Abstract
Purpose
In order to provide a systematic and standardized treatment course for MVD patients, a critical pathway (CP) program was developed and the results of its long term application were analyzed.
Methods
This was a methodological study. The CP was established and applied to 75 (step I) and 1,216 (step II). Another group of 56 with similar features was used as a control group.
Results
The application of CP turned out to be useful in many regards: the rate of hearing loss was reduced from 1.8% to 0% (step I) and 0.5% (step II), and low cranial nerve palsy was reduced from 1.8% to 1.3% and 0.7%, respectively. The length of hospitalization decreased by 2.56 days (25.2%) for step I and 3.05 days (30.0%) for step II. Days of ICU stay were reduced by 7.9% and 1.8%. The total cost per patient was reduced by 14.8% (step I). The cost per day was increased by 13.7% and 52.4%. An increase in the patient satisfaction index was noted, as shown in the ICU information guide (p=.002).
Microvascular decompression (MVD) is the standard treatment for hyper-functioning disorders of the cranial nerve roots such as hemifacial spasm (HFS) and trigeminal neuralgia (TN) (Li et al., 2004; Mauriello et al., 1996; McLaughlin et al., 1999; Mustafa, Weerden, & Mooij, 2003; Wang & Jankovic, 1998). HFS is an involuntary movement disorder in which spasms occur on one half of the face. Although this disease begins in the region around the eye, involuntary muscle spasms usually progress to involve the whole face, particularly around the eye, mouth, and even the neck (Wang & Jankovic, 1998). By way of contrast, TN creates intense pain along the branches of the trigeminal nerve that control facial senses. For the accurate diagnosis and effective treatment of these conditions, great efforts have been made by medical personnel and various diagnostic tools such as 3D spin echo magnetic resonance imaging (MRI) and electromyography (EMG) have been employed in attempts to achieve a successful treatment regimen.
Prior to the implementation of the critical pathway (CP), no standard guidelines had been established and public education was insufficient. In addition, the following problems existed. When patients visited the hospital for the first time, they were often subjected to great inconveniences; for example, some patients had to wait for very long times to receive examinations or treatment, and also frequently had to visit the clinic many times. Additionally, patients occasionally lacked information regarding the treatment process and the relevant operative risks. On the other hand, discomfort levels remained high until all spasms had completely disappeared after surgery (Goto, Matsushima, Natori, Inamura, & Tobimatsu, 2002; Ishikawa, Nakanishi, Takamiya, & Namiki, 2001; Samii et al., 2002). In such cases, finding a solution and preventing the commonly-encountered discomforts might prove helpful in reducing hospitalization periods, in addition to elevating patient satisfaction levels (Isla-Guerrero et al., 2001). Some studies have reported that a post-endoscopy checklist reduced the length of stay for non-variceal upper gastrointestinal bleeding (Romagnuolo et al., 2005), and that standardized patient care using a CP reduced length of stay and complication rates following bariatric surgery (Kim, 2010a; Yeats, Wedergren, Fox, & Thompson, 2005; Van Vliet et al., 2011; Zhang & Liu, 2011).
Therefore, the principal objective of this study was to enhance management efficiency during hospitalization and patient satisfaction via the use of a standard medical treatment guide for MVD. We also evaluated the treatment steps via the continuous application of these guidelines. In particular, the long-term investigation conducted to validate the usefulness and efficacy of MVD CP.
This study was conducted to provide an effective management protocol for MVD patients. This was a methodological study (quasi-experimental study and long term survey). We compared 56 patients treated in the period prior to CP commencement from January 2001 to December 2001, 75 patients applied during the period from July 2002 to December 2002 (step I), and 1,216 patients were treated during the period spanning January 2003 to December 2009 (step II). The samples used in this study were selected as the total number of patients that received MVD for HFS or TN during the study period.
