Abstract
Objectives
After Women's Health Initiative (WHI) study had been published, the use of hormone therapy (HT) have been decreasing even though it is the most effective therapy for menopausal symptom. The survey was conducted to investigate Korean menopausal women's perception of HT and behavior when they are treated by HT.
Methods
During 4 weeks from September 2009 to October 2009, total 600 women aged 45~64 participated in the survey by face to face interview. Out of answering women, women who have visited clinic/hospital at least 1 time to treat their menopausal symptom during last 1 year were included. One hundred fifty women for each age group, 45~49, 50~54, 55~59 and 60~64, were recruited in consecutive order.
Results
Eighty percent women who have visited clinic/hospital to treat menopausal symptom, visited obstetrics and gynecology. Only 16% of these women were current user, and other 84% of these women had no experience of HT (53%) or stopped therapy (31%). Among current user, only 9% of women have used HT more than 5 years. Eighty percent of current user had used HT less than 2 years. Most distressing menopausal symptom is 'hot flush' regardless HT experience. When doctor recommend HT, 72% of patients accept HT in overall. Among women who had no experience of HT, the most common reason of not to take HT was concern of side effects (51%). And 67% of women who had concern of side effects worried about cancer incidence.
Conclusion
Many women with menopausal symptom do not take HT even though it is the most effective therapy. Most of women who take HT stop treatment within 1 year. Most common reason of not to take HT is concern about side effect, increasing incidence of cancer related to HT. Therefore, HT should be considered to short-term relief of menopausal symptoms and at the minimal dose, if possible.
Hormone therapy (HT) for menopause is known as it alleviates vasomotor symptoms as well as mental, psychological symptoms that are experienced after the menopause, and as it manifests effects of preventing urogenital atrophy and protecting the bones and the cardiovascular system. It also has many benefits for the health of menopausal women as it owns beneficial effects on dementia or colorectal cancer. However, as a negative results of study on the secondary prevention of cardiovascular diseases by the Heart and Estrogen/progestin Replacement Study (HERS) in 1998 and as the risks for coronary disease, breast cancer and stroke came to the fore by the Women's Health Initiative (WHI) in 2002, the use of hormone for 2003 was reduced by 28% in comparison to the prior year in USA.1,2 Moreover, with the results of Million Women Study (MWS) being reported together with aforementioned study, there had been many debates on the HT for the post-menopausal women as its risks were more magnified than its benefits.3 However, WHI study or HERS study was conducted in the subjects whose mean ages were 63 and 67, who were more than 10 years from menopause, and in particular, HERS study had its limitation as it was conducted in the aged women with coronary diseases, those results could not be applied to all menopausal women.4 Therefore, in reality, HT was recommended as primary treatment for vasomotor symptoms with short-term use as possible.
After WHI study had been published, the use of HT have been decreased even though it has many advantages effective therapy for menopausal symptoms due to the conversion of perception on the HT. Also the use of HT has been decreased with reasons like worries on breast cancer and abnormal vaginal bleeding, many women had rejected the HT itself or stopped its use. To this end, this survey was conducted to investigate Korean menopausal women's response to perception of HT and their behaviors in women who had visited the hospital because of menopausal symptom.
This study was conducted in women whose ages were ranged being 45~64 who had visited the hospital to treat menopausal symptoms during 4 weeks from September 2009 to October 2009 through inquiries. The regions subjected to this study were Seoul, Gyeonggi-do, Incheon, Busan, Daejon, Daegu and Gwangu and the inquiries were made by face to face interview within 30 minutes performed in total 600 women aged 45~64 participated in the survey. The contents of inquiries were categorized largely into the menopausal symptoms and perception on them, treatment of menopausal symptoms and whether to visit the hospital, and HT for women and perception on it. Among the women who had visited the hospital, women younger than 45 as well as older than 65 years were excluded from the study subjects. And such inquiries were performed to the women experienced menopausal symptoms among those who were diagnosed as menopause from the hospital. The study was performed in total 600 women who were categorized into 4 groups by the age ranges into 45~49 group, 50~54 group, 55~59 group, and 60~64 group with 150 women for each group respectively. Out of answering women, residents of Seoul, Gyeonggi-do and Incheon was 71% while residents in Busan was 13% and 8% was from Taegu, and the residents in Daejon and Gwangu were 4% respectively. Sixty four percent of responders were full time housewives, 23% was self-business owner, 9% was employees of service business, 2% as office worker and 2% was skilled workers. As the academic background, 64% was high school graduate, 19% with junior high school graduate, 13% with university graduates and 5% with elementary graduates.
