Abstract
Purpose
Skin allergies through type 1 and 4 hypersensitivity reactions are the most frequent manifestations of drug allergies. We had previously experienced a case of a nurse with cefotiam-induced contact urticaria syndrome. To aid in preventing the progression of drug-induced allergic disease in nurses, we conducted a survey of tertiary hospital nurses who were likely to have been exposed professionally to antibiotics.
Methods
All 539 staff nurses at a tertiary hospital were asked to respond to a questionnaire regarding antibiotic exposure. Of the 457 nurses (84.8%) who responded, 427 (79.2%) received a physical examination of the hands and 318 (59.0%) received skin prick tests with the β-lactam antibiotics cefotiam, cefoperazone, ceftizoxime, flomoxef, piperacillin and penicillin G.
Results
A positive response to at least one of the antibiotics occurred in 8 (2.6%) of the 311 subjects included in the analysis and stages 1 and 2 contact urticaria syndrome were observed in 38 (8.9%) and 3 (0.7%) of 427 nurses, respectively. The frequencies of a positive antibiotic skin test (6.9 versus 1.3%, χ2=7.15, P=0.018), stage 1 contact urticaria syndrome (14.4 versus 7.4%, χ2=4.33, P=0.038) and drug allergy (15.3 versus 3.6%, χ2=18.28, P=0.000) were higher in subjects with a positive skin allergy history than in those without. Allergic rhinitis (P=0.02, OR=3.86, CI=1.23-12.06), night cough (P=0.04, OR=3.12, CI=1.03-9.41) and food allergy (P=0.00, OR=9.90, CI=3.38-29.98) were significant risk factors for drug allergy.
Adverse drug reactions are common, occurring in 7% of the general population and 10-20% of hospitalized patients.1,2 Approximately 80% of adverse drug reactions are caused by the pharmacological properties of the causative drug (type A reactions) and thus are predictable. However, 10-15% are unpredictable and occur in vulnerable subjects (type B reactions). Additionally, there are type C reactions, which are associated with long-term therapy and type D reactions, which produce teratogenic and carcinogenic effects.3 Approximately 5-10% of type B adverse drug reactions (hypersensitivity reactions) are non-allergic and are induced by non-immunological mechanisms; other type B reactions are drug allergies that develop through immunological mechanisms induced by not only IgE- but also T cell-, or rarely immune complex-mediated reactions.
Skin tests for IgE-mediated immediate allergic reactions (type I hypersensitivity reactions) are frequently used to predict drug allergy or hypersensitivity. Intradermal tests with readings taken at 24 to 48 hours and patch tests can be used for delayed reactions occurring more than 1 hour after drug administration; these reactions are mediated mainly by T cells.2-4 A positive skin test for type I hypersensitivity is not always accompanied by drug allergy symptoms, as occur with other allergic diseases. Although cephalosporins at concentrations of 2-3 mg/mL are usually non-irritative, some cephalosporins produced false-positive reactions in skin prick tests because of irritative effects.2 Conversely, despite a negative penicillin skin prick test, penicillin allergy was evoked in 5.4% of patients with a positive history of penicillin allergy, suggesting a substantial number of false-negative reactions.2 Furthermore, although some antibiotics such as cephalosporin, ciprofloxacin, trimethoprim and penicillin are able to elicit a positive type I hypersensitivity skin reaction, most low-molecular-weight drugs act as haptens only after their conversion to reactive metabolites in the body; thus, skin testing with an unaltered drug may not identify a drug allergy.5 Despite these limitations of skin tests, we believe, based on our recent case of cefotiam-contact anaphylaxis,6 that skin tests for type I hypersensitivity to antibiotics should be performed in populations with the potential to develop drug allergies.
A search of the literature revealed that since the development of the second-generation cephalosporin cefotiam in 1981, there have been several cases of nurses with contact urticaria syndrome (CUS) due to cefotiam in Japan7,8 and Korea.9-14 Moreover, the disease was progressive, beginning as dermatitis localized at the contact area, progressing to generalized urticaria involving other organs and finally producing anaphylaxis. Our case showed not only a strong positive reaction to cefotiam on a skin test but also symptoms of CUS and a positive skin reaction to cefoperazone/sulbactam.6
As nurses are frequently exposed to antibiotics, drug sensitization and related allergy development should be monitored in this population. The early detection of drug allergies may prevent their progression. In this study, we asked all staff nurses at a tertiary hospital to respond to a questionnaire regarding antibiotic exposure and respondents received a physical examination of the hands and type I hypersensitivity skin tests with several common antibiotics.
