Abstract
Purpose
Drug rash with eosinophilia and systemic symptoms (DRESS) and the Stevens-Johnson syndrome (SJS) are both severe drug reactions. Their pathogenesis and clinical features differ. This study compared the causes and clinical features of SJS and DRESS.
Methods
We enrolled 31 patients who were diagnosed with DRESS (number=11) and SJS (number=20). We retrospectively compared the clinical and laboratory data of patients with the two disorders.
Results
In both syndromes, the most common prodromal symptoms were itching, fever, and malaise. The liver was commonly involved in DRESS. The mucosal membrane of the oral cavity and eyes was often affected in SJS. The most common causative agents in both diseases were antibiotics (DRESS 4/11 (37%), SJS 8/20 (40%)), followed by anticonvulsants (DRESS 3/11 (27%), SJS 7/20 (35%)). In addition, dapsone, allopurinol, clopidogrel, sulfasalazine and non-steroidal anti-inflammatory drugs (NSAIDs) were sporadic causes.
The drug rash with eosinophilia and systemic symptoms (DRESS) syndrome, previously referred to as the 'drug hypersensitivity syndrome', is an adverse drug reaction characterized by skin rash, fever, lymph-node enlargement and internal organ involvement.1 The definition of DRESS is flawed in that it does not characterize the nature of the cutaneous rash. Aromatic anticonvulsants (phenytoin, phenobarbital, carbamazepine) and sulfonamides are the most common causes of DRESS.2
The differential diagnosis includes Stevens-Johnson syndrome (SJS), which is a rare, life-threatening, cutaneous adverse reaction. SJS is characterized by targetoid cutaneous lesions affecting less than 10% of the body surface area. There is mucous membrane involvement in approximately 90% of the affected patients.3 The risk factors for SJS include infection, vaccination, drugs, systemic diseases, physical agents and food. SJS has been associated with more than 100 drugs based on case reports and studies.4
DRESS and SJS are similar in that the clinical manifestations typically occur within 2 to 6 weeks after initiating drug therapy.1 However, the two syndromes have different characteristics, treatments and prognoses. Here, we compare the causes and clinical features of DRESS and SJS.
Records of the patients who were hospitalized with a diagnosis of DRESS or SJS from April 2004 to March 2008 were reviewed. The diagnosis of DRESS or SJS was based on the presence of a relationship between drug intake and the time to cutaneous adverse reactions. Moreover, the diagnosis of DRESS was based on the existence of associated systemic involvement and the presence of eosinophilia (>500/mm3 or >10%).5,6 The diagnosis of SJS was based on severe skin lesions (mucous membrane erosions, target lesions and epidermal necrosis with skin detachment) affecting less than 10% of the total body surface, regardless of the laboratory findings. The diagnosis was confirmed by a histopathological analysis of focal tissue (vacuolization of basal layer keratinocytes associated with lymphocytes).5,7,8
DRESS and SJS are differentiated by the nature of the skin lesions and extent of body surface area involvement over other criteria. Considering an appropriate differential diagnosis in patients with mucocutaneous erosions can help prevent misdiagnoses associated with cutaneous adverse drug reactions.
Statistical analysis was performed using SPSS version 17.0 for Windows (SPSS, Chicago, IL, USA). Data are expressed as the mean and standard error of the mean. Fisher's exact test and the Mann-Whitney U-test were used for categorical and continuous variables, respectively. Personal characteristics and disease-related factors were compared between the disorders. The association of laboratory tests with the two disorders was adjusted for the 95% confidence interval as the effect measure. A P value of less than 0.05 was considered statistically significant.
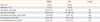
The study included 31 adults hospitalized with a diagnosis of DRESS or SJS. Eleven patients (4 men, 7 women; median age 51.5 years) had DRESS and 20 patients (12 men, 8 women; median age of 58.5 years) had SJS. There were no significant differences in the baseline values between the two disorders (Table 1).
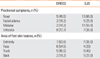
For DRESS syndrome, patients had prodromal symptoms of itching, fever and facial edema. Patients with SJS commonly had prodromal symptoms of fever and malaise. The first skin lesions appeared on the extremities and face in DRESS and on the trunk in SJS (Table 2). The trunk lesions in SJS were tender. The mucosal membranes of the oral cavity and eyes were commonly affected in SJS. The genitalia (2/19, 10.5%) and anus (2/19, 10.5%) were also affected (Table 3A).
