1. Lindström J, Peltonen M, Eriksson JG, Ilanne-Parikka P, Aunola S, Keinänen-Kiukaanniemi S, Uusitupa M, Tuomilehto J. Finnish Diabetes Prevention Study (DPS). Improved lifestyle and decreased diabetes risk over 13 years: long-term follow-up of the randomised Finnish Diabetes Prevention Study (DPS). Diabetologia. 2013; 56:284–293.

2. Krishnan S, Rosenberg L, Singer M, Hu FB, Djoussé L, Cupples LA, Palmer JR. Glycemic index, glycemic load, and cereal fiber intake and risk of type 2 diabetes in US black women. Arch Intern Med. 2007; 167:2304–2309.

3. Pedicino D, Liuzzo G, Trotta F, Giglio AF, Giubilato S, Martini F, Zaccardi F, Scavone G, Previtero M, Massaro G, Cialdella P, Cardillo MT, Pitocco D, Ghirlanda G, Crea F. Adaptive immunity, inflammation, and cardiovascular complications in type 1 and type 2 diabetes mellitus. J Diabetes Res. 2013; 2013:184258.

4. American Diabetes Association. Economic costs of diabetes in the U.S. in 2012. Diabetes Care. 2013; 36:1033–1046.
5. Snel M, Jonker JT, Hammer S, Kerpershoek G, Lamb HJ, Meinders AE, Pijl H, de Roos A, Romijn JA, Smit JW, Jazet IM. Long-term beneficial effect of a 16-week very low calorie diet on pericardial fat in obese type 2 diabetes mellitus patients. Obesity (Silver Spring). 2012; 20:1572–1576.

6. Boden G, Sargrad K, Homko C, Mozzoli M, Stein TP. Effect of a low-carbohydrate diet on appetite, blood glucose levels, and insulin resistance in obese patients with type 2 diabetes. Ann Intern Med. 2005; 142:403–411.

7. Nielsen JV, Joensson EA. Low-carbohydrate diet in type 2 diabetes: stable improvement of bodyweight and glycemic control during 44 months follow-up. Nutr Metab (Lond). 2008; 5:14.

8. Grinvalsky M, Nathan DM. Diets for insulin pump and multiple daily injection therapy. Diabetes Care. 1983; 6:241–244.

9. Pan XR, Li GW, Hu YH, Wang JX, Yang WY, An ZX, Hu ZX, Lin J, Xiao JZ, Cao HB, Liu PA, Jiang XG, Jiang YY, Wang JP, Zheng H, Zhang H, Bennett PH, Howard BV. Effects of diet and exercise in preventing NIDDM in people with impaired glucose tolerance. The Da Qing IGT and Diabetes Study. Diabetes Care. 1997; 20:537–544.

10. Houlihan CA, Allen TJ, Baxter AL, Panangiotopoulos S, Casley DJ, Cooper ME, Jerums G. A low-sodium diet potentiates the effects of losartan in type 2 diabetes. Diabetes Care. 2002; 25:663–671.

11. Heilbronn LK, Noakes M, Clifton PM. Effect of energy restriction, weight loss, and diet composition on plasma lipids and glucose in patients with type 2 diabetes. Diabetes Care. 1999; 22:889–895.

12. Hemmingsen B, Lund SS, Gluud C, Vaag A, Almdal T, Hemmingsen C, Wetterslev J. Intensive glycaemic control for patients with type 2 diabetes: systematic review with meta-analysis and trial sequential analysis of randomised clinical trials. BMJ. 2011; 343:d6898.

13. ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, Cutler JA, Simons-Morton DG, Basile JN, Corson MA, Probstfield JL, Katz L, Peterson KA, Friedewald WT, Buse JB, Bigger JT, Gerstein HC, Ismail-Beigi F. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362:1575–1585.

14. Zoppini G, Negri C, Stoico V, Casati S, Pichiri I, Bonora E. Triglyceride-high-density lipoprotein cholesterol is associated with microvascular complications in type 2 diabetes mellitus. Metabolism. 2012; 61:22–29.

