Abstract
BACKGROUND/OBJECTIVES
Lactobacillus brevis G101 suppresses the absorption of monosodium glutamate (MSG) from the intestine into the blood in mice. Therefore, the attenuating effect of orally administered G101 on monosodium glutamate (MSG) symptom complex was investigated in humans.
MATERIALS/METHODS
Capsules (300 mg) containing Lactobacillus brevis G101 (1×1010 CFU/individual) or maltodextrin (placebo) was orally administered in 30 respondents with self-recognized monosodium glutamate (MSG) symptom complex for 5 days and the rice with black soybean sauce containing 6 g MSG (RBSM) was ingested 30 min after the final administration. Thereafter, the MSG symptom complex (rated on a 5-point scale: 1, none; 5, strong) was investigated in a double blind placebo controlled study. The intensity of the MSG symptom complex was significantly reduced in respondents of the G101 intake group (2.87 ± 0.73) compared to that in those treated with the placebo (3.63 ± 1.03) (P = 0.0016). Respondents in the placebo group exhibited more of the various major conditions of the MSG symptom complex than in the G101 intake group. Although there was no significant difference in the appearance time of the MSG symptom complex between subjects orally administered G101 and those administered the placebo, its disappearance in < 3 h was observed in 69.9% of subjects in the G101 treatment group and in 38.0% of subjects in the placebo group (P = 0.0841).
Monosodium glutamate (MSG), the sodium salt of glutamate, is used worldwide as a flavor enhancer in various processed foods [123]. MSG was extracted from seafood and has been as the source of the umami taste [4]. The Food and Drug Administration (FDA) has classified MSG as a generally recognized as safe (GRAS) substance and no limitation is placed on its use as a food additive. Nevertheless, Kwok first described a complex of symptoms, including numbness at the back of the neck and arms, weakness, and palpitation, after ingestion of a Chinese meal and suggested that MSG was one of the possible causes [5]. These symptoms were referred to collectively as Chinese Restaurant Syndrome (CRS). In 1995, the Federation of American Societies for Experimental Biology (FASEB) proposed the term MSG symptom complex to denote the reactions that occur following ingestion of MSG [6]. When > 5 g may be ingested, it is characterized by unpleasant reactions such as numbness, tingling, headaches, muscle tightness, general weakness, and flushing [7].
Lactic acid bacteria are found in yogurt, cheese, kimchi, and in the gut microbiota [8]. Upon ingestion, lactic acid bacteria confer beneficial effects on the health of the host [9]. Of these lactic acid bacteria, some convert MSG to gamma-aminobutyric acid (GABA), which has been reported to possess various physiological functions that act via the decarboxylation of glutamic acid by glutamate decarboxylase [1011]. Therefore, lactic acid bacteria have been used as initiators to produce GABA-rich foods [12]. We previously isolated Lactobacillus brevis G-101, a kimchi-derived lactic acid bacterium that potently converted MSG to GABA [13]. Lactobacillus brevis G101 reduces the concentration of MSG in the blood of mice fed oral administration in mice: G101 suppresses the absorption of MSG from the intestine into the blood rather than mediating the biotransformation of MSG to GABA [14].
In the present study, to investigate the ability of orally administered Lactobacillus brevis G101 to attenuate the MSG symptom complex, we orally administered G101 or a placebo (maltodextrin) to respondents presenting with self-recognized MSG symptom complex, following ingestion of rice with black soybean sauce (Jajangbap) containing 6 g MSG (RBSM), and then investigated the intensity of the MSG complex in them. This experiment was performed as a double-blind, placebo-controlled study.
The study subjects consisted of 30 healthy Korean individuals (average age, 23.57 ± 2.36 yrs; 10 male subjects, 23.00 ± 3.46 yrs; 20 female subjects, 23.85 ± 1.60 yrs) who self-identified as MSG-sensitive. Exclusion criteria included consumption of any current medication. The recruitment of subjects was approved by the Committee for the Care and Use of Clinical Study at Kyung Hee University (KHSIRB-14-004) and performed according to CONSORT 2010 guidelines.
All 30 subjects participated in an orientation session for this study. The subjects were evenly divided into 2 groups (A and B). In the first week, group A subjects were orally administered one capsule (Lactobacillus brevis G101) at 11:00 am for 5 days and group B subjects took the placebo capsule every day (Table 1). RBSM was ingested 30 min after the final administration of G101, and the intensity and variety of the MSG symptom complex over 6 h were described. In the second week, group A switched with group B and the test was performed for 5 days. The intensity of the MSG symptom complex was rated according to a 5-point scale (1 = none, 5 = strong).
Capsules (300 mg) containing 1 × 1010 CFU Lactobacillus brevis G101 or maltodextrin (placebo) were prepared by CTCBIO Inc. RBSM was prepared by mixing steamed rice (180 g) and MSG-contained black soybean sauce. The ingredients of the MSG-contained black soybean sauce (one serving) were as follows: 40 g pork, 40 g onion, 40 g zucchini, 30 g carrot, 50 g cabbage, 1 Tsp black soybean sauce without MSG, 1/2 Tsp soybean oil, 6 g MSG, 1 tsp starch, and 1 2/3 Tsp water. MSG was purchased from a local market.
