. Palmer LJ, Daniels SE, Rye PJ, Gibson NA, Tay GK, Cookson WO, Goldblatt J, Burton PR, LeSöuef PN. Linkage of chromosome 5q and 11q gene markers to asthma-associated quantitative traits in Australian children. Am J Respir Crit Care Med. 1998. 158:1825–1830.
12. Postma DS, Bleecker ER, Amelung PJ, Holroyd KJ, Xu J, Panhuysen CI, Meyers DA, Levitt RC. Genetic susceptibility to asthma--bronchial hyperresponsiveness coinherited with a major gene for atopy. N Engl J Med. 1995. 333:894–900.
13. Graves PE, Kabesch M, Halonen M, Holberg CJ, Baldini M, Fritzsch C, Weiland SK, Erickson RP, von Mutius E, Martinez FD. A cluster of seven tightly linked polymorphisms in the IL-13 gene is associated with total serum IgE levels in three populations of white children. J Allergy Clin Immunol. 2000. 105:506–513.
14. Heinzmann A, Mao XQ, Akaiwa M, Kreomer RT, Gao PS, Ohshima K, Umeshita R, Abe Y, Braun S, Yamashita T, Roberts MH, Sugimoto R, Arima K, Arinobu Y, Yu B, Kruse S, Enomoto T, Dake Y, Kawai M, Shimazu S, Sasaki S, Adra CN, Kitaichi M, Inoue H, Yamauchi K, Tomichi N, Kurimoto F, Hamasaki N, Hopkin JM, Izuhara K, Shirakawa T, Deichmann KA. Genetic variants of IL-13 signalling and human asthma and atopy. Hum Mol Genet. 2000. 9:549–559.
15. Walter DM, McIntire JJ, Berry G, McKenzie AN, Donaldson DD, DeKruyff RH, Umetsu DT. Critical role for IL-13 in the development of allergen-induced airway hyperreactivity. J Immunol. 2001. 167:4668–4675.
16. Park HS. Early and late onset asthmatic responses following lysineaspirin inhalation in aspirin-sensitive asthmatic patients. Clin Exp Allergy. 1995. 25:38–40.
17. Kim SH, Bae JS, Holloway JW, Lee JT, Suh CH, Nahm DH, Park HS. A polymorphism of MS4A2 (-109T>C) encoding the beta-chain of the high-affinity immunoglobulin E receptor (FcepsilonR1beta) is associated with a susceptibility to aspirin-intolerant asthma. Clin Exp Allergy. 2006. 36:877–883.
18. Palikhe NS, Kim SH, Choi GS, Ye YM, Park HS. No evidence of association between interleukin-13 gene polymorphism in aspirin intolerant chronic urticaria. Allergy Asthma Immunol Res. 2009. 1:36–40.
19. Wynn TA. IL-13 effector functions. Annu Rev Immunol. 2003. 21:425–456.
20. Hunninghake GM, Soto-Quirós ME, Avila L, Su J, Murphy A, Demeo DL, Ly NP, Liang C, Sylvia JS, Klanderman BJ, Lange C, Raby BA, Silverman EK, Celedón JC. Polymorphisms in IL13, total IgE, eosinophilia, and asthma exacerbations in childhood. J Allergy Clin Immunol. 2007. 120:84–90.
21. Kim HB, Lee YC, Lee SY, Jung J, Jin HS, Kim JH, Kim BS, Kang MJ, Jang SO, Kim J, Kimm K, Shin ES, Lee SG, Hong SJ. Gene-gene interaction between IL-13 and IL-13R alpha 1 is associated with total IgE in Korean children with atopic asthma. J Hum Genet. 2006. 51:1055–1062.
22. Vladich FD, Brazille SM, Stern D, Peck ML, Ghittoni R, Vercelli D. IL-13 R130Q, a common variant associated with allergy and asthma, enhances effector mechanisms essential for human allergic inflammation. J Clin Invest. 2005. 115:747–754.