For this study, a questionnaire regarding antibiotic exposure and signs of drug allergy was sent to all 539 nurses working at our university hospital in 2008. Of the 457 nurses (84.8%) who responded, 427 (79.2%) received a physical examination of the hands and 318 (59.0%) received skin tests. Subjects who did not provide consent were excluded from the study. Skin tests were not conducted in subjects who were or were thought to be pregnant or in those who had taken antihistamines within 1 week of the tests and could not discontinue antihistamine use for longer than 1 week. The study protocol was approved by our institutional review board (IRB No. I-2008-04-040).
After receiving the responses to the questionnaire and collecting demographic and occupational information, including the duration of antibiotic exposure, consenting respondents received a physical examination of the hands to detect any skin lesions and skin prick tests with common antibiotics. Available atopic allergy data were collected from hospital medical records. All data were collected by trained residents in the Departments of Internal Medicine and Dermatology or by trained nurses.
The questionnaire was constructed with reference to previous reports.15,16 It contained items regarding the history of exposure to antibiotics, including the duration of employment and experiences with injectable antibiotics and items for assessing the presence of allergic diatheses or diseases. Questions included the following: (1) Do you have common cold symptoms such as rhinorrhea and sneezing frequently or persistently? (2) Have you ever had dyspnea or wheezing? (3) Have you ever been awakened due to a severe night cough? (4) Have you ever had urticaria or dyspnea after eating? (5) Do you suffer from urticaria frequently? (6) Have you ever experienced a drug allergy? (7) How long have you had the aforementioned allergic symptoms? (8) Is there any family history of the aforementioned allergic symptoms or diseases? Maculopapular or morbilliform rashes, which are the most frequent manifestations of drug allergy,3 and contact dermatitis due to metal, as in a necklace, are usually regarded as type IV hypersensitivity reactions; however, these types of reactions were not queried separately in this study. Many subjects with these reactions reported urticaria as an alternative and some subjects recorded metal contact allergy or atopic dermatitis on the questionnaire form. Therefore, we classified urticaria, rash, contact dermatitis and atopic dermatitis as skin allergies. Subjects responding positively to any of the first six questions above were considered to have an allergic condition.
We employed the CUS staging system proposed by Von Krogh and Maibach17: stage 1, local urticaria on the contact area; stage 2, generalized urticaria; stage 3, extracutaneous involvement (rhinoconjunctivitis, asthma, orolaryngeal or gastrointestinal); and stage 4, anaphylactic shock. For stage 1, a clinical diagnosis of contact urticaria was made by asking, "Does itching or urticaria develop a few minutes after contact with antibiotics?" A clinical diagnosis of allergic contact dermatitis was made when a physical examination found eczema on one or both hands. Eczema is difficult to associate with antibiotics, because it usually develops 12-48 hours after antibiotic contact.18 For this reason, eczema, which was probably related to rubber gloves, was also regarded as antibiotic-related eczema. For stage 2, skin rashes were observed at sites distant from the contact site. For stage 3, a history of allergic rhinitis, conjunctivitis, bronchial asthma or oropharyngeal/gastrointestinal symptoms after hand contact with antibiotics was determined. For stage 4, a history of dizziness, loss of consciousness or decrease in blood pressure after hand contact with antibiotics was assessed. In addition, the symptom duration was recorded according to stage.