15. Nagy A, Adany R, Sandor J. Effect of diagnosis-time and initial treatment on the onset of type 2 diabetes mellitus complications: a population-based representative cross-sectional study in Hungary. Diabetes Res Clin Pract. 2011; 94:e65–e67.

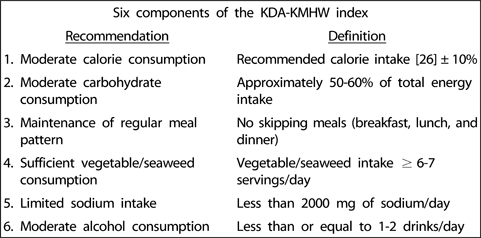
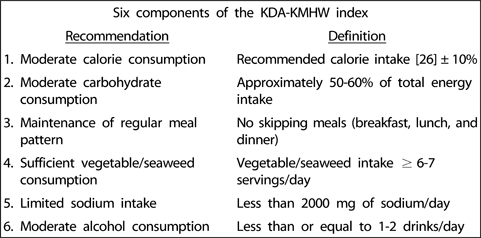
16. Korean Diabetes Association. Treatment Guideline for Diabetes. 1st ed. Seoul: Korean Diabetes Association;1990.
17. Korean Diabetes Association. Treatment Guideline for Diabetes. 2nd ed. Seoul: Korean Diabetes Association;1995.
18. Korean Diabetes Association. Treatment Guideline for Diabetes. 3rd ed. Seoul: Korean Diabetes Association;2007.
19. Korean Diabetes Association. Treatment Guideline for Diabetes. 4th ed. Seoul: Korean Diabetes Association;2011.
20. Ministry of Health & Welfare (KR). Dietary Guidelines for Disease Management. Seoul: Ministry of Health & Welfare;2010.
21. Lim JH, Paik HY, Lee YS, Song Y. Adherence to lifestyle recommendations is associated with improved glycemic control and improved blood lipid levels in Korean adults with type 2 diabetes. Diabetes Res Clin Pract. 2013; 101:e21–e24.

22. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, Chun C, Khang YH, Oh K. Data resource profile: The korea national health and nutrition examination survey (knhanes). Int J Epidemiol. 2014; 43:69–77.

23. American Diabetes Association. Standards of medical care in diabetes--2012. Diabetes Care. 2012; 35:Suppl 1. S11–S63.
24. World Health Organization Western Pacific Region (PH). International Association for the Study of Obesity (GB). International Obesity Task Force (GB). The Asia-Pacific Perspective: Redefining Obesity and Its Treatment. Balmain: Health Communications Australia;2000.
25. Korean Nutrition Society. Dietary Reference Intakes for Koreans. 1st rev. ed. Seoul: Korean Nutrition Society;2010.
27. Rivellese AA, Boemi M, Cavalot F, Costagliola L, De Feo P, Miccoli R, Patti L, Trovati M, Vaccaro O. Mind.it Study Group. Dietary habits in type II diabetes mellitus: how is adherence to dietary recommendations? Eur J Clin Nutr. 2008; 62:660–664.

28. Santos FL, Esteves SS, da Costa Pereira A, Yancy WS Jr, Nunes JP. Systematic review and meta-analysis of clinical trials of the effects of low carbohydrate diets on cardiovascular risk factors. Obes Rev. 2012; 13:1048–1066.

29. Kirk JK, Graves DE, Craven TE, Lipkin EW, Austin M, Margolis KL. Restricted-carbohydrate diets in patients with type 2 diabetes: a meta-analysis. J Am Diet Assoc. 2008; 108:91–100.

30. Kim S, Moon S, Popkin BM. The nutrition transition in South Korea. Am J Clin Nutr. 2000; 71:44–53.

31. Park SH, Lee KS, Park HY. Dietary carbohydrate intake is associated with cardiovascular disease risk in Korean: analysis of the third Korea National Health and Nutrition Examination Survey (KNHANES III). Int J Cardiol. 2010; 139:234–240.

32. Lee H, Kim M, Daly BJ. Nutritional patterns of Korean diabetic patients: an exploratory study. Int Nurs Rev. 2008; 55:442–446.

