Abstract
Purpose
The purpose of this study was to identify the impact of practical communication strategies (PCS) on the reduction of AEs (Adverse Events) in pediatric cardiac ICU (PCICU).
Methods
Intra-operative findings and care plans were documented and shared between staff members on a daily basis from the day of operation to the day of general ward transfer. Incidence of AEs was investigated in all patients who were admitted to the PCICU and was compared with incidence of AEs one year after establishment of PCS.
Results
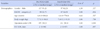
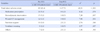
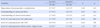
The study population consisted of 216 patients in pre-PCS group and 156 patients in post-PCS group. Incidence of readmission decreased from 6.0% (13/216) in pre-PCS group to 0.6% (1/156) in post-PCS group (χ2=7.23, p=.010). Incidence of other major complications decreased from 4.2% (9/216) to 0.6% (χ2=6.66, p=.012). Minor AEs such as intervention omission, order error, and protocol misunderstanding were reduced from 23.3 cases per 100 patient-days to 7.5 cases per 100 patient-days (χ2=20.31, p<.001).
Conclusion
Handover protocol is an effective strategy to reduce AEs for critically ill patients after pediatric cardiac surgery. Efforts to develop effective communication strategies should be continued and outcome research about communication strategies for patient safety should be further studied.
Figures and Tables
References
1. Sentinel Event Data: Root Causes by Event Type: 2004-Third Quarter 2011. The Joint Commission;2011. p. 20–21.
2. Donchin Y, Gopher D, Olin M, Badihi Y, Biesky M, Sprung CL, et al. A look into the nature and causes of human errors in the intensive care unit. Crit Care Med. 1995; 23(2):294–300.
3. Miller MR, Elixhauser A, Zhan C. Patient safety events during pediatric hospitalizations. Pediatrics. 2003; 111(6 Pt 1):1358–1366.
4. Muething SE, Goudie A, Schoettker PJ, Donnelly LF, Goodfriend MA, Bracke TM, et al. Quality improvement initiative to reduce serious safety events and improve patient safety culture. Pediatrics. 2012; 130(2):e423–e431. DOI: 10.1542/peds.2011-3566.
5. Agarwal S, Classen D, Larsen G, Tofil NM, Hayes LW, Sullivan JE, et al. Prevalence of adverse events in pediatric intensive care units in the United States. Pediatr Crit Care Med. 2010; 11(5):568–578. DOI: 10.1097/PCC.0b013e3181d8e405.
6. Larsen GY, Donaldson AE, Parker HB, Grant MJ. Preventable harm occurring to critically ill children. Pediatr Crit Care Med. 2007; 8(4):331–336. DOI: 10.1097/01.pcc.0000263042.73539.99.
7. Rothschild JM, Landrigan CP, Cronin JW, Kaushal R, Lockley SW, Burdick E, et al. The Critical Care Safety Study: The incidence and nature of adverse events and serious medical errors in intensive care. Crit Care Med. 2005; 33(8):1694–1700.
8. Barach P, Johnson JK, Ahmad A, Galvan C, Bognar A, Duncan R, et al. A prospective observational study of human factors, adverse events, and patient outcomes in surgery for pediatric cardiac disease. J Thorac Cardiovasc Surg. 2008; 136(6):1422–1428. DOI: 10.1016/j.jtcvs.2008.03.071.
9. Nathan M, Liu H, del Nido P, Pigula F, Thiagarajan R, Bacha EA. Intraoperative adverse events can be compensated by technical performance in neonates and infants after cardiacsurgery: A prospective study. J Thorac Cardiovasc Surg. 2011; 142:1098–1107. DOI: 10.1016/j.jtcvs.2011.07.003.
10. Kitch BT, Cooper JB, Zapol WM, Marder JE, Karson A, Hutter M, et al. Handoffs causing patient harm: A survey of medical and surgical house staff. Jt Comm J Qual Patient Saf. 2008; 34(10):563–570.
11. Pezzolesi C, Schifano F, Pickles J, Randell W, Hussain Z, Muir H, et al. Clinical handover incident reporting in one UK general hospital. Int J Qual Health Care. 2010; 22(5):396–401. DOI: 10.1093/intqhc/mzq048.
12. Riesenberg LA, Leitzsch J, Cunningham JM. Nursing handoffs: A systematic review of the literature. Am J Nurs. 2010; 110(4):24–34. quiz 5-6DOI: 10.1097/01.naj.0000370154.79857.09.
13. Lane D, Ferri M, Lemaire J, McLaughlin K, Stelfox HT. A systematic review of evidence-informed practices forpatient care rounds in the ICU. Crit Care Med. 2013; 41(8):2015–2029. DOI: 10.1097/CCM.0b013e31828a435f.
