Abstract
Purpose
To analyze the proportion of medical institutions meeting the legal standard for nurse staffing.
Methods
Data collected from 29,282 institutions between 1996 and 2013 were analyzed. Nurse staffing was measured as daily patient census per registered nurse (RN). The standard for general hospitals, hospitals, and clinics is 2.5 or less, and that for long-term care hospitals is 6.0 or less of the daily patient census per RN. Clinics may substitute nursing assistants for RNs by 50% or 100% depending on their daily inpatient census; long-term care hospitals may substitute nursing assistants for RNs by two thirds of the required number of RNs.
Results
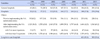
The proportion of general hospitals, hospitals, clinics, and long-term care hospitals meeting the standards was 63%, 19%, 63%, and 94%, respectively, in 2013. While general hospitals had an increase in the proportion during the 1996-2013 period, small changes were found in hospitals and clinics. In 2013, nurses were estimated to care for 16 (interquartile range: 12~24) patients per shift in general hospitals. Three quarters of clinics had no RNs in 2013.
Figures and Tables
Table 1
Proportion of General Hospitals, Hospitals and Clinics Meeting the Legal Standard for Nurse Staffing
References
1. Organisation for Economic Co-operation and Development. OECD Health Care Resources [Internet]. France: OECD;2015. cited 2015 November 30. Available from: http://stats.oecd.org/Index.aspx?DataSetCode=HEALTH_S TAT#.
2. Cho SH. Who forces patient families and informal caregivers to stay at the patient's bedside?: Providing holistic nursing care by improving nurse staffing. Paper presented at: Seoul National University Nursing Policy Forum. 2015 July 17; Seoul National University, Seoul.
3. National Health Insurance Service (KR). National Health Insurance comprehensive nursing care service program manual [Internet]. Sejong: Ministry of Health and Welfare (KR);2015. cited 2015 November 30. Available from: http://www.nhis.or.kr/bbs7/boards/B0040/14050.
4. Ausserhofer D, Zander B, Busse R, Schubert M, De Geest S, Rafferty AM, et al. Prevalence, patterns and predictors of nursing care left undone in European hospitals: Results from the multicountry cross-sectional RN4CAST study. BMJ Qual Saf. 2014; 23(2):126–135. DOI: 10.1136/bmjqs-2013-002318.
5. Kalisch BJ, Landstrom G, Williams RA. Missed nursing care: Errors of omission. Nurs Outlook. 2009; 57(1):3–9. DOI: 10.1016/j.outlook.2008.05.007.
6. Kohn LT, Corrigan J, Donaldson MS. To err is human: Building a safer health system. Washington: National Academy Press;2000.
7. Cho SH, Kim YS, Yeon KN, You SJ, Lee ID. Effects of increasing nurse staffing on missed nursing care. Int Nurs Rev. 2015; 62(2):267–274. DOI: 10.1111/inr.12173.
8. International Council of Nurses. Safe staffing saves lives: information and action tool kit. Geneva, Switzerland: International Council of Nurses;2006.
9. Kane RL, Shamliyan TA, Mueller C, Duval S, Wilt TJ. The association of registered nurse staffing levels and patient outcomes: systematic review and meta-analysis. Med Care. 2007; 45(12):1195–1204. DOI: 10.1097/MLR.0b013e3181468ca3.
10. Needleman J, Buerhaus PI, Stewart M, Zelevinsky K, Mattke S. Nurse staffing in hospitals: Is there a business case for quality? Health Aff (Millwood). 2006; 25(1):204–211. DOI: 10.1377/hlthaff.25.1.204.
11. Kim Y, Cho SH, June KJ, Shin SA, Kim J. Effects of hospital nurse staffing on in-hospital mortality, pneumonia, sepsis, and urinary tract infection in surgical patients. J Korean Acad Nurs. 2012; 42(5):719–729. DOI: 10.4040/jkan.2012.42.5.719.
12. Cho SH, Hwang JH, Kim J. Nurse staffing and patient mortality in intensive care units. Nurs Res. 2008; 57(5):322–322. DOI: 10.1097/01.nnr.0000313498.17777.71.
13. The National Assembly (KR). Medical service act [Internet]. 2015. [cited 2015 November 30. Available from: http://likms.assembly.go.kr/law/jsp/law/Main.jsp.
14. You SJ. Policy implications of nurse staffing legislation. J Korea Contents Assoc. 2013; 13(6):380–389. DOI: 10.5392/JKCA.2013.13.06.380.
15. Ministry of Health and Social Affairs (KR). Health and social white paper 1984. Gwacheon: Author.
16. Ministry of Health and Social Affairs (KR). Health and social white paper 1990. Gwacheon: Author.
17. You SJ, Chang HS, Kim MK, Choi YK. The utilization strategy of nursing personnel by types of medical institutions. Seoul: Korea Health Industry Development Institute;2005.
18. Ministry of Health and Welfare (KR). Reporting the results of the Healthcare Accreditation 2005 [Internet]. 2006. cited 2015 November 30. Available from: http://www.mohw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=37496&pag e=1.
19. Ministry of Health and Welfare (KR). Reporting the results of the Healthcare Accreditation 2006 [Internet]. 2007. cited 2015 November 30. Available from: http://www.mohw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=41228&pag e=1.
20. Oh YH. Supply and demand of health care workforce: 2015-2030. Sejong: Korea Institute for Health and Social Affairs;2014.
21. Kye HB, Doh SR, Song KY. Study on the improvement plan and survey design of patient survey. Seoul: Korea Institute for Health and Social Affairs;1996.
22. Doh SR, Jang YS, Jung YH, Choi JS, Oh YH, Oh MA, et al. Patient survey 2013. Sejong: Korea Institute for Health and Social Affairs;2013.
23. Kim D, Lee HJ. Effects on long-term care hospital staff mixing level after implementing differentiated inpatient nursing fees by staffing grades. J Korean Acad Nurs Adm. 2014; 20(1):95–105. DOI: 10.11111/jkana.2014.20.1.95.
24. Aiken LH, Sermeus W, Van den, Sloane DM, Busse R, McKee M, et al. Patient safety, satisfaction, and quality of hospital care: cross sectional surveys of nurses and patients in 12 countries in Europe and the United States. BMJ. 2012; 344:e1717. DOI: 10.1136/bmj.e1717.
25. Spetz J, Donaldson N, Aydin C, Brown DS. How many nurses per patient? Measurements of nurse staffing in health services research. Health Serv Res. 2008; 43(5 Pt 1):1674–1692. DOI: 10.1111/j.1475-6773.2008.00850.x.
26. Coffman JM, Seago JA, Spetz J. Minimum nurse-to-patient ratios in acute care hospitals in California. Health Aff (Millwood). 2002; 21(5):53–64.
27. Gerdtz MF, Nelson S. 5-20: a model of minimum nurse-to-patient ratios in Victoria, Australia. J Nurs Manag. 2007; 15(1):64–71. DOI: 10.1111/j.1365-2934.2006.00657.x1.




 PDF
PDF ePub
ePub Citation
Citation Print
Print






 XML Download
XML Download