The mean age of subjects in this study for investigation was 54 years old and the mean menopausal age was 60 years old.
Forty-six percent of subject women had visited the hospital after experiencing menopausal symptoms within 1~3 months. Among the types of hospital for initial visits, 62% of them had visited private obstetrics and gynecology clinics as the most followed by 18% who visited to department of obstetrics and gynecology of the general hospitals, 12% visited the private internal medicine clinics and 4% to the private family medicine clinics. The private obstetrics and gynecology clinics had the most frequent visits of patients followed by the obstetrics and gynecology department in the general hospital, but such sequence had no association with ages or to the HT. As the main reason to visit the hospital, worries on any presence of abnormality in their health was the biggest one with 39%, and the symptoms severe enough to impair routine daily living was 20%, intolerable symptoms causing discomforts was 17% and 12% had visited the hospital by the recommendation from associates, and 6% was the cases who had visited the hospital for health examination.
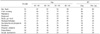
All women experienced menopausal symptoms and the most frequently experienced symptom was 'hot flush' with responses from 91% patients. Subsequent to the hot flash, the patients complained cold sweat, palpitation, depression, fatigue, myalgia/arthralgia pain, insomnia, sensory abnormality, frequent urination, memory impairments and sexual dysfunction in sequential order. In particular, 68% of patients complained severe hot flush with painfulness as the most frequently complained distressing menopausal symptom than any other symptoms, and there were many patients who felt this symptoms required treatment as 72%. The older patents had shown many profiles of experiencing hot flush, cold sweat, palpitation, fatigue, and memory impairments. And there were many patients showing profiles in the age group ranged being 60~64 more experiencing the most of menopausal symptoms in comparison to other age groups. In the group with age ranged being 55~59, the percentage of patients complaining more severe symptoms was higher than any other groups in regard to hot flush, cold sweat, palpitation, fatigue, and myalgia/arthralgia pain. The symptom of frequent urination did not show large differences by age groups in the percentage to complain its severity in comparison to other symptoms. On the other hand, higher the age gets, more cases had felt severe symptoms in connections with insomnia or memory impairments while two age groups of 45~49 and 60~64 had shown high percentage of patients experiencing severe symptoms of sexual dysfunction (Table 1).
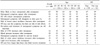
In the survey on perception of menopausal symptoms, 89% of subjects had felt the hot flush was the menopausal symptom and in addition 78% perceived the cold sweat as menopausal symptom while 74% perceived the sexual dysfunction as menopausal symptoms. Sixty-three percent of women were aware that osteoporosis develops after menopause, and the HT users had higher interest in the post-menopausal symptoms in comparison to the non-users, while most of thoughts on menopausal symptoms has shown similar pattern in each age groups. However, the percentage of responders answering that the menopausal symptoms disappears by time was 36% in the HT users and 52% in the non-users which was higher than the HT users (Table 2).
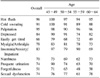
Fifty-three percent of women who had visited the hospital was those who never used the HT in the past, while 31% was those who had stopped HT after use and the currently users of HT continuously was 16%. Sixty percent of women who had visited the hospital due to menopausal symptoms had been recommended the use of HT, and among them 71% had accepted the HT and received the treatment. Thirty-three percent of them had begun the treatment from the date that they had visited the hospital, with 51% of them within 1 year treatment period. The higher the age range gets, the longer the treatment period of HT was in small differences (Table 3).
When subjected the HT user, the main reason to start the HT was alleviation of menopausal symptoms in 85% of them while 57% was those women ranged being 60~64 who had started the HT for prevention and treatment of osteoporosis, showing higher proportion than another age groups (Table 3).
Among 360 subjects who were recommended to use HT. One hundred fifty-nine subjects taking up 44% had been reluctant to beginning the HT or rejected it. The main reason was worries on cancer as shown from 40%, and 33% was due to the side effects such as weight gain, vaginal bleeding, gastrointestinal disturbance, 33% as considering the HT was not helpful, 21% feeling the burden from the cost of HT, and 4% was due to concerns on the cardiovascular disease.
Among the women visited the hospital for menopausal symptoms, the cases with experience of dietary and exercise therapies previously was 63% as the most percentage, followed by the cases who have had experience of receiving HT as 47%. In addition, they answered as prescribed with osteoporosis treatment agent, placenta extraction injection and phytoestrogen and etc. As far as the satisfaction level on the treatment method, in case of those experienced HT, it was 67%, while the satisfaction level on the dietary and exercise therapy was expressed as 21%, while the satisfaction level on the dietary and exercise therapy was expressed as 64% in non-users of HT, indicating that HT was more satisfactory treatment methods among the HT users, whereas the dietary and exercise therapy were more satisfactory treatments in the non-users of HT.
