Abstract
Objectives
This study was performed to assess the risk factors, histologic and clinical features of breast cancer in postmenopausal women receiving hormone therapy (HT).
Methods
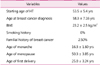
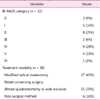
We evaluated 40 breast cancer patients who received HT due to postmenopausal symptoms by reviewing their medical charts at Pusan National University Hospital. Research variables, including patients' history, type and duration of received HT, moment of cancer debut after starting HT, radiological characteristics of breast cancer stage, histologic type, tumor size, grade, lymph node metastasis, estrogen and progesterone receptor status and 5-year survival were investigated.
Results
In the risk factors of breast cancer patients, only one patient had familial history of breast cancer. No patient had smoking history. The average body mass index (BMI) was 23.2 kg/m2. Twelve patients (30%) had estrogen only therapy, 13 patients (32.5%) had combined estrogen and progesterone therapy, 10 patients (25%) had tibolone therapy and the others consecutively received combination therapy of the above regimens. The mean duration of treatment was 31 ± 27.9 months (range 0.4-115 months). In the distribution of the cancer debut after starting HT, in 4 cases (10%) was within 1 year, 5 cases (12.5%) within 1-2 years, 10 cases (25%) within 2-3 years, 4 cases (10%) within 3-4 years, 1 case (2.5%) within 4-5 years, and 16 cases (40%) within more than 5 years. The average diameter of tumor size was 1.7 cm. In 92.5% of cases, the tumor was of ductal type. Tumor stage 0 and 1 appeared in 66% and grade I was present in 38% of investigated cases. Hormone receptor-positive breast cancers were 85% and 70% of patients had negative lymph node metastases. The 5-year survival rate was 92%.
Conclusion
The breast cancers which emerged during HT in postmenopausal women had hormone receptor-positive tendency. The size and stage of these breast cancers were shown as small and low, and represented low-grade differentiation. Recurrences of disease were uncommon and we found favorable 5-year survival rates and good prognosis.
Figures and Tables
References
1. McTiernan A, Martin CF, Peck JD, Aragaki AK, Chlebowski RT, Pisano ED, et al. Estrogen-plus-progestin use and mammographic density in postmenopausal women: Women's Health Initiative randomized trial. J Natl Cancer Inst. 2005. 97:1366–1376.
2. Boyd NF, Lockwood GA, Byng JW, Tritchler DL, Yaffe MJ. Mammographic densities and breast cancer risk. Cancer Epidemiol Biomarkers Prev. 1998. 7:1133–1144.
3. Byrne C, Schairer C, Brinton LA, Wolfe J, Parekh N, Salane M, et al. Effects of mammographic density and benign breast disease on breast cancer risk (United States). Cancer Causes Control. 2001. 12:103–110.
4. Byrne C, Schairer C, Wolfe J, Parekh N, Salane M, Brinton LA, et al. Mammographic features and breast cancer risk: effects with time, age, and menopause status. J Natl Cancer Inst. 1995. 87:1622–1629.
5. Ursin G, Ma H, Wu AH, Bernstein L, Salane M, Parisky YR, et al. Mammographic density and breast cancer in three ethnic groups. Cancer Epidemiol Biomarkers Prev. 2003. 12:332–338.
6. Ziv E, Tice J, Smith-Bindman R, Shepherd J, Cummings S, Kerlikowske K. Mammographic density and estrogen receptor status of breast cancer. Cancer Epidemiol Biomarkers Prev. 2004. 13:2090–2095.
7. Rossouw JE, Anderson GL, Prentice RL, LaCroix AZ, Kooperberg C, Stefanick ML, et al. Risks and benefits of estrogen plus progestin in healthy postmenopausal women: principal results From the Women's Health Initiative randomized controlled trial. JAMA. 2002. 288:321–333.
8. Beral V. Million Women Study Collaborators. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003. 362:419–427.
9. Hall P, Ploner A, Bjöhle J, Huang F, Lin CY, Liu ET, et al. Hormone-replacement therapy influences gene expression profiles and is associated with breast-cancer prognosis: a cohort study. BMC Med. 2006. 4:16.
10. The Study Group of Menopause. Clinical Characteristics of Breast Cancers Diagnosed in Korean Women on Hormone Therapy. J Korean Soc Menopause. 2009. 15:172–177.
11. McCormack VA, dos Santos Silva I. Breast density and parenchymal patterns as markers of breast cancer risk: a meta-analysis. Cancer Epidemiol Biomarkers Prev. 2006. 15:1159–1169.
12. McTiernan A, Chlebowski RT, Martin C, Peck JD, Aragaki A, Pisano ED, et al. Conjugated equine estrogen influence on mammographic density in postmenopausal women in a substudy of the women's health initiative randomized trial. J Clin Oncol. 2009. 27:6135–6143.
13. Stahlberg C, Pedersen AT, Andersen ZJ, Keiding N, Hundrup YA, Obel EB, et al. Breast cancer with different prognostic characteristics developing in Danish women using hormone replacement therapy. Br J Cancer. 2004. 91:644–650.
14. Nanda K, Bastian LA, Schulz K. Hormone replacement therapy and the risk of death from breast cancer: a systematic review. Am J Obstet Gynecol. 2002. 186:325–334.
15. Conroy SM, Pagano I, Kolonel LN, Maskarinec G. Mammographic density and hormone receptor expression in breast cancer: the Multiethnic Cohort Study. Cancer Epidemiol. 2011. 35:448–452.
16. Fournier A, Berrino F, Clavel-Chapelon F. Unequal risks for breast cancer associated with different hormone replacement therapies: results from the E3N cohort study. Breast Cancer Res Treat. 2008. 107:103–111.
17. Hammar M, Christau S, Nathorst-Böös J, Rud T, Garre K. A double-blind, randomised trial comparing the effects of tibolone and continuous combined hormone replacement therapy in postmenopausal women with menopausal symptoms. Br J Obstet Gynaecol. 1998. 105:904–911.
18. Kenemans P, Kubista E, Foidart JM, Yip CH, von Schoultz B, Sismondi P, et al. Safety of tibolone in the treatment of vasomotor symptoms in breast cancer patients--design and baseline data 'LIBERATE' trial. Breast. 2007. 16:Suppl 2. S182–S189.
19. Kenemans P, Bundred NJ, Foidart JM, Kubista E, von Schoultz B, Sismondi P, et al. Safety and efficacy of tibolone in breast-cancer patients with vasomotor symptoms: a double-blind, randomised, non-inferiority trial. Lancet Oncol. 2009. 10:135–146.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download