This study was conducted at a single institute in Korea. The setting for this study was a neurosurgical unit which included an outpatient unit, general wards, and an intensive care unit (ICU). To assess the mean differences among the three groups with regard to complications (step I: 1, step II: 5, SD: 1.0) and hospital duration (step I: 2.5, step II: 3, SD: 2), the sample size of each group was required to achieve a significance level of 0.05, with a power of 90%. The quality of treatment was evaluated in terms of the frequency of complications. The efficacy of hospital management was evaluated by the length of stay in hospital, the length of stay at the ICU, the total cost per patient, and the cost per day. CP application was evaluated via variation analysis (step I and the year 2003) and measurements of patient satisfaction.
In January 2002, with the objectives of establishing medical treatment flow and efficacy improvement, a team unit was comprised of 14 members (neurosurgeon 2, professor of nursing school 1, nurse managers 2, registered nurses 4 [neurosurgical ICU 1, general wards 2, and outpatient unit 1], clinical nurse specialist [CNS] 1, laboratory technicians 3, and hospital administrator 1). This team established a plan and studied the task by attending lectures and via a literature review.
After careful study, we established a standard treatment guide for MVD. The team then evaluated treatment progress by reviewing the relevant documents and charts. The medical records of 15 patients with MVD during the January-December 2000 period who fulfilled the selection criteria were reviewed. Medical record analysis consisted of 73 items (8 items on measures/observations, 3 items on activity/rest, 4 items on diet/nutrition, 23 items on medication, 14 items on laboratory test, 12 items on treatment, 2 items on interdepartmental consult and 7 items on patient education). A pilot CP was composed from the literature review, modification of preexisting CP for other diseases, and the opinion of the medical team. The x-axis of the pilot CP represented the time-frame, whereas the y-axis interpolated the treatment and nursing items. The devised CP was a systematically organized schedule that runs from the time of initial visit to the clinic to the time of discharge, and was designed to assist in decisions made concerning observation and measurement, activity, diet, medication, lab & tests, treatments & procedures, consultation, and education. That table was completed by placing the dates in rows and eight items in a column. All data were registered in the database, and the practitioners were able to easily use the package.
Each item was finalized after evaluation by staff nurses and neurosurgeon, validation by professionals group (neurosurgeon 2, professor of nursing school 1, nurse managers 2, registered nurses 4, CNS 1), and the approval of the CP development team. Five neurosurgeons and 62 nurses were recruited and educated regarding the objective of the study, the concept of CP, the development and application of CP, patient/family educating methods, and variations. In order to analyze its clinical adaptability, the pilot CP went through 17 experimental cases before its completion into a final MVD CP. To analyze the variations occurring during the application of CP, a clarification of the modified variation record was used (Beyea, 1996). The CP for patients was developed such that it could be readily understood by patients using simple words and pictures.
Additionally, we planned an intra-operative monitoring system (facial evoked EMG and brainstem auditory evoked potential [BAEP]) that was used to assess the intra-operative status of muscles and nerves.
A website was developed by the CP team to provide information. The associated educational information system was composed of an educational brochure that included a CP for patients and a website (http://facialspasm.samsunghospital.com). Education regarding disease and treatment was provided to patients at the outpatient clinic throughout the hospitalization period using an educational brochure and a website.
We analyzed independent variables affecting treatment and economic outcome, which included the incidence of complications, length of hospitalization, individual medical costs, the number of operations, CP variations, and patient satisfaction prior to and after CP initiation. Postoperative complications were monitored continuously by the neurosurgeon and the nurse. The hearing loss was confirmed by audiometry on the third day after surgery. Additionally, the low cranial nerve palsy was examined by ear, nose, and throat (ENT) doctors. The number of operations was defined as the total number of patients that received MVD for HFS or TN. Length of hospitalization was defined as the total number of days spent in hospital., including the ICU and excepting outpatient department (OPD) visits. ICU stay was computed from entry into the unit until transfer to the general ward. Medical costs per person were defined as the total charges incurred during the hospital stay. The daily treatment cost was defined as the cost per patient per day, and was calculated by dividing the total treatment cost by the days of stay.
