Abstract
Purpose
To develop staffing levels for nursing personnel (registered nurses and nursing assistants) to provide inpatients with integrated nursing care that includes, in addition to professional nursing care, personal care previously provided by patients' families or private caregivers.
Methods
A time & motion study was conducted to observe nursing care activities and the time spent by nursing personnel, families, and private caregivers in 10 medical-surgical units. The Korean Patient Classification System-1 (KPCS-1) was used for the nurse manager survey conducted to measure staffing levels and patient needs for nursing care.
Results
Current nurse to patient ratios from the time-motion study and the survey study were 1:10 and 1:11, respectively. Time spent in direct patient care by nursing personnel and family/private caregivers was 51 and 130 minutes per day, respectively. Direct nursing care hours correlated with KPCS-1 scores. Nursing personnel to patient ratio required to provide integrated inpatient care ranged from 1:3.9 to 1:6.1 in tertiary hospitals and from 1:4.4 to 1:6.0 in general hospitals. The functional nursing care delivery system had been implemented in 38.5% of the nursing units.
Figures and Tables
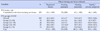
Table 1
Characteristics of Nursing Units, Number of Patients per Nursing Personnel by Shift, Work Hours, and Nursing Hours per Patient Day (N=80)

Table 2
Results from Time & Motion Study: Nursing Care Activities and Hours Provided by Team Nurses, Family Members, and Private Caregivers

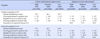
Table 4
Direct Nursing Care Hours Provided by Nursing Personnel, Family, and Private Caregivers, and the Relationship between Direct Nursing Care Hours and Patient Classification System (N=109)
References
1. Ministry of Health and Welfare (KR). Medical service act. Act No. 14438. 2016. 12. 20.
2. National Health Insurance Service (KR). National Health Insurance integrated nursing care program manual. Wonju: National Health Insurance Service;2016.
3. Cho SH, Kim YS, Yeon KN, You SJ, Lee ID. Effects of increasing nurse staffing on missed nursing care. Int Nurs Rev. 2015; 62(2):267–274. DOI: 10.1111/inr.12173.
4. Coffman JM, Seago JA, Spetz J. Minimum nurse-to-patient ratios in acute care hospitals in California. Health Aff (Millwood). 2002; 21(5):53–64. DOI: 10.1377/hlthaff.21.5.53.
5. State of California. California Code of Regulations [Internet]. 2017. cited 2017 January 12. Available from: http://www.dir.ca.gov/dlse/ccr.htm.
6. Royal College of Nursing. Mandatory nurse staffing levels. . London: Royal College of Nursing;2012.
7. National Institute for Health and Care Excellence (GB). Safe staffing for nursing in adult inpatient wards in acute hospitals [Internet]. updated July 2014. cited 2017 January 12. Available from: https://www.nice.org.uk/guidance/sg1.
8. American Nurses Association. Principles for nurse staffing. 2nd ed. Silver Spring, Maryland: American Nurses Association;2012.
9. Giovannetti P. Understanding patient classification systems. J Nurs Adm. 1979; 9(2):4–9.
10. Song KJ, Kim EH, Yoo CS, Park HO, Park KO. Development of KPCS (Korean Patient Classification System for Nurses) based on nursing needs. J Korean Clin Nurs Res. 2009; 15(1):5–17.
11. Song KJ, Kim EH, Yoo CS, Park HA, Song MS, Park KO. Verification of reliability and validity of KPCS-1 and estimation of nursing time conversion index. J Korean Clin Nurs Res. 2010; 16(2):127–140.
12. Kim SS, Chae GS, Kim KN, Park KO, Seong SM. Survey on nursing care delivery systems of university affiliated hospitals in Korea. J Korean Clin Nurs Res. 2010; 16(1):167–175.
13. Lankshear AJ, Sheldon TA, Maynard A. Nurse staffing and healthcare outcomes: A systematic review of the international research evidence. ANS Adv Nurs Sci. 2005; 28(2):163–174.
14. Bae SH, Fabry D. Assessing the relationships between nurse work hours/overtime and nurse and patient outcomes: Systematic literature review. Nurs Outlook. 2014; 62(2):138–156. DOI: 10.1016/j.outlook.2013.10.009.
15. Olds DM, Clarke SP. The effect of work hours on adverse events and errors in health care. J Safety Res. 2010; 41(2):153–162. DOI: 10.1016/j.jsr.2010.02.002.
16. Hendrich A, Chow MP, Skierczynski BA, Lu Z. A 36-hospital time and motion study: How do medical-surgical nurses spend their time? Perm J. 2008; 12(3):25–34.
17. Westbrook JI, Duffield C, Li L, Creswick NJ. How much time do nurses have for patients? A longitudinal study quantifying hospital nurses' patterns of task time distribution and interactions with health professionals. BMC Health Serv Res. 2011; 11:319. DOI: 10.1186/1472-6963-11-319.
18. Institute for Healthcare Improvement (US). Percent of nurse time spent in direct patient care [Internet]. cited 2017 January 12. Available from: http://www.ihi.org/resources/Pages/Measures/PercentNurseTimeSpentinDirectPatientCare.asp.
19. Royal College of Nursing. Accountability and delegation: What you need to know [Internet]. updated October 2011. cited 2017 January 12. Available from: https://www2.rcn.org.uk/__data/assets/pdf_file/0003/381720/003942.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download