The Pharmaceutical Department of our hospital provided ceftizoxime, flomoxef, piperacillin, which are frequently prescribed antibiotics in our hospital, as well as cefotiam, cefoperazone and penicillin G, a representative antibiotic that often induces drug allergy. For the skin prick tests, penicillin G was used at 10,000 U/mL and cefoperazone, ceftizoxime, flomoxef and piperacillin were each used at a concentration of 33 mg/mL. Cefotiam was used at a lower concentration (10 mg/mL) to avoid severe adverse reactions, given that a nurse with cefotiam-contact anaphylaxis had previously shown a strong positive skin reaction and generalized allergic symptoms following a skin prick test using as little as 1 mg/mL cefotiam.6 In addition to the six drugs, two house dust mites, Dermatophagoides farinae and D. pteronyssinus, which are the most common atopic allergens; 0.9% normal saline; and 1 mg/mL histamine were used as controls for the skin prick tests. For the skin prick test, the forearm skin was pricked with a sterile needle through a drop of the antibiotic and 15 minutes later, the longest wheal diameter and the diameter perpendicular to it were measured using vernier calipers and then averaged. Test results in subjects with dermographism were not used in the analysis. A positive reaction was defined as a mean wheal size was ≥3 mm and larger than the size of the negative control, according to the European Society of Contact Dermatitis guidelines.19 For house dust mites, the ratio of the allergen wheal size relative to that of the histamine control (A/H ratio) was graded on a 4-point scale: 1+, 25-49%; 2+, 50-99%; 3+, 100-199%; and 4+, ≥200%. The house dust mite results were considered as clinically significant positive when the A/H ratio was ≥3+.20 When a medical chart was available, we collected data regarding the number of peripheral white blood cells, fraction of eosinophils, number of eosinophils (number of white blood cells×fraction of eosinophils) and serum total IgE measured by nephelometry (Behring Diagnostics, Marburg, Germany).
All statistical analyses were performed using SPSS 17.0 (SPSS Inc., Chicago, IL, USA). Data are expressed as the mean±SD. The prevalence of atopic allergy and the frequency of antibiotic sensitization were analyzed using descriptive statistics. Differences in the results according to the test response to antibiotics or the history of skin allergies were examined using Student's t-test, the χ2 test or Fisher's exact test. Risk factors for a positive skin test to an antibiotic, CUS and drug allergy were analyzed with a logistic regression model. A P value <0.05 was considered statistically significant.
Table 1 shows the differences in clinical characteristics between subjects who received skin prick tests (number=318) and those who did not (number=139). There was no significant difference in age or employment duration between the groups. However, there were significantly more antibiotic handlers in the group that took skin tests than in the group that did not (P<0.001). The duration of contact with intravenous antibiotics did not differ significantly between the antibiotic handlers in each group. Approximately 50% of the subjects in each group had allergic disease related to type I hypersensitivity and the prevalence of each disease was not significantly different between the groups. There was a trend toward a higher prevalence of drug allergy, especially antibiotic allergy, in the group that took the skin tests, but the difference was not statistically significant.
Stage 1 CUS was observed in 38 (8.9%) of the 427 subjects who underwent a physical examination, with localized urticaria observed in 11 subjects (2.6%) and eczema observed in 38 (8.9%). Sixteen (44.4%) of the 38 stage 1 subjects exhibited stage 1 CUS on both hands. Stage 2 CUS was present in three subjects (0.7%) and stages 3 and 4 were not observed. Stages 1 and 2 urticaria developed only in the group who took the skin tests, but the difference was not statistically significant (Table 1). The groups with and without skin tests did not differ with respect to the number of subjects with eosinophils ≥450/mm3 or with IgE ≥100 IU/mL (with: 1/17, 5.9%; without: 1/6, 16.7%).
Among the 318 subjects who took skin tests, 4 subjects who were negative for histamine sensitivity and 3 dermographic subjects who were positive for normal saline were excluded from the skin test analysis. Eight (2.6%) of the remaining 311 subjects showed a positive response to at least one of the six test antibiotics.
Among these eight, 3 were positive for cefotiam; 2, for cefoperazone; 4, for ceftizoxime; 5, for flomoxef; 4, for piperacillin; 5, for penicillin G; and 2, for all antibiotics (Table 2). Antibiotic-induced CUS was observed in three subjects, all whom showed both localized urticaria and eczema. Two of these subjects were sensitized to cefotiam and showed stage 2 CUS; one was sensitized to flomoxef and showed only stage 1 CUS. One subject who reported no use of antibiotics had a history of penicillin- and cephalosporin-induced urticaria and abdominal pain; she showed positive reactions to penicillin G and flomoxef. One subject who had a positive reaction to antibiotics did not have any allergic symptoms. Only two of the eight subjects with positive reactions to antibiotics had a positive history of drug allergy and the occurrence of CUS was not related to drug allergy history.