Step I variation analysis was categorized into three groups: 'type', 'detailed fact', and 'grade'. The type of variation was classified into patient/family, medical attendance, and hospital. The detailed fact was classified into assessment, test, treatment, medication, diet, activity, interdepartmental cooperative treatment, nursing/education, discharge plan, record, treatment schedule, and communication. The grade category was divided into three degrees: grade 1, a slight change occurred, but was still correspondent to CP; grade 2, a slight change not correspondent to CP, but the CP still could be used; grade 3, the proper application of CP was impossible (Kim, 2010a). Step II variation analysis was recorded in terms of change content by CNS.
A patient satisfaction questionnaire was developed to evaluate the quality of care provided in the hospital. Patient satisfaction with the care provided by various health care professionals was measured with five-point questions. A score of 5 was very satisfactory and a score of 1 was not satisfactory. The tool consisted of 12 items, and the reliability as measured by Cronbach's α value was .912.
We applied and evaluated the guidelines for step I and step II. Compared with the period of step I, improvements were noted in the period of step II, such as a revision of CP, modification of contents in the educational material and website, increased research work, and strengthened teamwork. Difficulties in communicating ensued upon changes in team members. We communicated continuously about variances between team members, and CNS provided information about new members.
The study was conducted after obtaining approval from the ethical committee of our hospital. In addition, permission to conduct this study was obtained from the board of directors of the nursing department.
The statistical analysis system version 19.0 (SPSS Inc., Chicago, IL, USA) was used for analysis. Based on these data, we carried out statistical analysis using χ2 with Fisher's exact tests and one-way ANOVA with Bonferroni's correction. Variation was analyzed by frequency and percentage. Patient satisfaction was analyzed via ANOVA. Reliability was analyzed by Cronbach's α.
A barometer for the evaluation of the effects of the CP model application was designated. The x-axis represents the chronological process of 8 days of hospital stay, with details on daily treatment and nursing. The y-axis of the final CP consists of observation and measurement, activity, diet, medication, lab & tests, treatment/procedures, consultation, and education. Development and implementation took place over a total of 7 years (Figure 1).
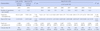
The 56 patients before the application of CP, the 75 patients during step I, and the 1,216 patients during step II comprised the study cohort, which consisted of 402 (29.8%) men and 945 (70.2%) women, with a mean age of 49.7 years (age range 19 to 79 years). No significant differences were noted between groups in terms of (step I, step II); age (p=.620, p=.313), gender (p=.569, p=.761), diagnosis (p=1.000, p=.167), symptom location (p=.294, p=.418), symptom duration (p=.887, p=.912), hypertension history (p=.641, p=.278) and diabetes mellitus (p=.423, p=.515) (Table 1).
We found that the incidence of hearing loss was reduced from 1 (1.8%) in the control group to 0 (0.0%) for step I and to 6 (0.5%) for step II. However, these differences were not found to be significant (p=.421, p=.272). The incidence of lower cranial nerve palsy was reduced from 1 (1.8%) in the control group to 1 (1.3%) for step I and to 8 (0.7%) for step II; these differences were not significant (p=1.000, p=.331). No decrease in delayed facial palsy (transient) was noted (p=1.000, p=.312) (Table 2).
The number of operations was 4.6 (per month) in the control group, and increased to 12.5 for step I and to 14.3 for step II. The mean number of operations for step II increased by 9.7 (210.0%) compared to 2001, averaging 173.7 patients a year. The total days of hospital stay was shortened by 2.56 days (25.2%) for step I (p<.001) and 3.05 days (30.0%) for step II (p<.001). Days of ICU stay in the control group were 1.14 days, step I was 1.05 days (p=.261), and step II was 1.12 days (p=.721). The ICU stay for step II was reduced by 0.02 days (1.8 %). The total cost per patient in step I was reduced by $738 (14.8%) (p<.001) and 2003~2005 years, step II marked an average annual increase of $310 (6.2%) (p=.022). The cost per day was increased by $69 (13.7%) for step I (p<.001) and by $264 (52.4%) for step II (p<.001) (Table 3).