33. Ahn HJ, Koo BK, Jung JY, Kwon HR, Chung MY, Ku YH, Kim JT, Han KA, Min KW. Association between volume of bowls and the dietary intakes in subjects with type 2 diabetes. Korean Diabetes J. 2009; 33:335–343.

34. Moon SJ. Rice in the Korean diet: a value system. DACO Industrial Research Institute Symposium on manufacturing techniques of traditional food utilizing rice. Seoul: DACO Industrial Research Institute;1993.
35. Elliott P, Stamler J, Nichols R, Dyer AR, Stamler R, Kesteloot H, Marmot M. Intersalt revisited: further analyses of 24 hour sodium excretion and blood pressure within and across populations. Intersalt Cooperative Research Group. BMJ. 1996; 312:1249–1253.

36. Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet. 2005; 365:217–223.

37. Cohen HW, Hailpern SM, Alderman MH. Sodium intake and mortality follow-up in the third national health and nutrition examination survey (nhanes iii). J Gen Intern Med. 2008; 23:1297–1302.

38. Ekinci EI, Clarke S, Thomas MC, Moran JL, Cheong K, MacIsaac RJ, Jerums G. Dietary salt intake and mortality in patients with type 2 diabetes. Diabetes Care. 2011; 34:703–709.

39. Maillot M, Drewnowski A. A conflict between nutritionally adequate diets and meeting the 2010 dietary guidelines for sodium. Am J Prev Med. 2012; 42:174–179.

40. Solomon CG, Hu FB, Stampfer MJ, Colditz GA, Speizer FE, Rimm EB, Willett WC, Manson JE. Moderate alcohol consumption and risk of coronary heart disease among women with type 2 diabetes mellitus. Circulation. 2000; 102:494–499.

41. Sluik D, Boeing H, Bergmann MM, Schütze M, Teucher B, Kaaks R, Tjønneland A, Overvad K, Arriola L, Ardanaz E, Bendinelli B, Agnoli C, Tumino R, Ricceri F, Mattiello A, Spijkerman AM, Beulens JW, Grobbee DE, Nilsson PM, Melander O, Franks PW, Rolandsson O, Riboli E, Gallo V, Romaguera D, Nöthlings U. Alcohol consumption and mortality in individuals with diabetes mellitus. Br J Nutr. 2012; 108:1307–1315.

42. Ahrén B. Avoiding hypoglycemia: a key to success for glucose-lowering therapy in type 2 diabetes. Vasc Health Risk Manag. 2013; 9:155–163.
43. Kim JH, Kim SJ, Lee WY, Cheon YH, Lee SS, Ju A, K M, Kim DJ. The effects of alcohol abstinence on BDNF, ghrelin, and leptin secretions in alcohol-dependent patients with glucose intolerance. Alcohol Clin Exp Res. 2013; 37:Suppl 1. E52–E58.

44. Kahn SE. "The relative contributions of insulin resistance and beta-cell dysfunction to the pathophysiology of Type 2 diabetes", by Kahn SE. Diabetologia. 2003; 46:3–19.

45. Kim TH, Chun KH, Kim HJ, Han SJ, Kim DJ, Kwak J, Kim YS, Woo JT, Park Y, Nam M, Baik SH, Ahn KJ, Lee KW. Direct medical costs for patients with type 2 diabetes and related complications: a prospective cohort study based on the Korean National Diabetes Program. J Korean Med Sci. 2012; 27:876–882.

46. Navarro-Vidal B, Banegas JR, León-Muñoz LM, Rodríguez-Artalejo F, Graciani A. Achievement of cardiometabolic goals among diabetic patients in Spain. A nationwide population-based study. PLoS One. 2013; 8:e61549.

47. Harris MI, Eastman RC. Early detection of undiagnosed diabetes mellitus: a US perspective. Diabetes Metab Res Rev. 2000; 16:230–236.

48. Lee J, Smith JP. The effect of health promotion on diagnosis and management of diabetes. J Epidemiol Community Health. 2012; 66:366–371.

49. Choi YJ, Kim HC, Kim HM, Park SW, Kim J, Kim DJ. Prevalence and management of diabetes in korean adults: Korea national health and nutrition examination surveys 1998-2005. Diabetes Care. 2009; 32:2016–2020.