14. Resar RK, Rozich JD, Simmonds T, Haraden CR. A trigger tool to identify adverse events in the intensive care unit. Jt Comm J Qual Patient Saf. 2006; 32(10):585–590.
15. Thiagarajan RR, Bird GL, Harrington K, Charpie JR, Ohye RC, Steven JM, et al. Improving safety for children with cardiac disease. Cardiol Young. 2007; 17:Suppl 2. 127–132. DOI: 10.1017/S1047951107001230.
16. Joy BF, Elliott E, Hardy C, Sullivan C, Backer CL, Kane JM. Standardized multidisciplinary protocol improves handover of cardiac surgery patients to the intensive care unit. Pediatr Crit Care Med. 2011; 12(3):304–308. DOI: 10.1097/PCC.0b013e3181fe25a1.
17. Zavalkoff SR, Razack SI, Lavoie J, Dancea AB. Handover after pediatric heart surgery: A simple tool improves information exchange. Pediatr Crit Care Med. 2011; 12(3):309–313. DOI: 10.1097/PCC.0b013e3181fe27b6.
18. Agarwal S, Frankel L, Tourner S, McMillan A, Sharek PJ. Improving communication in a pediatric intensive care unit using daily patient goal sheets. J Crit Care. 2008; 23(2):227–235. DOI: 10.1016/j.jcrc.2007.07.001.
19. Pronovost P, Berenholtz S, Dorman T, Lipsett PA, Simmonds T, Haraden C. Improving communication in the ICU using daily goals. J Crit Care. 2003; 18(2):71–75. DOI: 10.1053/jcrc.2003.50008.
20. Cornell P, Townsend-Gervis M, Vardaman JM, Yates L. Improving situation awareness and patient outcomes through interdisciplinary rounding and structured communication. J Nurs Adm. 2014; 44(3):164–169. DOI: 10.1097/nna.0000000000000045.
21. Jacobs JP, Benavidez OJ, Bacha EA, Walters HL, Jacobs ML. The nomenclature of safety and quality of care for patients with congenital cardiac disease: A report of the Society of Thoracic Surgeons Congenital Database Taskforce Subcommittee on Patient Safety. Cardiol Young. 2008; 18:Suppl 2. 81–91. DOI: 10.1017/s1047951108003041.
22. Jenkins KJ, Gauvreau K, Newburger JW, Spray TL, Moller JH, Iezzoni LI. Consensus-based method for risk adjustment for surgery for congenital heart disease. J Thorac Cardiovasc Surg. 2002; 123(1):110–118.
23. Kim J. Epidemiology Principle. Fifth ed. Seoul: Sinkwang;2003. 25, July, 2002.
24. Chen JG, Wright MC, Smith PB, Jaggers J, Mistry KP. Adaptation of a postoperative handoff communication process for children with heart disease: A quantitative study. Am J Med Qual. 2011; 26(5):380–386. DOI: 10.1177/1062860610394342.
25. Townsend-Gervis M, Cornell P, Vardaman JM. Interdisciplinary rounds and structured communication reduce readmissions and improve some patient outcomes. West J Nurs Res. 2014; 36(7):917–928. DOI: 10.1177/0193945914527521.
26. Agarwal HS, Saville BR, Slayton JM, Donahue BS, Daves S, Christian KG, et al. Standardized postoperative handover process improves outcomes in the intensive care unit: A model for operational sustainability and improved team performance. Crit Care Med. 2012; 40(7):2109–2115. DOI: 10.1097/CCM.0b013e3182514bab.
27. Pronovost PJ, Jenckes M, To M, Dorman T, Lipsett PA, Berenholtz S, et al. Reducing failed extubations in the intensive care unit. Jt Comm J Qual Improv. 2002; 28(11):595–604.
28. Centofanti JE, Duan EH, Hoad NC, Swinton ME, Perri D, Waugh L, et al. Use of a daily goals checklist for morning ICU rounds: A mixed-methods study. Crit Care Med. 2014; 42(8):1797–1803. DOI: 10.1097/ccm.0000000000000331.
29. Narasimhan M, Eisen LA, Mahoney CD, Acerra FL, Rosen MJ. Improving nurse-physician communication and satisfaction in the intensive care unit with a daily goals worksheet. Am J Crit Care. 2006; 15(2):217–222.
30. Clarke CM, Persaud DD. Leading clinical handover improvement: A change strategy to implement best practices in the acute care setting. J Patient Saf. 2011; 7(1):11–18. DOI: 10.1097/PTS.0b013e31820c98a8.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download