Abstract
Purpose
The purpose was to compare operating room (OR) nurses and general ward nurses on their communication competence and interpersonal relationship ability within the medical team.
Methods
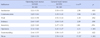
Participants were 276 nurses (OR 122, ward 154) working in one of 4 university hospitals located in I and K areas. Data were collected using a questionnaire and data collection was done in June, 2013. Comparisons between OR nurses and general ward nurses on communication competence and interpersonal relationship ability were analyzed using ANCOVA.
Results
There were statistically significant differences between the two groups in communication competence (F=11.96, p=.001) with average score for OR nurses at 3.37 points and ward nurses at 3.53 points. There were statistically significant differences between the two groups in interpersonal relationship ability (F=15.51, p<.001) with the average score for OR nurses at 3.30 points and ward nurses at 3.50 points.
Figures and Tables
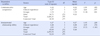
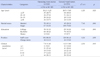
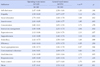
Table 2
Differences in Communicative Competence and Interpersonal Relationship Ability between Operation Room Nurses and General Ward Nurses (N=276)
References
1. Caldeira SM, Avila MAG, Braga EM. Educational and cultural activities in surgical and anesthetical recovery center: perception of the nursing team. J Nurs UFPE. 2013; 7(8):5232–5238.
2. Kim JO, Kim HJ, Cho GY. A study on the perception of medical technology, self efficacy and professional self-concept among operating nurses. Korean J Health Serv Manag. 2012; 6(1):1–13. http://dx.doi.org/10.12811/kshsm.2012.6.1.001.
3. Yoon K. A study on the job satisfaction and organizational commitment among perioperative nurses. J Korean Acad Nurs Adm. 2010; 16(1):86–100. http://dx.doi.org/10.11111/jkana.2010.16.1.86.
4. Roh YH, Yoo YS. Workplace violence, stress, and turnover intention among Perioperative nurses. Korean J Adult Nurs. 2012; 24(5):489–498. http://dx.doi.org/10.7475/kjan.2012.24.5.489.
5. Higgins BL, MacIntosh J. Operating room nurses perceptions of the effects of physician-perpetrated abuse. Int Nurs Rev. 2010; 57(3):321–327. http://dx.doi.org/10.1111/j.1466-7657.2009.00767.x.
6. Yoon KS, Park SA. Development and validation of an instrument to measure the job satisfaction of perioperative nurses. J Korean Clin Nurs Res. 2009; 15(1):93–106.
7. Bigony L, Lipke TG, Lundberg A, McGraw CA, Pagac GL, Rogers A. Lateral violence in the perioperative setting. AORN J. 2009; 89(4):688–696. http://dx.doi.org/10.1016/j.aorn.2009.01.029.
8. Kim EY. A study on the impact relationship between communication and job satisfaction in a medical organization: Focusing on operating room nurses [master's thesis]. Bucheon: The Catholic University of Korea;2011. 80.
9. Salmon P, Young B. Dependence and caring in clinical communication: The relevance of attachment and other theories. Patient Educ Couns. 2009; 74(3):331–338. http://dx.doi.org/10.1016/j.pec.2008.12.011.
10. Dingley C, Daugherty K, Derieg MK, Persing R. Improving patient safety through provider communication strategy enhancements. In : Henriksen K, editor. Agency for Healthcare Research and Quality. Advances in patient safety: New directions and alternative approaches. v.3, Performance and tools. Rockville, MD: Agency for Healthcare and Research Quality;2008.
11. Wloszczak-Szubzda A, Jarosz MJ. Professional communication competences of nurses-a review of current practice and educational problems. Ann Agric Environ Med. 2013; 20(1):183–188.
12. Im SI, Park J, Kim HS. The effects of nurse's communication and self-leadership on nursing performance. Korean J Occup Health Nurs. 2012; 21(3):274–282. http://dx.doi.org/10.5807/kjohn.2012.21.3.274.
13. Shin HH. The impact of doctors' communication styles on patient's self-disclosure. Daehan J Bus. 2011; 24(1):179–198.
14. Hur GH. Construction and validation of a global interpersonal communication competence scale. Korean J Journal Commun Stud. 2003; 47(6):380–408.
15. Lee HS, Kim JK. Relationship among communication competence, communication types, and organizational commitment in hospital nurses. J Korean Acad Nurs Adm. 2010; 16(4):488–496. http://dx.doi.org/10.11111/jkana.2010.16.4.488.
16. Guerney BG. Relationship enhancement: [skill-training programs for therapy, problem prevention, and enrichment]. San Francisco: Jossey-Bass;1977.
17. Moon SM. A study on the effect of human relations training of university students. J Gyeongsang Natl Univ. 1980; 19:195–203.
18. Chun SK. A study on the effectiveness of social skills training program for rehabilitation of the schizophrenic patients [dissertation]. Seoul: Soongsil University;1995. 87.
19. Son YJ, Lee Y, Sim KN, Kong SS, Park YS. Influence of communication competence and burnout on nursing performance of intensive care units nurses. J Korean Acad Fundam Nurs. 2013; 20(3):278–288. http://dx.doi.org/10.7739/jkafn.2013.20.3.278.
20. Lingard L, Espin S, Whyte S, Regehr G, Baker GR, Reznick R, Bohnen J, Orser B, Doran D, Grober E. Communication failures in the operating room: An observational classification of recurrent types and effects. Qual Saf Health Care. 2004; 13(5):330–334. http://dx.doi.org/10.1136/qshc.2003.008425.
21. Im S, Kim EK. Interpersonal communication competence and difficult communication experiences of preceptor nurses. J Korean Acad Psychiatr Ment Health Nurs. 2008; 17(4):471–480.
22. Buback D. Assertiveness training to prevent verbal abuse in the OR. AORN J. 2004; 79(1):148–150. 153–158. 161–164. http://dx.doi.org/10.1016/S0001-2092(06)61149-6.
23. Nam KD, Yoon KS, Chung HS, Park SA, Jang BY, Kim HR, et al. A study on the development of verbal abuse scale for operating room nurses. J Korean Acad Nurs Adm. 2005; 11(2):159–172.
24. Kim MH. An ethnographic research about daily work experiences of operating room nurses [master's thesis]. Seoul: Hanyang University;2006. 47–49.
25. Jackson S, Brady S. Counting difficulties: Retained instruments, sponges, and needles. AORN J. 2008; 87(2):315–321. http://dx.doi.org/10.1016/j.aorn.2007.07.023.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download