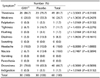
To evaluate the attenuating effect of Lactobacillus brevis G101 against the MSG symptom complex, we orally administered G101 to volunteers who then ingested RBSM, and after which we evaluated the MSG symptom complex for 6 h in a double-blind, placebo-controlled study (Table 2). The intensity of MSG symptom complex was measured using a 5-point scale (1 = none, 5 = strong). Oral administration of G101 significantly attenuated the intensity of the MSG symptom complex (P = 0.0016). When treated with the placebo, 43.3% of respondents presented with more than a slightly strong MSG symptom complex, but when treated with G101, only 20.0% of respondents exhibited more than a slightly strong response. A significant difference was observed among female subjects, but not among male subjects, indicating that female respondents were more sensitive to the MSG symptom complex than male (Table 3).
The effects of orally administered G101 on RBSM-induced self-recognized MSG symptoms (variety) experienced by the respondents were investigated (Table 4). After ingestion of RBSM, the most frequently observed self-recognized symptoms associated with the MSG symptom complex were thirstiness (81.7%) and drowsiness (70.0%), followed by weakness (26.7%), tightness (11.7%), headache (10.0%), nausea (10.0%), dizziness (8.3%), palpitation (1.7%), flushing (1.7%), and indigestion (1.7%). No significant difference was observed between the varieties of self-recognized symptoms experienced by respondents who were orally administered G101 and those administered the placebo.
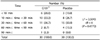
The effect of orally administered G101 on the time at which the RBSM-induced MSG symptom complex appeared was also evaluated (Table 5). There was no significant difference in the appearance time of the MSG symptom complex observed between subjects orally administered G101 and those administered the placebo. When subjects were treated with G101, the appearance for the MSG symptoms complex was less than 1 h for 70.0% of the respondents in the group, and in subjects treated with the placebo, the appearance time was for 76.6% of the group.
Next, we investigated the effect of orally administered G101 on the disappearance time for the RBSM-induced MSG symptoms complex (Table 6). There was no significant difference in the appearance time for the MSG symptom complex between subjects orally administered G101 and those administered the placebo. Disappearance of the MSG symptom complex in less than 3 h was observed in 69.9% of subjects in the G101 treatment group and in 38.0% of subjects in the placebo group (P = 0.0841).
MSG is frequently used in various canned foods and in food from Chinese restaurant. MSG has been associated with various side effects, including numbness, headaches, migraines, palpitations, tightness, weakness, aching, flushing, sweating, fasciculation, lacrimation, syncope, dizziness, shudder attacks, paresthesia, arrhythmia and tachycardia [1]. Although the oral threshold range for minimal MSG-induced symptoms in humans is considerably variable, in the previous study, the oral threshold range for minimal MSG-induced symptoms in 36 subjects was found to be 1.5 to 12 g, and increased intensity of the MSG symptom response was related to an increase in the oral dose [15]. In this study, we found that oral administration of RBSM, which is containing 6 g of MSG, showed various side effects including thirstiness (56.7%), drowsiness (23.3%), weakness (6.7%), indigestion (6.7%), headache (3.3%), and nausea (3.3%). It was previously shown that the elimination of all food sources containing MSG resulted in a decreased frequency of headaches [3]. These results suggest that the side effects of MSG are dependent on the daily intake amount of MSG, and the oral intake of more than 6 g of MSG may cause its side effect. Therefore, Xiong et al. suggested possible ways to reduce the side effects of MSG, such as taking vitamin C or pre-exposure to a low dose of MSG that may either prevent or reduce the side effects of MSG [3]. Nevertheless, it is not sufficient to reduce only the side effects of MSG. Therefore, we investigated the ability of Lactobacillus brevis G101 to reduce the side effects of MSG. Oral administration of Lactobacillus brevis G101 significantly attenuated the MSG symptom complex. Although G101 did not reduce the variety of side effects, it shortened the disappearance time of the MSG symptom complex.
In conclusion, this study suggests that orally administration of Lactobacillus brevis G101 may be able to reduce the intensity of the MSG symptom complex and shorten its disappearance time.
Figures and Tables
Table 1
Experimental plan for the effect of oral administered Lactobacillus brevis G101 on the MSG symptom complex in a double-blind, placebo-controlled study
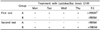
Table 2
The effect of orally administered Lactobacillus brevis G 101 on the intensity of RBSM-induced MSG symptom complex
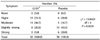
Table 3
The difference on the efficacy of Lactobacillus brevis G101 on the MSG symptom complex by gender