When compared the experiences, the perception, and their thoughts on the needs treatment between current HT user up to now as well as those who had been received the HT in the past but had stopped the use of hormone currently (n = 279) and those non users who had never experienced the HT (n = 321), the more number of HT user showed tendency of experiencing the most of menopausal symptoms more severely and of thinking that the treatment is required in comparison to the non-users of hormone. In case of hot flush, it was presented as 94% of the HT user and 89% of non HT users experience it with severe degree of symptoms felt by 77, 59% respectively. In addition, 93% of the HT user and 86% of non HT users had perceived hot flush as a menopausal symptom whereas 76% of the HT user and 69% of non HT users had felt that the treatment is required.
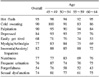
In the symptomatic improvement among the HT, the patients who had improvement in hot flush was the largest percentage as 96%, whereas the cases who had experienced improvement in fatigue or memory impairment were 66% and 51% that were smaller than percentages to feel improvements in other symptoms. Especially, as far as the myalgia/arthralgia pain, the improvement cases were small as the age range was increased (Table 4). For the satisfaction level on the symptomatic alleviation after having HT, it was also presented as having the highest satisfaction level for alleviation of hot flush as 95%, while the satisfaction level for memory impairment was the lowest as 54% (Table 5).
In case of experiencing the improvement in quality of life after having HT was 89% while the cases who were satisfied with the HT took up 90%. From the age groups, for the cases experienced the improvement in the quality of life, each age group of ranged being 45~49, 50~54, 55~59 and 60~64 had shown 97, 93, 85% and 84% respectively, while for the HT satisfaction level, the age groups of 45~49, 50~54, 55~59 and 60~64 had shown 98, 93, 87% and 83% respectively, presenting the pattern that higher the age range increased, the lower percentage of being satisfied with improvement in the quality of life or the HT gets.
Most of women who had never experienced the HT, answered that they had not used the hormone due to negative perception on the side effects of HT, and among them the negative perception on the development of cancer took up the highest proportion as 67%. This result was similar to the results that the worries on cancer when using HT was presented as the highest perception among 59.6% from a study in 307 women.5 In case of women who had stopped HT currently, most of them as 44% did not require the treatment any more as the symptoms were improved, while 26% of them had stopped after hearing on the side effects from friends and associates, 19% had stopped due to gain of body weight and 17% of them had stopped the HT due to such as gastrointestinal disturbances, Nonetheless, 78% of women who are actually using the HT was presented as not to experience any side effects except 14% of them experienced gain of body weight and 13% experienced the gastrointestinal disturbances.
Most of women whom were recommended with HT had informed from the doctor that HT can be beneficial to relieve hot flush, arthralgia, vaginal dryness (78%) and the proportion who answered such information had been acted as the most crucial factor in accepting and beginning HT took up the largest percentage as 41%. In addition, the answered that they were given with information that HT was important for supplementation of the lack of estrogen, that improves the quality of life deteriorated by insomnia or arthralgia, that it has cost-effectiveness in prevention and treatment of osteoporosis, that it does not cause cancer incurrence, and it does not increase the risk of breast cancer incidence when being used for the period less than 7 years.
This study had investigated on the behavior, perception and satisfaction on the HT in women who had visited hospital due to the menopausal symptoms.
The symptoms complained from the menopausal women were hot flush, palpitation, cold sweat, arthralgia, depression, insomnia, agitation and vaginal dryness and the most frequently experienced symptom is hot flush being presented from about 75% of menopausal women.6 As shown in this investigation, the hot flush was a menopausal symptom that may require treatment as it causes discomforts in daily life as the most common symptom in menopausal women regardless any previous HT experiences.
