Abstract
BACKGROUND/OBJECTIVES
Women's bone health status is closely related with environmental factors and lifestyle factors. The purpose of this study is to evaluate the dietary risks of osteoporosis and osteopenia for Korean postmenopausal women.
SUBJECTS/METHODS
The data from 1,433 subjects from the 2010 KNHANES were used and divided into three groups: normal, osteopenia, and osteoporosis group using bone mineral density (BMD). Nutrient intakes and food intake frequency were evaluated. Logistic regression analysis was applied to determine the odds ratios for osteoporosis and osteopenia.
RESULTS
The RNI percentage of each nutrient and food intake frequency from 12 food groups decreased as bone mineral density status deteriorated. Risk for osteoporosis of low calcium (Ca) intake, under the EAR, showed an odds ratio of 2.13(95% CI; 1.26-3.61, P < 0.05). Higher intake frequency showed preventive effect from osteoporosis compared to lower intake frequency in such food group as dairy products (ORs 0.40, CI 0.21-0.75), beans (ORs 0.49, CI 0.29-0.83), seaweeds (ORs 0.55, CI 0.32-0.94), fish (ORs 0.56, CI 0.32-0.98), and fruits (ORs 0.42, CI 0.23-0.79) after adjusting for age.
Korea is expected to transit into an aged society by 2020 and the life expectancy of Korean women is consistently increasing every year. Accordingly the number of postmenopausal women is increasing rapidly. According to the findings [1,2,3] regarding the average age of Korean women with menopause, more than one-third of the entire Korean women lie in the period of postmenopause. The increase in the population of elderly women and their lengthened lives also increase the burden of their disease treatment and rehabilitation, deteriorating the national budget burden.
Osteoporosis is a metabolic disease increasing fracture risks in the femoral neck, lumbar spine, and total femur due to changes in concrete bone structure leading to bone strength and homogeneity. With the decrement in estrogen excretion during menopause, osteoporosis has become a disease of bone resorption whose prevalence rate is higher in women than in men [1,2,3]. Osteoporosis is a global health problem with the accelerating growth of the elderly population, and its prevalence rate has been consistently increasing since 1998 according to the National Statistical Office Statistics [4]. Since decrease in bone mass, which is a representative symptom of metabolic bone disease, progresses silently, most of the patients fail to recognize any symptoms until they experience bone fracture when they cannot receive effective treatment and end up enduring economic loss, physical disability, and decreased quality of life [5]. Osteoporosis is recognized as a representative disease of elderly women [6].
It is believed that, among genetic factors, estrogen is the most affective conjunction with environmental factors such as physical activity, medicine, smoking, being underweight, ovariotomy, alcohol drinking, nutrition, etc. [7].
Trigliceride, total cholesterol, LDL cholesterol, and Follicle-stimulating hormone (FSH) are negatively correlated with bone density [8] and age especially in females [8], while income levels and housing types are closely related to bone mineral density status [8]. As the number of family members is also related with bone mineral density status, postmenopausal women living alone are highly vulnerable and double burdened with relatively lower income and balanced diet for the lack of attention paid to cooking preparation [9].
Lower education level is also negatively related with bone mineral density status due to lower chance of exposure to information regarding prevention of osteoporosis [10]. As for anthropometric factors, higher BMI showed lower risk of the disease. Higher body weight tends to decrease the risk of the disease as increased body weight tends to give more tension to body, leading to some protective effect [11,12]. These phenomena can be explained by an increase in body weight with physical stress, vitamin D and estrogen synthesis in the subcutaneous fat mass [13], and the storage place of 25(OH) Vitamin D3 [13,14]. Underweight women show higher risk compared to overweight women due to lower estrogen production and lower estrogen concentration in the blood [13]. As the lengthening of menopause duration deteriorates the bone's health status and increases the risks of related diseases, it is necessary for the spread and impact of osteoporosis to be assessed consistently in many aspects [8].
It is important to analyze the relationship between dietary aspects and bone health risks with considerations of sociodemographic, anthropometric, and biochemical factors in order to manage the disease based on those findings. Despite many studies that evaluate dietary factors based on relatively small convenient samples, such nationwide studies which assess risk factors and estimate the possible disease impacts for the subjects of post-menopausal women as this have been lacking. Developing the systematic osteoporosis prevention programs for the vulnerable groups whose dietary practices are unhealthy, especially the low-income elderly, is required in order to ease the burden of national medical expense.
