Abstract
Objectives
To investigate the occurrence of glaucoma and association with the serum estradiol (E2) level in postmenopausal women.
Methods
We evaluated the serum E2 level, female reproductive factors and glaucoma related risk factors including intraocular pressure and optical coherence tomography (OCT) findings in 30 postmenopausal women who visited Obstetrics and Gynecology outpatient clinic. Patients who showed abnormal findings on the glaucoma screening test were classified to the glaucoma suspect group (group-G), and underwent a glaucoma confirmatory test. Serum E2 level, female reproductive and other menopausal health-related factors such as lipid profiles and bone mineral densities were analyzed in the group-G and non glaucomatous group (group-N).
Results
Eight out of thirty participants (26.7%) were classified to the group-G. One of them was diagnosed as having glaucoma that required treatment, and the other two were found to have early glaucomatous changes. Compared to the group-G, the group-N had a higher level of serum E2 (19.40 ± 4.79 vs. 13.95 ± 4.55 pg/mL) The difference, however, was not statistically significant (P = 0.525). The proportion of glaucoma suspect patients in the groups with a higher serum E2 level (≥ 20 pg/mL) and a lower serum E2 level (< 20 pg/mL) was similar (25.0 and 27.3%, P = 0.645). Multiple logistic regression analysis showed that no female reproductive factors were associated with the risk of glaucoma.
Figures and Tables
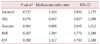
Table 2
Menopausal health related factors and frequency of glaucoma suspect by serum estradiol level

*Mean ± SE, †Number (%), ‡P value for Student's t test for continuous variables and Fisher's exact test for categorical variables.
LDL: low density lipoprotein, HDL: high density lipoprotein, TG: triglyceride, Glu: glucose, BMI: body mass index, BMD: bone mineral densities, IOP: intraocular pressure
References
1. Wei X, Cai SP, Zhang X, Li X, Chen X, Liu X. Is low dose of estrogen beneficial for prevention of glaucoma? Med Hypotheses. 2012; 79:377–380.
2. Altintaş O, Caglar Y, Yüksel N, Demirci A, Karabaş L. The effects of menopause and hormone replacement therapy on quality and quantity of tear, intraocular pressure and ocular blood flow. Ophthalmologica. 2004; 218:120–129.
3. Colton T, Ederer F. The distribution of intraocular pressures in the general population. Surv Ophthalmol. 1980; 25:123–129.
4. Qureshi IA. Intraocular pressure: a comparative analysis in two sexes. Clin Physiol. 1997; 17:247–255.
5. Sator MO, Joura EA, Frigo P, Kurz C, Metka M, Hommer A, et al. Hormone replacement therapy and intraocular pressure. Maturitas. 1997; 28:55–58.
6. Sator MO, Akramian J, Joura EA, Nessmann A, Wedrich A, Gruber D, et al. Reduction of intraocular pressure in a glaucoma patient undergoing hormone replacement therapy. Maturitas. 1998; 29:93–95.
7. Affinito P, Di Spiezio Sardo A, Di Carlo C, Sammartino A, Tommaselli GA, Bifulco G, et al. Effects of hormone replacement therapy on ocular function in postmenopause. Menopause. 2003; 10:482–487.
8. Russo R, Cavaliere F, Watanabe C, Nucci C, Bagetta G, Corasaniti MT, et al. 17Beta-estradiol prevents retinal ganglion cell loss induced by acute rise of intraocular pressure in rat. Prog Brain Res. 2008; 173:583–590.
9. Guttridge NM. Changes in ocular and visual variables during the menstrual cycle. Ophthalmic Physiol Opt. 1994; 14:38–48.
10. Park SK, Park DJ, Kim JS, Koo YH, Lee SR, Kim SH, et al. Association between serum estradiol level and intraocular pressure in postmenopausal women. J Korean Soc Menopause. 2007; 13:39–44.
11. Kim JM, Kim TH. Changes of urinary tract after menopause and effectiveness of menopausal hormone replacement therapy. J Korean Soc Menopause. 2011; 17:136–141.
12. Kim KH. Menopause and skin. J Korean Soc Menopause. 2011; 17:63–67.
13. Kim YS, Jung EY, Lee BY. The necessity of thyroid function test of perimenopausal women with menopausal symptoms. J Korean Soc Menopause. 2012; 18:174–179.
14. Kim CS, Seong GJ, Lee NH, Song KC. Prevalence of primary open-angle glaucoma in central South Korea the Namil study. Ophthalmology. 2011; 118:1024–1030.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download