But physicians who recommend HT to the women who visited the hospital due to menopausal symptoms are about 60%, showing relatively low proportion. This seems that doctors themselves are concerns on side effects or the safety of long term use rather than many advantages that HT has as there is still room for debates on the safety of HT as far as the breast cancer or the coronary diseases.7 In particular, the most women visits the hospital due to hot flush as the main indication of menopausal symptoms, and as the relevance of hot flush with the cardiovascular disease had risen, in fact, the HT is not being strongly recommended.8,9 However, as the objective evidences enough to make conclusion on the relevance between the hot flush and the cardiovascular diseases are insufficient so far, HT can be recommendable in consideration of variables such as individual patient's age, time passage after menopause, life style or body mass index (BMI).2
The key factor to begin with HT for menopausal symptoms is the recommendation from physician, as approximately 72% of menopausal women had started the HT by the recommendation of doctor. This result supports that the recommendation of physician can be the most important factor in determination of HT in the menopausal women.10 Especially, the explanation that HT would be useful for alleviation of menopausal symptoms had been shown as the material factor in accepting HT. However, the doctor may do not have correct knowledge on the advantages of HT or its risks, or due to lack of information on the updates in the latest advancement, thereby it is possible for them unable to provide assurance to the patient on the treatment.
Even if once begun with HT, it was indicated as approximately 25% of them had stopped the HT and most of them had stopped the use of HT within 1 year. As the reasons, the most general reason was the improvement of symptoms, followed by the stories heard on the side effects from other significant persons around the patients. However, as the patients who had not experienced any side effects in actuality after using HT was 78%, proving if the prescribing doctor provides detailed explanation on the stability of HT and also provides additional information on the side effects possible during the follow-up period since the beginning of HT, that will be helpful in continuous use of HT a bit longer. Also for the women who desire to stop HT due to improvement of menopausal symptoms, it would be different depending on the specialized field or experiences of doctor for whether the HT should be stopped at the free will of patients with addition of recommending the dietary or exercise therapy, and if stopping the HP, in which method the discontinuity should be processed but there is no recommendation established.11
Currently used HT's types or administration routes are diversified, therefore, many studies are in progress on the long term advantages or side effects of each respective hormone agents, and they are subjected to the instigation of arguments. Therefore, recently it has been emphasized on the needs of individualized treatment depending each patients for performing menopausal HT of menopausal women by The North American Menopause Society or the International Menopause Society.2 From the result of this study, it was identified the most of menopausal women experiences hot flushes and they had chosen HT for the symptomatic alleviation, in addition that the satisfaction on the symptomatic relief and improvement in the quality of life were quite high, it is considered as desirable to use a short term HT as the individualized treatment for each patient.
Figures and Tables
Acknowledgements
This research was supported by Seoul St. Mary's Clinical Medicine Research Program year of 2009 through the Catholic University of Korea.
References
1. Hersh AL, Stefanick ML, Stafford RS. National use of postmenopausal hormone therapy: annual trends and response to recent evidence. JAMA. 2004. 291:47–53.
2. The North American Menopause Society. Estrogen and progestogen use in postmenopausal women: 2010 position statement of The North American Menopause Society. Menopause. 2010. 17:242–255.
3. Beral V. Breast cancer and hormone-replacement therapy in the Million Women Study. Lancet. 2003. 362:419–427.
4. Utian WH, Archer DF, Bachmann GA, Gallagher C, Grodstein F, Heiman JR, et al. Estrogen and progestogen use in postmenopausal women: July 2008 position statement of The North American Menopause Society. Menopause. 2008. 15:584–602.
5. Kim JG, Kim JW, Kim SH, Choi YM, Shin CJ, Moon SY, et al. A survey of menopausal women's attitudes on menopause and hormone replacement therapy. J Korean Soc Menopause. 1995. 1:42–50.
6. Sassarini J, Lumsden MA. Hot flushes: are there effective alternatives to estrogen? Menopause Int. 2010. 16:81–88.
7. Baumgartner AK, Hausler A, Seifert-Klauss V, Schuster T, Schwarz-Boeger U, Kiechle M. Breast cancer after hormone replacement therapy-does prognosis differ in perimenopausal and postmenopausal women? Breast. 2011. 20:448–454.
8. Rossouw JE, Prentice RL, Manson JE, Wu L, Barad D, Barnabei VM, et al. Postmenopausal hormone therapy and risk of cardiovascular disease by age and years since menopause. JAMA. 2007. 297:1465–1477.
9. Huang AJ, Sawaya GF, Vittinghoff E, Lin F, Grady D. Hot flushes, coronary heart disease, and hormone therapy in postmenopausal women. Menopause. 2009. 16:639–643.
10. Newton KM, Lacroix AZ, Leveille SG, Rutter C, Keenan NL, Anderson LA. The physician's role in women's decision making about hormone replacement therapy. Obstet Gynecol. 1998. 92:580–584.
11. Newton KM, Reed SD, Grothaus LC, La Croix AZ, Nekhlyudov L, Ehrlich K, et al. Hormone therapy discontinuation: physician practices after the Women's Health Initiative. Menopause. 2010. 17:734–740.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download