This study, using the 2010 Korean National Health and Nutrition Examination Survey Data, aims to identify the dietary practices related to osteoporosis risk by dividing the subjects into three groups based on bone health status, and provides baseline data for the prevention of osteoporosis.
This study uses the 2010 Korea National Health and Nutrition Examination Survey Data. First, 1,579 postmenopausal females were selected by excluding male or premenopausal women from a total of 8,953 subjects of the KNHANES. Among the 1,579 subjects, 146 women who recently changed their dietary intakes under the advice of doctors were dropped, leading to the 1,433 subjects whose data were collected and analyzed.
The final data set of the 1,433 participants, who completed the health examination, was divided into three groups: normal, osteopenia, and osteoporosis according to their bone health status. The T-score was calculated using the following formula:
The 213 participants with T-score ≥ -1.0 were grouped as normal, 722 participants with -2.5 < T-score < -1.0 were put in the osteopenia, and the remaining 495 participants with T-score ≤ -2.5 were categorized as having osteoporosis following the WHO criteria [14].
The weight and height measurement data from the participants were collected and the BMI (Body Mass Index) values were calculated using the following formula:
Obese and overweight subjects were defined as those with BMI ≥ 25.0, and low weight was defined as those with BMI < 18.5 based on the WHO Standard Definition for Obesity.
Data of socio-demographic characteristics of the subjects were collected using a structured questionnaire of the KNHANES, carried out by individual interviews and self-administered answering. The items surveyed using the questionnaire included family size, house type, attained education level, employment status, monthly disposable income, age, gender, etc.
Income was categorized into three levels after adjusting the value classified according to the average monthly household income equalization such as gender and age.
The KNHANES diet survey is composed of food frequency intake data and one-day food intake data collected using the 24-hr dietary recall method. A 24-hr dietary recall investigated the contents of the food intake survey the day before the survey was investigated from January to December as a regular investigation.
The average amount of a certain nutrient intake was calculated and compared with the KDRI [24]. All of the dietary data were collected by pre-trained professionals by individual interview method. Food frequency intake data were collected using a structured food frequency questionnaire, which included 11 food groups, totaling 63 foods composed of 7 grains, 5 beans, 6 meats and eggs, 9 fish, 12 vegetables, 2 seaweeds, 11 fruits, 3 milk and milk products, 3 beverages, 3 alcoholic drinks, and others. Intake frequencies were divided into 10 intervals. All of the intake frequencies were converted into average weekly consumption and compared.
Using calculating coefficient was converting; the coefficient value was 0 (rarely eating), 0.16 (6-11/year), 0.23 (2-3/month), 0.58 (2-3/month), 1 (1/week), 2.5 (2-3/week), 5(4-6/week), 7 (1/day), 14 (2/day) and 21 (3/day), respectively; the resulting figures from each of the three groups of the bone mineral density status were compared and analyzed. The intake frequencies of each food group were divided into tertile and intake frequency of Q2, while Q3 was compared to Q1 after adjusting for age.
All the analyses were conducted using a survey weighting to account for a complex survey design. The SPSS 18.0 statistics package (ver. 18.0, SPSS Inc., Chicago, USA) was used for the data analysis. Descriptive statistics such as nominal variables, frequency, and proportion were calculated, while the Chi-square test was carried out to examine the association between categorical variables using a significance level of P < 0.05.
For continuous variables, the average and standard error were calculated and one-way-ANOVA test or Logistic regression analysis was applied by controlling age, body mass index, and hormone supplement intake to examine the difference or odds ratio among those three bone health groups.
The socio-demographic characteristics of the study participants grouped by bone mineral density status are reported in Table 1. The proportion of those with osteoporosis among women under 59 was 13.5%, 33.3% among those 60-69 years, and 64.9% among those 70 years and above (P < 0.001), showing increase with age. On the contrary, the proportion of those grouped "normal" was 29.4% among those 59 years and under, 8.3% among those in their sixties, and 3.2% among those 70 and above (P < 0.001).
As for attained education level, subjects were categorized into four groups according to the Korean education system. The bone health status of Korean postmenopausal women showed a strong association with education level; the more educated they were, the stronger the bone they had. Among elementary school graduates, the prevalence rate of osteoporosis was highest at 45.8%, while the college graduates registered lowest at 11.8% On the other hand, the proportion of those with normal bone mineral density was highest at 32.4% among college graduates and lowest at 8.9% among elementary school graduates (P < 0.001).