In the application of CP in 197 patients in step I (75) and step II (122, only 2003 year), variations were observed in step I 1,425, step II 1,465 incidents. Details were as follows: step I incidents 150 (10.5%) and step II incidents 696 (47.5%) involved the patient or family due to patient's condition. step I incidents 1,275 (89.5%) and step II incidents 769 (52.5%) with the medical attendance as the result of a doctor's prescription. Classifying the variations by degree, step I incidents 1,425 (100%), step II incidents 1,464 (99.9%) fell into the grade 1 category, in which the application was slightly modified although the main content of CP remained, and 1 (0.1%) incident were classified as grade 3, in which CP application was not possible. Meanwhile, variations during the 2003~2009 period were observed in 12 items: observation/measurement 1, medication 8 and lab & test 3. Town's view was added. The medications changed were pre-operative main fluid, antacid, and coagulant. The schedule shortened was intake/output, post-operative main fluid, antibiotics, osmotic diuretics, steroid, discharge medication, and blood tests (ABGA, CBC and Serum & Urine electrolyte/Osmol.). Temporal bone CT schedule was changed (Table 4).
The average satisfaction rates for step I and step II (the year 2003) versus the control group increased slightly in all items, but not significantly so. One item from the questionnaire that did differ significantly was increased satisfaction with the guidance and information provided when patients were hospitalized in the ICU (p=.002). This increased satisfaction implies a reduction in patient anxiety and illustrates the importance of providing adequate information beforehand.
CPs have been defined as "systematically developed statements that assist practitioner and patient decision-making about appropriate health care in specific clinical circumstances". Some pressure is currently being exerted to develop guidelines by which the management of many medical and surgical conditions can be improved (Cheah, 2000; Mitchell et al., 2005; Park & Ro, 2000). We developed a CP for patients with HFS and TN who underwent MVD. The devised CP could alter clinical practices and improve patients' outcomes for this condition. Moreover, this application of CP reduced the incidence of complications, hospitalization duration, and patients' medical costs, and also improved patient satisfaction.
The principal complications were hearing loss and cranial nerve palsy. Previous reports demonstrated that hearing loss occurred in 0.3~4.8% of patients and that low cranial palsy occurred in 4% of patients (Acevedo, Sindou, Fischer, & Vial., 1997; Chung, Chang, Choi, Chang, & Park, 2001; Wang & Jankovic, 1998). The rate of hearing loss incidence was 1.8% in the control group. On the other hand, this rate was reduced in the application group (step I: 0%, step II: 0.5%). Similarly, the rate of low cranial nerve palsy occurrence decreased (control group: 1.8%, step I: 1.3%, step II: 0.7%). This decrease was attributed to the prompt response and continuous clinical intervention mandated by the systematic treatment plan at each stage, which was targeted toward the prevention of complications. The results of this study were consistent with a previous study (Ball & Peruzzi, 1997; Müller et al., 2009; Rotter et al., 2010).
In the CP application group, the hospital stay prior to surgery was reduced by step I 2.56 days, and step II 3.05 days. The total cost per patient in step I was reduced by 14.8%. The total cost per patient for step II marked an average annual increase of 6.2%. This was attributed to rising medical costs per person in Korea (9.3%) between the year 2000 and 2009 (Ministry of Health and Welfare, 2013). This suggested an increased profit rate of the hospital and confirmed the 1999 proposal of Rohrbach. The cost per day was increased by 13.7% (step I) and by 52.4% (step II). These results of this study were consistent with the results of a previous study (Rotter et al., 2010; Van Vliet et al., 2011; Oreja-Guevara et al., 2010; Panella, Marchisio, & Di Stanislao, 2003).