The liver was involved in DRESS, and all patients with DRESS had elevated liver enzymes. The kidneys (2/11, 18.2%) were also involved (Table 3B).
In differentiating between DRESS and SJS, the skin lesions are considered first. Two patients with SJS had eosinophilia (>500/mm3 or >10%) and 17 had elevated liver enzymes (ALT or AST >40 U/L).
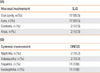
The most common causative drugs were antibiotics, which were identified as the cause in 4 of 11 patients (36%) with DRESS and 8 of 20 patients (40%) with SJS. From most to least common, the four antibiotics that were involved most frequently were vancomycin, ceftriaxone, rifampin, ciprofloxacin and Bactrim. Anticonvulsants were the second most common drugs involved; 3 (27%) cases of DRESS and 7 (35%) of SJS were associated with anticonvulsants. From most to least common, the four anticonvulsants that were involved most frequently were lithium, carbamazepine, lamotrigine and oxcarbazepine. The remaining drugs involved in both disorders were herbal medications (10%), allopurinol, clopidogrel and sulfonamide. In addition, dapsone (18%) and NSAIDs were associated with the development of DRESS (Table 4).
Patients with DRESS with internal organ involvement were treated with corticosteroids (7 patients, 64%) and dramatic improvement was observed. Most patients recovered in the absence of specific treatment after eliminating the causative drug. Most patients with SJS were successfully treated conservatively or with corticosteroids. Six patients (30%) were treated with antibiotics and one patient relapsed and died.
This study compared the causes and clinical features of DRESS and SJS. DRESS is a major cause of hospitalization for dermatological complications in patients treated with anticonvulsants.10 The clinical manifestations typically occur within 2 to 6 weeks after initiating drug therapy and most cases resolve without sequelae when the drug is discontinued. The outcome is fatal in 5-10% of cases. The most common clinical presentation of DRESS includes fever, eruption and lymphadenopathy. The most common hematological abnormalities are eosinophilia, leukocytosis and lymphocytosis. Liver involvement in patients with DRESS may range from a transitory increase in liver enzymes to liver necrosis with fulminant hepatic failure. Only transitory hepatitis was observed in our study, and the patients recovered without sequelae. Other potentially fatal complications are hypersensitivity myocarditis, pericarditis, pneumonitis and nephritis.6,11,12
Although there are a variety of etiologies, such as infections and underlying malignancies, drugs remain the predominant cause of SJS. The most commonly implicated drugs are anticonvulsants, sulfa derivatives, NSAIDs, penicillins, cephalosporins and allopurinols.1,9 The characteristic skin lesions seen in SJS are diffuse erythematous macules with purpuric, necrotic centers, and overlying blistering. These cutaneous lesions often demonstrate a positive Nikolsky sign, which is further detachment of the epidermis with slight lateral pressure. Painful erosions of the mucous membranes are common and may affect the lips, oral cavity, conjunctiva, nasal cavity, urethra, vagina, gastrointestinal tract and respiratory tract during the course of the illness. The mucosal membranes most often affected in our study were the oral cavity and eyes. SJS is fatal in 5-15% of cases.3,8 Both the incidence of the condition and the associated mortality appear to be increased in immunocompromised patients.
DRESS and SJS are part of a spectrum of adverse cutaneous drug reactions. However, the pathophysiology of DRESS and SJS has not been elucidated fully. Various theories have been proposed, including both immunological and non-immunological mechanisms.3,13 The current pathophysiological explanation for DRESS is immunological. Drugs with reactive metabolites can modify cellular proteins and target an autoimmune response against the skin or liver cells.11 It now appears that the immunological mechanisms associated with SJS are initiated by the Fas antigen, a cell surface molecule that can mediate apoptosis.3
Laboratory testing can help to identify internal organ involvement, which may not be evident clinically. A skin biopsy may help to confirm the diagnosis, but is usually not specific. The suspected drug should be discontinued immediately when these two syndromes are being considered.1,8,12 Delaying this measure may be associated with a poor outcome. For patients with extensive mucocutaneous involvement, prompt referral to a burn unit is recommended.
Corticosteroids remain the agents most widely used for treating DRESS, although the doses used vary widely across case reports.8 Favorable results have been reported with their use. In the absence of a well-established therapy, primary and secondary prevention have key roles in the management of these two syndromes.1,8 Milder cases of SJS can be managed in an inpatient setting using the same fundamental therapeutic protocol used for the treatment of burns. The use of medications to treat SJS remains controversial. Treatment with corticosteroids, while effective in most other acute inflammatory disorders, is controversial.