The eight subjects with positive responses to a skin prick test did not differ from those without a positive response (number=303) with respect to age, employment duration, positive history or duration of exposure to antibiotics (Table 3). However, a skin allergy history was significantly more prevalent in the group with a positive test than in the group without a positive test (62.5 versus 22.1%; χ2=7.15; P=0.018). Allergic diseases (87.5 versus 54.1%; χ2=3.51; P=0.078), drug allergies (25.0 versus 6.3%; χ2=4.34, P=0.095) and antibiotic allergies (14.3 versus 2.7%; χ2=3.12; P=0.194) tended to be more prevalent in the positive test group compared with the other group, although the differences were not statistically significant. Stage 1 CUS (37.5 versus 7.3%; χ2=9.64; P=0.020), localized urticaria (37.5 versus 2.6%; χ2=27.76; P=0.002]), eczema (37.5 versus 7.3%; χ2=9.64; P=0.020) and stage 2 CUS (25.0 versus 0.3%; χ2=49.65; P=0.002) occurred more frequently in the group with a positive test than in the group without a positive test. The time interval between stages 1 to 2 CUS was not obtained in the positive test group, but the interval was 14.3±14.0 months in the other group. There was no significant difference in the frequency of increased eosinophils in peripheral blood or sensitization to house dust mites between the two groups.
Given the significant difference in the prevalence of skin allergy history between the groups with and without a positive skin test, the clinical characteristics of the subjects were compared according to skin allergy history. There were no significant differences in age or employment duration between the subjects with a positive history of skin allergy (number=98) and those without (number=359); however, the duration of contact with antibiotics and duration of allergic diseases were significantly longer in the group with a positive skin allergy history (Fig. 1). The number of eosinophils in peripheral blood tended to be higher in the group with a positive skin allergy history than in the group without a positive history, but the proportion of subjects with an eosinophil count ≥450/mm3 was not significantly different between the groups (5.1 versus 2.2%; χ2=1.78; P=0.242). The frequencies of a positive drug allergy history (15.3 versus 3.6%; χ2=18.28; P=0.000), stage 1 CUS (14.4 versus 7.4%; χ2=4.33; P=0.038) and positive antibiotic skin test responders (6.9 versus 1.3%; χ2=7.15; P=0.018) were higher in the group with than without a positive skin allergy history. Stage 2 CUS (2.2 versus 0.3%; χ2=3.77; P=0.114]) and stage 1 localized urticaria (4.4 versus 2.1%; χ2=1.59; P=0.255) tended to be more prevalent in the group with a positive history (Fig. 2), but the differences between the groups with and without a positive history were not statistically significant.
The subjects with a drug allergy history (number=28) were significantly older and had a longer employment duration, longer duration of contact with antibiotics and higher prevalences of allergic rhinitis, night cough, food allergy and skin allergy compared with the subjects without a drug allergy history (number=429) (Table 4). Moreover, the grade of the skin test reactivity to D. farinae was significantly higher in the subjects with a drug allergy than in the other group.
According to the univariate analysis, the significant risk factors for a positive response to the drug skin tests were a positive history of skin allergy, stage 1 CUS (localized urticaria) and stage 2 CUS (generalized urticaria). The risk factors in the multivariate analysis were a positive history of drug allergy and localized stage 1 CUS (Table 5). According to the univariate analysis, the risk factors for stage 1 CUS were a positive history of any allergic disease, night cough, skin allergy and a positive response to the drug skin tests. Multivariate analysis showed the risk factors to be a positive history of any allergic disease and a positive response to the drug skin tests. For localized contact urticaria, the risk factors were a positive history of any allergic disease and positive response to the drug skin tests based on univariate analysis and a positive history of asthma and positive response to the drug skin tests based on multivariate analysis. According to the univariate analysis, allergic rhinitis, night cough, food allergy and skin allergy were risk factors for drug allergy. Age, allergic rhinitis, night cough and food allergy were the risk factors for drug allergy according to the multivariate analysis.
The positive response rate to the 6 antibiotics was 6.9% in nurses with a positive history of skin allergy, 1.3% in those without and 2.6% in all subjects. The prevalence of self-reported allergy to penicillin or other β-lactam antibiotics according to Gomes et al.21 was 6.0% in the general adult female population and the positive response rate to antibiotics in patients with a history of previous penicillin allergy was reported to be 14% by Solley et al.22 and 8.7% by Raja et al.23 Compared with these reported rates,21-23 the positive response rates in our study with nurses were relatively high.