The number of operations per month was increased by 9.7 (210.0%) as compared to the year 2001, averaging 173.7 patients a year. This was attributed to the effects of education and public information including web and telephone counseling and the implementation of an effective management schedule. Moreover, it is anticipated that the performance of preliminary examinations and the management of hospitalization periods will increase the number of surgeries and improve bed-occupancy (Oreja-Guevara et al., 2010; Owen et al., 2006). Patients that undergo MVD have usually received other alternative treatment modalities including perennial treatment with Chinese medicine and ineffective physical therapy; often, these patients were originally incorrectly diagnosed or misadvised about their condition or the appropriate treatment method. Therefore, an accurate diagnosis and an active information system for this malady will be necessary. Thus, the maintenance of a website and the mailing of educational books will undoubtedly prove helpful in the creation of an information system for affiliated hospitals. Moreover, other ideas concerning information systems should also be taken into consideration (Van Vliet et al., 2011).
A total of 1,425 incidents of variations were observed among 75 patients. The severity and number of variations were insignificant relative to other proposals (Kim, 2010a, 2010b). Although an attempt was made to modify the CP based on the results of analysis of the variations, no items were modified. This was because the incidents (100.0%) were all first-degree variations, which did not affect the application of the CP. Meanwhile, variations during the period of 2003 to 2009 were observed in 12 items: observation/measurement 1, medication 8, and lab & test 3. This is a very important reason to develop CP (Cheah, 2000; Panella et al., 2003).
The value of the devised CP lies in the construction of a system based on teamwork by many health care professionals (Barbieri et al., 2009). By improving patients' education programs throughout stages of hospitalization (Owen et al., 2006; Van Vliet et al., 2011), nursing in the ICU and in general wards, and the management following discharge, the devised CP enhanced the cost-effectiveness of patient care (Kim, 2010b). The key factor underlying the success of this system was the collaborative relationship among health care professionals. However, it is by no means clear that all the positive results were attributable to the implementation of the pathway (Van Vliet et al., 2011). In fact, these results may have been attributable to the surgeon's experience. Further evaluation in this regard will be necessary, but CP has been instrumental in surgeons' experience, and has resulted in advances in the positive results of this study (Kim, 2010a). Specially, the current problem with the developed CP is not used (Lim, 2006). The advantage of this MVD CP was used with long time in practices. The significance of this paper is a long-term evaluation of eight years. This methodological study has established the effectiveness of CP.
In the future, quality improvement (QI) activity should be calibrated to ensure that continuous efforts are made to increase efficiency and teamwork, thus improving the quality of medical treatment and patient satisfaction level.
This study verified that the development and a long term application of the CP for MVD could significantly improve the quality of medical intervention and the efficiency of hospital management by standardizing the patient care system. In particular, the key component of the successful application of CP is the active participation of responsible doctors and CNS, and their teamwork. In fact, we proposed that the role of the CNS is critical in maximizing the effect of long term CP application. The following research courses are suggested in the future. Although CP has been regarded as an inappropriate for long term application due to variation, very promising results were obtained. Therefore, in order to apply CP for long term, the role of CNS is very important. Finally, the well organized and efficient system and multidisciplinary teamwork are required to implement the system successfully.
Figures and Tables
Figure 1
Critical pathway of microvascular decompression.
ABGA=Arterial blood gas analysis; A/C & D/B=Active cough & deep breathing; BST=Blood sugar test; CBC=Complete blood count; CT=Computed tomography; D/C=Discontinue; EKG=Electrocardiography; EMG=Electromyography; ENT=Ear, nose and throat; GCS=Glasgow coma scale; GW=General ward; HD=Hospital day; IAC MRI=Internal auditory canal MRI; ICU=Intensive care unit; I/O=Intake/output; iv=Intravenous; L/M=Limb movement; NCS=Nerve conduction study; NPO=Nil per os; N/S=Normal saline (Sodium chloride 0.9%); Op=Operation; opd=Outpatient department; P/S & L/R=Pupil size & Light reflex; PTA/SA=Pure tone audiometry/speech audiometry; SBP=Systolic blood pressure; SOW=Sips of water; SpO2=Pulse oximetry.