As for occupation, compared to housewives or simple labor workers such as farmers and fishermen whose socio-economic statuses are relatively low, office workers or those in the service sector showed better bone mineral density status. This result is also derived among those living in dual income households, as their higher economic status allows for higher chance of practicing physical activity or obtaining nutritional information (P < 0.001).
As for a household's monthly income, in case of below 1,000,000 won, the distribution of subjects was 8.5% (n = 44) in the normal group of bone mineral density status, 44.2% (n = 228) in the osteopenia group, and 47.3% (n = 244) in the osteoporosis group. Between 1,000,000 and 2,000,000 won, the distribution of subjects was 16% (n = 98) in the normal group of bone mineral density status, 54.3% (n = 333) in the osteopenia group, and 29.7% (n = 182) in osteoporosis group; over 2,000,000 won, the distribution of subjects was 25% (n = 71) in the normal group of bone mineral density status, 52.8% (n = 150), in the osteopenia group, and 22.2% (n = 63) in the osteoporosis group.
A household's monthly income showed association with bone mineral density status. The prevalence rates of osteoporosis were higher among those of relatively lower economic status or those who were unemployed.
The number of family members showed association with bone mineral density status. The prevalence rates of osteoporosis were higher among those with a relatively lower number of family members. The reason perhaps was diversity in food choice and food intake.
Participants' anthropometric characteristics are reported in Table 2. The ANOVA test showed significant differences in average height and weight, waist circumference, and BMI value among the three groups. Average weight, waist circumference, and BMI value also increased as bone mineral density status were improved. All of the anthropometric characteristics showed the same trend: bone mineral density status improved as the average anthropometric measurements increased, in the order of the osteoporosis group, the osteopenia group, and the normal group (P < 0.001). The average height was 156.1 ± 0.4 cm in the normal group, 154 ± 0.2 cm in the osteopenia group, and 150.3 ± 0.3 cm in the osteoporosis group. As for weight, the normal group was 62.0 ± 0.5 kg, the osteopenia group was 57.9 ± 0.3 kg, and the osteoporosis group was 53.1 ± 0.4 kg (P < 0.001). As for the waist circumference, the normal bone health group was 83.9 ± 0.6 cm, the osteopenia group was 82.6 ± 0.3 cm, and the osteoporosis group was 81.3 ± 0.4 cm. The prevalence rate of osteoporosis was 63.9% among the underweight group but it decreased to 38.9% among the normal weight group and 25.8% among the obesity group (P < 0.001).
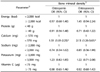
Nutrient intakes expressed as %RNI, 2010 KDRI is reported in Table 3. All the nutrients except energy, sodium, and iron showed similar patterns: highest percentage of RNI in the normal bone health group and lowest percentage of RNI in the osteoporosis group. The percentage of the RNI of Ca was the lowest in all of the three bone health groups: 79.2 + -4.8% in the normal bone health group, 66.8% in the osteopenia group, and 54.5% of RNI in the osteoporosis group. As for sodium, 2000 mg of intake goal KDRI was employed and all of the three bone health groups showed 341.1% in the normal bone health group, 291.2% in the osteopenia group, and 307.1% in the osteoporosis group, showing no difference in the percentage of recommended intake. In the osteoporosis group the percentage of RNI was the lowest, especially for Ca (54.5%), potassium (67.3%), riboflavin (63.7%), niacin (8.7%), and Vitamin C (82.6%), showing low intake of vegetables and dairy products. Although the bone health status was in the normal range, women in this group showed relatively low intake of Ca and potassium.
The odds ratio for the nutrients in three bone health group were analyzed after adjusting on age, body mass index, and hormone supplements intake. The result was reported in Table 4. The EAR values were used for each nutrient for logistic analysis whose baseline was the intake goal by the KDRI. When consumed less than 570 mg of the daily average calcium requirement, the osteopenia group odds ratio was 1.51 (95% CI 1.01-2.25) versus the normal group (ORs: 1): the osteoporosis group odds ratio was 2.13 (95% CI 1.26-3.61) versus the normal group (ORs : 1), (P < 0.05).