The skin test response rate for a drug may be lower than the prevalence of an allergy history for that drug, because the positive response to a skin test will decrease as the antibody level decreases over time. Only 22% of patients with a penicillin allergy showed a positive skin test response to penicillin 10 years after exposure.24 The continual antibiotic exposure of the nurses in the present study may explain their higher positive response rate to antibiotic skin tests, compared with the rate of approximately 1% in the general adult population. Our results are supported by those of You et al.,25 who found that positive response rates to patch tests were 10% for cefotaxime, 10% for neomycin and as high as 50% for vancomycin in 40 intensive care unit nurses who were suspected of high exposure to antibiotics. Even excluding vancomycin, because it is well known to non-immunologically release histamine and thus induce "redman syndrome,"26 the positive response rates reported by You et al.25 were relatively high. Of course, the study methods used by You et al.25 differed from those in the present and previous studies.22,23 You et al.25 performed patch tests for T cell-mediated delayed adverse reactions and evaluated maculopapular and morbilliform skin rashes, a delayed reaction and common manifestation of drug allergy.3 In contrast, we and earlier investigators22,23 conducted prick or scratch skin tests for IgE-mediated immediate reactions such as urticaria. Barbaud et al.27 showed that in patients with cutaneous adverse reactions, the positive response rates to the drugs tested were 43% by the patch test and 24% by the skin prick test, suggesting a lower sensitivity for the skin prick test compared with the patch test. Furthermore, the prevalence of adverse reactions may differ between past and present cephalosporins; for example, the reaction rate to cephalosporin decreased from 10-20% to 2% when the second-generation drug was used instead of the firstgeneration drug, which showed cross-reactivity to penicillin.28 Considering these points, the sensitization rate to drugs may be higher in nurses than in the general population, owing to a more intense exposure of nurses to drugs.
In the present study, evidence for stage 1 CUS in response to an antibiotic was observed in 14.4% of the subjects with a positive skin allergy history, in 7.4% of those without and in 8.9% of all subjects; evidence for contact urticaria, in 4.4%, 2.1% and 2.6%, respectively; and evidence for stage 2 CUS, in 2.2%, 0.3% and 0.7%, respectively. It was difficult to discriminate between antibiotic-induced CUS and contact dermatitis caused by other factors. Allergic contact dermatitis develops 12-48 hours after dermal contact with allergens.18 In contrast, contact urticaria induced by antibiotics usually manifests within a few minutes and thus was apparent. All subjects with eczema on their hands were considered to have stage 1 CUS and given that some of these cases were probably contact dermatitis due to the other causes, the prevalence of stage 1 CUS would have been inflated. However, considering the cases of antibiotic-induced contact dermatitis beside contact urticaria, the prevalence of stage 1 would be higher than that of contact urticaria. Subjects with a positive skin test response to antibiotics showed a higher prevalence of stages 1 and 2 CUS, with 5.6 times the risk for stage 1 and 24.9 times the risk for contact urticaria compared with subjects without a positive skin test. This suggests that sensitization to antibiotics is strongly related to CUS.
Kim et al.29 reported a case with cold urticaria that progressed to exercise-induced anaphylaxis. CUS is a good example of similar events.17 This study was conducted as a fact-finding survey to prevent the progression of antibiotic-induced CUS. We identified two subjects with stage 2 CUS who had a positive skin test reaction to cefotiam, a second-generation cephalosporin. In Korea, since the first case report of cefotiam-induced CUS by Shin et al.9 in 1998, 10 cases of cefotiam-induced CUS have been reported.6,9-14,30 Cefotiam-induced CUS occurs mainly in nurses. Cefotiam is stored under vacuum; when the vacuum is released by a nurse, cefotiam becomes dispersed and is easily absorbed through damaged skin on the hands, where its irritative properties cause eczema.12 Owing to this peculiar property, cefotiam appears to not only induce progression to CUS but also facilitate secondary CUS induced by cefoprazone/sulbactam6 or imipenem.30 This phenomenon was observed in the present study: of the two cases of CUS sensitized to cefotiam, one was also sensitized to ceftizoxime and piperacillin and the other showed positive reactions to all antibiotics tested. However, the one case of CUS sensitized to flomoxef was not sensitized to the other antibiotics and did not progress to stage 2.