Table 4
Variation of Clinical Pathway of Microvascular Decompression (N=197)

A=Patient's condition; B=Decision of patient/family; C=doctor's prescription; #=Hospital day; ⓐ=Ampule; ABGA=Arterial blood gas analysis; CBC=Complete blood count; CT=Computed tomography; iv=Intravenous; KVO=Keep vein openm=minute; N/S=Normal saline (Sodium chloride 0.9%); OPD=Outpatient department; po=Per os; S/U electro & Osm=Serum/Urine electrolyte & Osmol; ⓣ=tablet.
References
1. Acevedo JC, Sindou M, Fischer C, Vial C. Microvascular decompression for the treatment of hemifacial spasm. Retrospective study of a consecutive series of 75 operated patients-electrophysiologic and anatomical surgicalanalysis. Stereotact Funct Neurosurg. 1997; 68:260–265. http://dx.doi.org/10.1159/000099936.
2. Ball C, Peruzzi M. Case management improves congestive heart failure outcomes. Nurs Case Manag. 1997; 2:68–74.
3. Barbieri A, Vanhaecht K, Van Herck P, Sermeus W, Faggiano F, Marchisio S, et al. Effects of clinical pathways in the joint replacement: A meta-analysis. BMC Med. 2009; 7:32. http://dx.doi.org/10.1186/1741-7015-7-32.
4. Beyea SC. Critical pathways for collaborative nursing care. New York: Addison-Wesley Publishing Company;1996.
5. Cheah J. Development and implementation of a clinical pathway programme in an acute care general hospital in Singapore. Int J Qual Health Care. 2000; 12:403–412. http://dx.doi.org/10.1093/intqhc/12.5.403.
6. Chung SS, Chang JH, Choi JY, Chang JW, Park YG. Microvascular decompression for hemifacial spasm: A long-term follow-up of 1,169 consecutive cases. Stereotact Funct Neurosurg. 2001; 77:190–193. http://dx.doi.org/10.1159/000064620.
7. Goto Y, Matsushima T, Natori Y, Inamura T, Tobimatsu S. Delayed effects of the microvascular decompression on hemifacial spasm: A retrospective study of 131 consecutive operated cases. Neurol Res. 2002; 24:296–300.
8. Isla-Guerrero A, Chamorro-Ramos L, Alvarez-Ruiz F, Aranda-Armengod B, Sarmiento-Martínez MA, Pérez-Alvarez M, et al. Design, implementation, and results of the clinical pathway for herniated lumbar disk. Neurocirugia (Astur). 2001; 12:409–418.
9. Ishikawa M, Nakanishi T, Takamiya Y, Namiki J. Delayed resolution of residual hemifacial spasm after microvascular decompression operations. Neurosurgery. 2001; 49:847–854.
10. Kim JS. Development of a critical pathway and its application for the management of subarachnoid hemorrhage. J Korean Data Anal Soc. 2010; 12(1):1–16.
11. Kim JS. Development of a critical pathway of barbiturate coma therapy in the management for severe brain damage. J Korean Acad Nurs Adm. 2010; 16:59–72. http://dx.doi.org/10.11111/jkana.2010.16.1.59.
12. Li ST, Pan Q, Liu N, Shen F, Liu Z, Guan Y. Trigeminal neuralgia: What are the important factors for good operative outcomes with microvascular decompression. Surg Neurol. 2004; 62:400–404.
13. Lim YJ, Jeong KI, Jeongm HY, Sun JJ, Kim YK, Choi JK, et al. Analysis of performance on activities in critical pathway of total hip replacement surgery. J Korean Acad Adult Nurs. 2006; 18:819–827.
14. Mauriello JA Jr, Dhillon S, Pakeman B, Mostafavi R, Yepez MC. Treatment choices of 119 patients with hemifacial spasm over 11 years. Clin Neurol Neurosurg. 1996; 98:213–216. http://dx.doi.org/10.1016/0303-8467(96)00025-X.