The most important diagnostic clues are the mucosal lesions and eosinophilia, characteristic of both syndromes. Age and gender were not helpful in differentiating SJS from DRESS. Elevated liver enzymes suggest the DRESS syndrome, well known to affect internal organs. As in a previous study, the liver was commonly involved in our DRESS patients. However, some earlier studies reported that up to 75% of the patients with SJS had elevated liver enzymes, similar to patients with DRESS.14 Hepatitis was observed in 85% of the patients with SJS in our study. Anticonvulsants were once the most common cause although, more recently, antibiotics have been reported to be the most common cause of both disorders.6,8,9 The increase in the use of antibiotics in Korea might explain this finding. After prompt withdrawal of the offending drug, conservative treatment or combination corticosteroid treatment has been used to treat patients with both syndromes, and most patients have improved clinical symptoms and laboratory findings with this approach. In the absence of specific treatment, the elimination of the causative drug and proper symptomatic treatment are the best management approaches for both SJS and DRESS.
Figures and Tables
References
1. Mahlab K, Orion E, Sthoeger ZM. Drug Rash with eosinophilia and systemic symptoms versus Stevens-Johnson Syndrome-a case that indicates a stumbling block in the current classification. Int Arch Allergy Immunol. 2006. 141:308–310.
2. Gruchalla RS. 10. Drug allergy. J Allergy Clin Immunol. 2003. 111:S548–S559.
3. Abe R. Toxic epidermal necrolysis and Stevens-Johnson syndrome: soluble Fas ligand involvement in the pathomechanisms of these diseases. J Dermatol Sci. 2008. 52:151–159.
4. Lee JH, Park HK, Heo J, Kim TO, Kim GH, Kang DH, Song GA, Cho M, Kim DS, Kim HW, Lee CH. Drug Rash with Eosinophilia and Systemic Symptoms (DRESS) syndrome induced by celecoxib and anti-tuberculosis drugs. J Korean Med Sci. 2008. 23:521–525.
5. Roujeau JC, Kelly JP, Naldi L, Rzany B, Stern RS, Anderson T, Auquier A, Bastuji-Garin S, Correia O, Locati F, Mockenhaupt M, Paoletti C, Shapiro S, Shear N, Schöpf E, Kaufman DW. Medication use and the risk of Stevens-Johnson syndrome or toxic epidermal necrolysis. N Engl J Med. 1995. 333:1600–1607.
6. Maoz KB, Brenner S. Drug rash with eosinophilia and systemic symptoms syndrome: sex and the causative agent. Skinmed. 2007. 6:271–273.
7. Roujeau JC, Stern RS. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994. 331:1272–1285.
8. Hazin R, Ibrahimi OA, Hazin MI, Kimyai-Asadi A. Stevens-Johnson syndrome: pathogenesis, diagnosis, and management. Ann Med. 2008. 40:129–138.
9. Lazarou J, Pomeranz BH, Corey PN. Incidence of adverse drug reactions in hospitalized patients: a meta-analysis of prospective studies. JAMA. 1998. 279:1200–1205.
10. Ganeva M, Gancheva T, Lazarova R, Troeva J, Baldaranov I, Vassilev I, Hristakieva E, Tzaneva V. Carbamazepine-induced drug reaction with eosinophilia and systemic symptoms (DRESS) syndrome: report of four cases and brief review. Int J Dermatol. 2008. 47:853–860.
11. Ichiche M, Kiesch N, De Bels D. DRESS syndrome associated with HHV-6 reactivation. Eur J Intern Med. 2003. 14:498–500.
12. Tas S, Simonart T. Management of drug rash with eosinophilia and systemic symptoms (DRESS syndrome): an update. Dermatology. 2003. 206:353–356.
13. Castaneda CP, Brandenburg NA, Bwire R, Burton GH, Zeldis JB. Erythema multiforme/Stevens-Johnson syndrome/toxic epidermal necrolysis in lenalidomide-treated patients. J Clin Oncol. 2009. 27:156–157.
14. Umebayashi Y, Enomoto H, Ogasawara M. Drug eruption due to peplomycin: an unusual form of Stevens-Johnson syndrome with pustules. J Dermatol. 2004. 31:802–805.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download