Compared with those without a positive skin allergy history, the subjects with a positive skin allergy history had longer durations of contact with antibiotics and of allergic diseases and higher prevalences of drug allergy, CUS and positive skin reactions to antibiotics. This may be attributable to the fact that skin allergy frequently develops in association with exposure and sensitization to antibiotics, which corresponds well with the results of a previous study by Gomes et al.,21 in which symptoms induced by β-lactam antibiotics occurred most frequently on the skin (63.5%), followed by the cardiovascular system (30.2%), bronchus (13.5%), eye/nose (11.5%) and gastrointestinal tract (6.3%). The skin lesions in Gomes et al.21 included skin rashes as well as urticaria and angioedema, and maculopapular or morbilliform rashes are the most common drug allergy.3 However, as we only asked about the occurrence of urticaria on the skin, many subjects probably reported maculopapular or morbilliform rashes caused by a T cell-mediated type IV hypersensitivity reaction as urticaria. Those with maculopapular rashes showed higher positive responses with the patch test,25 whereas urticaria is usually diagnosed by the skin prick test. If we had performed both the skin prick and patch tests, we might have obtained higher response rates and different results according to skin disease type. However, it was practical challenge to perform both tests on all subjects.
The subjects with a positive drug allergy history were older with longer durations of employment and contact with antibiotics and age was a significant risk factor for drug allergy, suggesting that long-term exposure to antibiotics may result in drug allergy. A positive drug allergy history was significantly correlated with allergic rhinitis, night cough, food allergy and skin allergy as well as sensitization to house dust mites. This indicates that a drug allergy may frequently occur in the skin and other organs in subjects with IgE-mediated allergic diseases such as allergic rhinitis, especially with sensitization to house dust mites. In contrast, when compared according to skin allergy, which included both IgE-mediated urticaria and T cell-mediated maculopapular rashes, the difference in the prevalence of IgE-mediated allergic diseases such as allergic rhinitis and positive skin reactions to house dust mites was not be significant, but the difference in the prevalence of CUS, which involves both mechanisms, was significant. A well-known study by Adkinson31 in 1984 reported that the rate of positive responses to the penicillin skin test was not high in atopic subjects. The present study found that atopy was significantly related to drug allergy. Recently, Apter et al.32 have also demonstrated that atopy, as well as interleukin-4 polymorphism, significantly correlates with drug allergy in patients with a self-reported penicillin allergy. A penicillin allergy can be induced by various types of allergic reactions in addition to an IgE-mediated reaction and therefore the statistical significance of the relationship between atopy and drug allergy in a given study may depend on the proportion of study subjects with an IgE-mediated allergic reaction. Once T cell-mediated eczema, a symptom of stage 1 CUS, has developed, IgE-mediated stages 2-4 CUS frequently occur after the subsequent absorption of allergens through damaged skin; furthermore, patients with skin contact allergy to multiple agents are easily sensitized to another agent and may more frequently present respiratory tract symptoms of an allergy.33 Different types of allergic mechanisms appear to augment each other.
This study had some limitations. First, we tested only six of the currently used antibiotics. Second, because only the skin prick test was performed, our results may underestimate the actual sensitization rates to antibiotics. To obtain more accurate results, it would be necessary to perform a patch test to detect T cell-mediated allergies and an intradermal test to improve the detection sensitivity for IgE-mediated allergies,27 as well as to observe late reactions 1 day after the intradermal test.19 Generally, for an intradermal test, cephalosporin is used at a 1:10 dilution, which does not induce an irritative reaction,34 whereas cephalosporin is often used without dilution for the skin prick test.19 In the present study, a 1:3 dilution was selected for most of the antibiotics used in the skin prick tests. Although this dilution helped to minimize the false-positive rate due to irritation, it created a third limitation, as the false-negative rate due to insufficient antibiotic concentrations might have been higher at this dilution. Fourth, because the excluded subjects had a higher probability for drug allergies, the skin test response rates in the nurse population may be underestimations. Additionally, the group of nurses who did not undergo skin tests had less frequent contact with injectable antibiotics; consequently, the overall sensitization rate based on the group of nurses who did undergo skin tests may be an overestimation. Lastly, female subjects have been shown to have a higher frequency of adverse drug reactions and a higher response rate to the penicillin skin test, compared with male subjects;35 thus, because almost all of our subjects were female, gender should be considered when interpreting our study results.