As for calcium, reduced risk for osteopenia and osteopenia incidence occurred when nutrient intake was more than the EAR value.
As for energy intake, the osteopenia group odds ratio in over 2,000 kcal/day was 0.97 (95% CI 0.68-1.40) versus the normal group (ORs : 1): the osteoporosis group odds ratio was 1.45 (95% CI 0.94-2.24) versus the normal group (ORs : 1), but it was not significant. The ORs of protein intake (over 40g) was 0.91 in the osteopenia group (95% CI 0.56-1.48 vs. normal group ORs 1) and 0.71 in the osteoporosis group (95% CI 0.42-1.22, vs. normal group ORs 1), which was not statistically significant. The risk of osteoporosis tended to decrease as sodium intake decreased. It tended to decrease as potassium and vitamin C intake increased but the effect was not statistically significant.
Food group intake frequencies of study participants according to bone health status are reported in Table 5. Except for grains, the staple food of the Koreans, and vegetables (the everyday dish of ordinary people in Korea), all of the food group intake frequencies showed the same trend: the bone health improves as each food's consumption frequency increases. All of the food groups, such as beans (P < 0.05), potatoes (P < 0.05), meat (P < 0.001), fish (P < 0.001), seaweeds (P < 0.001), fruits (P < 0.001), dairy products (P < 0.001), alcoholic drinks (P < 0.01), fast food (P < 0.01) and beverage (P < 0.001), showed the most frequent consumptions in the normal bone health group and the least frequent consumptions in the osteoporosis group.
For the weekly dairy products, usually recommended as a good source of Ca, the intake frequency was 4.2 ± 0.2 in the normal bone health group, 3.6 ± 0.1 in the osteopenia group, and 2.2 ± 0.2 in the osteoporosis group, showing a gradual decrease in that order (P < 0.001). The intake frequency of the normal group was almost twice that of the osteoporosis group but still lower than the average of 4 times per week. This finding confirms the previous findings that the main source of Ca for the Korean elderly was vegetables, beans, seaweeds, and grains. Grains and vegetables, the most frequently consumed foods among the Korean elderly, did not show any statistical differences in intake frequencies among the three bone health groups.
The odds ratio analysis results of food intake frequency in the osteopenia group and the osteoporosis group are reported in Table 6. In all food groups, as the intake frequencies increased, the risk of osteoporosis or osteopenia decreased after adjusting for age factor except in case of soft drinks, which showed increased risk of deteriorated bone health as consumption frequency increased.
Risk of osteoporosis decreased as intake frequency increased. The odds ratio of Q2 compared to Q1 was 0.63 (95% CI; 0.37-1.06) and that of Q3 was 0.40 (95% CI; 0.21-0.75, P for trend < 0.05). The osteopenia group also showed a similar trend but was not statistically significant.
The fruit consumption frequency also showed a similar preventive effect against the risk of osteoporosis: a high frequency showed a lower odds ratio of 0.42 (95% CI; 0.23-0.79, P for trend < 0.05). In case of osteopenia, a similar tendency was shown but it was not statistically significant.
As for beans, the risk of osteoporosis decreased as intake frequency increased, showing an odds ratio of 0.49 (95% CI; 0.29-0.83, P for trend < 0.01). The seaweeds also showed a preventive effect against osteoporosis and osteopenia. The risk of osteoporosis decreased to 0.55 (95% CI; 0.32-0.94, P for trend < 0.01) and the risk of osteopenia decreased to 0.51 (95% CI; 0.32-0.81, P for trend < 0.01).
The fish consumption also showed a decreased risk of osteoporosis and odds ratio 0.65 (95% CI; 0.32-0.98, P for trend < 0.05). Higher consumption frequency of meat and vegetables also showed a similar tendency but was statistically insignificant. Higher consumption frequency of soft drink showed an opposite effect, increasing the odds ratios both for osteoporosis and osteopenia as consumption frequencies increased, but such was not significant.
This study analyzed the odds ratio of nutrient intake level and frequencies for osteoporosis and osteopenia, controlling for age, BMI, and female hormone intakes for the postmenopausal women in Korea. In addition, the Chi-square analysis were carried out in order to assess the association between bone health status and such environmental factors as household income, education level, number of family members, and type of residence.