Table 4
The effect of orally administered Lactobacillus brevis G101 on RBSS-induced MSG symptom variety
References
1. Geha RS, Beiser A, Ren C, Patterson R, Greenberger PA, Grammer LC, Ditto AM, Harris KE, Shaughnessy MA, Yarnold PR, Corren J, Saxon A. Review of alleged reaction to monosodium glutamate and outcome of a multicenter double-blind placebo-controlled study. J Nutr. 2000; 130:1058S–1062S.

2. Yaqub H, Abdel Baky NA, Attia HA, Faggah LM. Hepatoprotective effect of N-acetyl cysteine and/or beta-carotene on monosodium glutamate-induced toxicity in rats. Res J Med Med Sci. 2008; 3:206–215.
3. Xiong JS, Branigan D, Li M. Deciphering the MSG controversy. Int J Clin Exp Med. 2009; 2:329–336.
4. Bellisle F. Glutamate and the UMAMI taste: sensory, metabolic, nutritional and behavioural considerations. A review of the literature published in the last 10 years. Neurosci Biobehav Rev. 1999; 23:423–438.

7. Yang WH, Drouin MA, Herbert M, Mao Y, Karsh J. The monosodium glutamate symptom complex: assessment in a double-blind, placebo-controlled, randomized study. J Allergy Clin Immunol. 1997; 99:757–762.

8. Kanmani P, Satish Kumar R, Yuvaraj N, Paari KA, Pattukumar V, Arul V. Probiotics and its functionally valuable products-a review. Crit Rev Food Sci Nutr. 2013; 53:641–658.

9. Gomes AM, Malcata FX. Bifidobacterium spp. and Lactobacillus acidophilus: biological, biochemical, technological and therapeutical properties relevant for use as probiotics. Trends Food Sci Technol. 1999; 10:139–157.

10. Cho YR, Chang JY, Chang HC. Production of gamma-aminobutyric acid (GABA) by Lactobacillus buchneri isolated from kimchi and its neuroprotective effect on neuronal cells. J Microbiol Biotechnol. 2007; 17:104–109.
11. Tamura T, Noda M, Ozaki M, Maruyama M, Matoba Y, Kumagai T, Sugiyama M. Establishment of an efficient fermentation system of gamma-aminobutyric acid by a lactic acid bacterium, Enterococcus avium G-15, isolated from carrot leaves. Biol Pharm Bull. 2010; 33:1673–1679.

12. Cherubini E, Gaiarsa JL, Ben-Ari Y. GABA: an excitatory transmitter in early postnatal life. Trends Neurosci. 1991; 14:515–519.

13. Jang SE, Han MJ, Kim SY, Kim DH. Lactobacillus brevis G101 inhibits the absorption of monosodium glutamate in mice. J Microbiol Biotechnol. 2014; 24:1592–1596.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download