The results of this study suggest that because adverse reactions to antibiotics occur mainly as skin allergies through type I and IV hypersensitivity reactions, positive responses to antibiotic skin tests, CUS and drug allergies were more frequently observed in subjects with skin allergies than in those without. Based on our results that allergic rhinitis and food allergy were important risk factors for drug allergies, as was also shown in a recent study,32 even though drug allergy has been known not to be prevalent in atopic subjects, atopy may play a crucial role in the development of drug allergy.
Figures and Tables
Fig. 1
The duration of dermal contact with antibiotics, duration of any allergic diseases and eosinophil counts in peripheral blood in nurses with and without a positive history of skin allergy in a tertiary hospital.

Fig. 2
The proportion of subjects who had a positive history of drug allergy, the contact urticaria syndrome and a positive skin prick test response to β-lactam antibiotics in nurses with and without a positive history of skin allergy in a tertiary hospital.
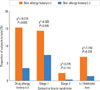
Table 2
Clinical characteristics of nurses who showed a positive response to skin prick tests using antibiotics
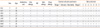
Table 3
Comparisons of clinical characteristics between positive and negative responders to antibiotic skin prick tests

ACKNOWLEDGMENTS
The authors are indebted to Dr. Kyung-Hee Jeong, Director of the Pharmaceutical Department, Chonnam National University Hospital for the gift of antibiotics used in this study.
References
1. Gomes ER, Demoly P. 111 Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol. 2005. 5:309–316.
2. Çelik G, Pichler WJ, Adkinson NF Jr. Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FER, editors. Drug allergy. Middleton's allergy. Principles and practice. 2009. 7th ed. Philadelphia: Mosby Elsevier;1205–1226. .
3. Schnyder B. Approach to the patient with drug allergy. Immunol Allergy Clin N Am. 2009. 29:405–418.
4. Romano A, Demoly P. Recent advances in the diagnosis of drug allergy. Curr Opin Allergy Clin Immunol. 2007. 7:299–303.
5. DeSwarte RD, Patterson R. Patterson R, Grammer LC, Greenberger PA. Drug allergy. Allergic diseases. 1997. 5th ed. Philadelphia: Lippincott-Raven;317–412.
6. Lee KH, Choi IS, Lee WJ, Kang SJ, Jeong HK. A case of cefotiam-contact anaphylaxis. Korean J Med. 2009. 76:Suppl 1. S238–S242. Korean.
7. Tadokoro K, Niimi N, Ohtoshi T, Nakajima K, Takafuji S, Onodera K, Suzuki S, Muranaka M. Cefotiam-induced IgE-mediated occupational contact anaphylaxis of nurses; case reports, RAST analysis, and a review of the literature. Clin Exp Allergy. 1994. 24:127–133.
8. Shimizu S, Chen KR, Miyakawa S. Cefotiam-induced contact urticaria syndrome: an occupational condition in Japanese nurses. Dermatology. 1996. 192:174–176.
9. Shin KY, Lee JY, Park CW, Lee CH. A case of cefotiam-induced contact urticaria syndrome. Korean J Dermatol. 1998. 36:1092–1095. Korean.
10. Shin HJ, Kim WS, Lee SY, Lee JS, Whang KU. A case of cefotiam-induced contact urticaria syndrome. Korean J Dermatol. 2005. 43:131–133. Korean.
11. Jang PM, Kim HJ, Kim YS, Cho YS, Lee JW, Yu KW, Lim H. Two cases of contact urticaria syndrome from cefotiam in nurses. J Korean Soc Clin Toxicol. 2006. 4:65–68.
12. Lee JY, Kim GI, Park CW, Lee CH. Two cases of cefotiam-induced contact urticaria syndrome. Ann Dermatol. 2000. 12:119–121.
13. Choi HJ, Song JY, Park YM, Kim CW, Kim HO. Occupational contact urticaria syndrome induced by cefotiam dihydrochloride in a nurse. Ann Dermatol. 2003. 15:113–115.
14. Jeong J, You K, Nahm S, Kim E. Anaphylaxis after epidermal contact with cefotiam hydrochloride. J Allergy Clin Immunol. 2006. 117:S227.
15. NIH Publication No. 97-4051. Expert panel report 3: guidelines for the diagnosis and management of asthma. Full Report 2007. 2007. Bethesda, MD: U.S. Department of Health and Human Services; National Institutes of Health; National Heart, Lung, and Blood Institute; National Asthma Education and Prevention Program.