23. Arima K, Umeshita-Suyama R, Sakata Y, Akaiwa M, Mao XQ, Enomoto T, Dake Y, Shimazu S, Yamashita T, Sugawara N, Brodeur S, Geha R, Puri RK, Sayegh MH, Adra CN, Hamasaki N, Hopkin JM, Shirakawa T, Izuhara K. Upregulation of IL13 concentration in vivo by the IL-13 variant associated with bronchial asthma. J Allergy Clin Immunol. 2002. 109:980–987.
24. Chen W, Ericksen MB, Levin LS, Khurana Hershey GK. Functional effect of the R110Q IL13 genetic variant alone and in combination with IL4RA genetic variants. J Allergy Clin Immunol. 2004. 114:553–560.
25. Kim SH, Park HS, Holloway JW, Shin HD, Park CS. Association between a TGFbeta1 promoter polymorphism and rhinosinusitis in aspirin-intolerant asthmatic patients. Respir Med. 2007. 101:490–495.
26. Kim SH, Yang EM, Lee HN, Cho BY, Ye YM, Park HS. Combined effect of IL-10 and TGF-beta1 promoter polymorphisms as a risk factor for aspirin-intolerant asthma and rhinosinusitis. Allergy. 2009. 64:1221–1225.
27. Sauter A, Stern-Straeter J, Chang RC, Hörmann K, Naim R. Influence of interleukin-13 on beta-catenin levels in eosinophilic chronic rhinosinusitis cell culture. Int J Mol Med. 2008. 21:447–452.
28. Cameron L, Webster RB, Strempel JM, Kiesler P, Kabesch M, Ramachandran H, Yu L, Stern DA, Graves PE, Lohman IC, Wright AL, Halonen M, Klimecki WT, Vercelli D. Th2 cell-selective enhancement of human IL13 transcription by IL13-1112C>T, a polymorphism associated with allergic inflammation. J Immunol. 2006. 177:8633–8642.
29. Ober C, Hoffjan S. Asthma genetics 2006: the long and winding road to gene discovery. Genes Immun. 2006. 7:95–100.
30. Li L, Xia Y, Nguyen A, Lai YH, Feng L, Mosmann TR, Lo D. Effects of Th2 cytokines on chemokine expression in the lung: IL-13 potently induces eotaxin expression by airway epithelial cells. J Immunol. 1999. 162:2477–2487.
31. Hirst SJ, Hallsworth MP, Peng Q, Lee TH. Selective induction of eotaxin release by interleukin-13 or interleukin-4 in human airway smooth muscle cells is synergistic with interleukin-1beta and is mediated by the interleukin-4 receptor alpha-chain. Am J Respir Crit Care Med. 2002. 165:1161–1171.
32. Moore PE, Church TL, Chism DD, Panettieri RA Jr, Shore SA. IL-13 and IL-4 cause eotaxin release in human airway smooth muscle cells: a role for ERK. Am J Physiol Lung Cell Mol Physiol. 2002. 282:L847–L853.
33. Zhu Z, Homer RJ, Wang Z, Chen Q, Geba GP, Wang J, Zhang Y, Elias JA. Pulmonary expression of interleukin-13 causes inflammation, mucus hypersecretion, subepithelial fibrosis, physiologic abnormalities, and eotaxin production. J Clin Invest. 1999. 103:779–788.
34. Nakamura H, Weiss ST, Israel E, Luster AD, Drazen JM, Lilly CM. Eotaxin and impaired lung function in asthma. Am J Respir Crit Care Med. 1999. 160:1952–1956.
35. Lamkhioued B, Renzi PM, Abi-Younes S, Garcia-Zepada EA, Allakhverdi Z, Ghaffar O, Rothenberg MD, Luster AD, Hamid Q. Increased expression of eotaxin in bronchoalveolar lavage and airways of asthmatics contributes to the chemotaxis of eosinophils to the site of inflammation. J Immunol. 1997. 159:4593–4601.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download