15. McLaughlin MR, Jannetta PJ, Clyde BL, Subach BR, Comey CH, Resnick DK. Microvascular decompression of cranial nerves: Lessons learned after 4400 operations. J Neurosurg. 1999; 90:1–8.
16. Ministry of Health & Welfare. Indicators of public health care at a glance. 2013. Retrieved November 21, 2013. from http://www.mw.go.kr/front_new/al/sal0301vw.jsp?PAR_MENU_ID=04&MENU_ID=0403&CONT_SEQ=293922&page=1.
17. Mitchell EA, Didsbury PB, Kruithof N, Robinson E, Milmine M, Barry M, et al. A randomized controlled trial of an asthma clinical pathway for children in general practice. Acta Paediatr. 2005; 94:226–233. http://dx.doi.org/10.1111/j.1651-2227.2005.tb01896.x.
18. Müller MK, Dedes KJ, Dindo D, Steiner S, et al. Impact of clinical pathways in surgery. Langenbecks Arch Surg. 2009; 394:31–39. http://dx.doi.org/10.1007/s00423-008-0352-0.
19. Mustafa MK, van Weerden TW, Mooij JJ. Hemifacial spasms caused by neurovascular compression. Ned Tijdschr Geneeskd. 2003; 147:273–277.
20. Oreja-Guevara C, Miralles A, Garcia-Caballero. J, Noval S, Gabaldon L, Esteban-Vasallo MD. Clinical pathways for the care of multiple sclerosis patients. Neurologia. 2010; 25:156–162. http://dx.doi.org/10.1016/S2173-5808(10)70031-6.
21. Owen JE, Walker RJ, Edgell L, Collie J, Douglas L, Hewitson TD. Implementation of a pre-dialysis clinical pathway for patients with chronic kidney disease. Int J Qual Health Care. 2006; 18:145–151. http://dx.doi.org/10.1093/intqhc/mzi094.
22. Panella M, Marchisio S, Di Stanislao F. Reducing clinical variations with clinical pathways: Do pathways work? Int J Qual Health Care. 2003; 15:509–521. http://dx.doi.org/10.1093/intqhc/mzg057.
23. Park HO, Ro YJ. Development of case management using critical pathway of posterolateral fusion for lumbar spinal stenosis. J Korean Acad Adult Nurs. 2000; 12:727–740.
24. Romagnuolo J, Flemons WW, Perkins L, Lutz L, Jamieson PC, Hiscock CA, et al. Post-endoscopy checklist reduces length of stay for non-variceal upper gastrointestinal bleeding. Int J Qual Health Care. 2005; 17:249–254. http://dx.doi.org/10.1093/intqhc/mzi023.
25. Samii M, Gunther T, Iaconetta G, Muehling M, Vorkapic P, Samii A. Microvascular decompression to treat hemifacial spasm: Long-term results for a consecutive series of 143 patients. Neurosurgery. 2002; 50:712–718.
26. Van Vliet EJ, Bredenhoff E, Sermeus W, Kop LM, Sol JC, Van Harten WH. Exploring the relation between process design and efficiency in high-volume cataract pathways from a lean thinking perspective. Int J Qual Health Care. 2011; 23:83–93. http://dx.doi.org/10.1093/intqhc/mzq071.
27. Wang A, Jankovic J. Hemifacial spasm: Clinical findings and treatment. Muscle Nerve. 1998; 21:1740–1747. http://dx.doi.org/10.1002/(SICI)1097-4598(199812)21:12<1740::AID-MUS17>3.0.CO;2-V.
28. Yeats M, Wedergren S, Fox N, Thompson JS. The use and modification of clinical pathways to achieve specific outcomes in bariatric surgery. Am Surg. 2005; 71:152–154.
29. Zhang AH, Liu XH. Clinical pathways: Effects on professional practice, patient outcomes, length of stay and hospital costs. Int J Evid Based Healthc. 2011; 9:191–192. http://dx.doi.org/10.1002/14651858.CD006632.pub2.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download