16. Demoly P, Kropf R, Bircher A, Pichler WJ. Drug hypersensitivity: questionnaire. EAACI interest group on drug hypersensitivity. Allergy. 1999. 54:999–1003.
17. Von Krogh G, Maibach HI. The contact urticaria syndrome-an updated review. J Am Acad Dermatol. 1981. 5:328–342.
18. Gober MD, DeCapite TJ, Gaspari AA. Adkinson NF, Bochner BS, Busse WW, Holgate ST, Lemanske RF, Simons FER, editors. Contact dermatitis. Middleton's allergy. Principles and practice. 2009. 7th ed. Philadelphia: Mosby Elsevier;1105–1116.
19. Barbaud A, Goncalo M, Bruynzeel D, Bircher A. Guidelines for performing skin tests with drugs in the investigation of cutaneous adverse drug reactions. Contact Dermatitis. 2001. 45:321–328.
20. Adinoff AD, Rosloniec DM, McCall LL, Nelson HS. Immediate skin test reactivity to Food and Drug Administration-approved standardized extracts. J Allergy Clin Immunol. 1990. 86:766–774.
21. Gomes E, Cardoso MF, Praca F, Gomes L, Marino E, Demoly P. Self-reported drug allergy in a general adult Portuguese population. Clin Exp Allergy. 2004. 34:1597–1601.
22. Solley GO, Gleich GJ, Van Dellen RG. Penicillin allergy: clinical experience with a battery of skin-test reagents. J Allergy Clin Immunol. 1982. 69:238–244.
23. Raja AS, Lindsell CJ, Bernstein JA, Codispoti CD, Moellman JJ. The use of penicillin skin testing to assess the prevalence of penicillin allergy in an emergency department setting. Ann Emerg Med. 2009. 54:72–77.
24. Sullivan TJ, Wedner HJ, Shatz GS, Yecies LD, Parker CW. Skin testing to detect penicillin allergy. J Allergy Clin Immunol. 1981. 68:171–180.
25. You HS, So HS. A study on the prevalence of dermatitis and allergic reactions to medicine & disinfectant used by nurses. Chonnam J Nurs Sci. 2002. 7:19–34.
26. Polk RE, Healy DP, Schwartz LB, Rock DT, Garson ML, Roller K. Vancomycin and the red-man syndrome: pharmacodynamics of histamine release. J Infect Dis. 1988. 157:502–507.
27. Barbaud A, Reichert-Penetrat S, Trechot P, Jacquin-Petit MA, Ehlinger A, Noirez V, Faure GC, Schmutz JL, Bene MC. The use of skin testing in the investigation of cutaneous adverse drug reactions. Br J Dermatol. 1998. 139:49–58.
28. Madaan A, Li JT. Cephalosporin allergy. Immunol Allergy Clin North Am. 2004. 24:463–476. vi–vii.
29. Kim SH, Choi IS, Lee S, Jung SH, Seo SR, Mun JS, Han ER. A case of cold urticaria with exercise- and cold-induced anaphylaxis. Chonnam Med J. 2006. 42:140–143. Korean.
30. Seo E, Yoon TY, Jung JS, Jang EJ, Choi W, Kim MK. A case of contact urticaria syndrome induced by cefotiam and imipenem in atopic dermatitis patient. Korean J Asthma Allergy Clin Immunol. 2009. 29:217–220. Korean.
31. Adkinson NF Jr. Risk factors for drug allergy. J Allergy Clin Immunol. 1984. 74:567–572.
32. Apter AJ, Schelleman H, Walker A, Addya K, Rebbeck T. Clinical and genetic risk factors of self-reported penicillin allergy. J Allergy Clin Immunol. 2008. 122:152–158.
33. Schnuch A, Brasch J, Uter W. Polysensitization and increased susceptibility in contact allergy: a review. Allergy. 2008. 63:156–167.
34. Empedrad R, Darter AL, Earl HS, Gruchalla RS. Nonirritating intradermal skin test concentrations for commonly prescribed antibiotics. J Allergy Clin Immunol. 2003. 112:629–630.
35. Park MA, Matesic D, Markus PJ, Li JT. Female sex as a risk factor for penicillin allergy. Ann Allergy Asthma Immunol. 2007. 99:54–58.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download