Several studies suggest age as one of the most important predictors of osteoporosis as its negative correlation with bone mineral density is statistically significant [15,16,17,18]. Aging activates osteoclast, accelerating drop in bone mineral density. Therefore, the best way to prevent osteoporosis is reaching the maximum bone mineral mass around the age of 35 [19]. Women, with both their average and maximum bone mass lower and their bone loss about 10% higher than those of men in all ages, are considered especially vulnerable against osteoporosis. Especially vulnerable are those in the phase of postmenopause, during which they lose 40 to 50% of their maximum bone mass [19]. Put together, these findings suggest the needs for effective preventive measures against osteoporosis for the aging postmenopausal women.
Such environmental factors as level of education, economic status, and family size are known to affect women's dietary behaviors, and their links to bone health appeared statistically significant for the subjects in this study as well. Previous studies generally suggested a negative association between levels of education and osteoporosis, as lower education level was associated with insufficient knowledge of and preventive measures against osteoporosis [20], while women with higher levels of education in general were socio-economically more stable and more exposed to medical assistance [21]. The level of education seemed to influence women's awareness of osteoporosis, as women with higher education tended to seek more knowledge regarding the disease's characteristics and dietary measures against it [22]. Such link was established in this study as well. That the prevalence rate of the disease appeared lower for those living in apartments compared to those living in independent housing suggested a link between income level and bone mineral density status.
Family size appeared positively associated with bone health, and it can be argued that similar to income levels, family size affects bone health through the subjects' choice, quality of food, and intake frequencies.
In this study, the subjects' prevalence rate of osteoporosis increased with BMI. The previous studies on BMI and bone density suggested that postmenopausal women's BMI and bone density are positively correlated [16,23,24,25,26,27,28,29]. For women over 40 years of age, being underweight is one of the main risk factors of osteoporosis [30,31], and loss of bone density seems to be prevalent among underweight postmenopausal women [32]. It has been argued that underweight or smaller women are more vulnerable to the disease for their lower bone mass and fat accumulation [33].
The subjects took higher levels of protein, phosphorus, iron, sodium, thiamin, niacin, vitamin A and vitamin C, and lower levels of energy, fiber, calcium, potassium and riboflavin compared to the KDRIs' RI [14]. The intake levels of potassium and riboflavin were especially low among the subjects in the osteopenia group and the osteoporosis group. All three groups showed intake levels of calcium much lower than 570 mg/day (EAR), and the odds ratio analysis also suggested higher risks of osteoporosis and osteopenia for those with insufficient calcium intakes, when age, BMI, and female hormone intakes were controlled.
A previous study has reported that BMD increased as Ca intakes increased, and that the risk of osteoporosis incidence was reduced when more than 1 serving of milk or dairy products were consumed and serum 25 (OH) vitamin D level was maintained in the normal range [34]. Thus, Ca, milk, and dairy product intake was considered important for the maintenance of bone health and the prevention of osteoporosis in adults.
The subjects in the osteopenia group and the osteoporosis group showed lower intake frequencies for all food groups except for grains and vegetables, while it should be noted that those are staple foods in Korean culture. Especially lower in terms of intake frequencies among the two groups were milk and dairy products, showing only about half of those among the normal group. Lower levels of intake frequencies of milk and dairy products can lead to insufficient intake of calcium or riboflavin. Therefore, increased intake of such animal foods as milk and dairy products, rather than plant foods with high contents of fiber and phytic acids, has been suggested in order to supplement calcium intakes [35]. Studies on milk intake showed that menopausal women who consumed large amounts of milk tended to have higher bone mineral density, as increased calcium intake prevented bone absorption [35,36].
Calcium supplementary intervention studies argue that consumption of calcium-rich foods and calcium supplements is effective against loss of bone mass with age. Rather than the calcium supplements, calcium-rich foods have generally been recommended [37] as the supplements can aggravate heart diseases among menopausal women over 80 years of age and can cause such side effects as digestive problems, vomiting, and diarrhea [38]. According to previous studies osteopenia and osteoporosis groups had lower intake percentage of milk, vegetables, and fruits than the normal group [39,40]. In addition, it was reported that there was significant positive relationship between the intake of vegetables and fruits and the bone mineral densities. Therefore, intake of milk and dairy products, at least once a day, is suggested for bone health [14].
This study found that the bone mineral density among postmenopausal women in Korea appears to be positively associated with education, income, and family size, and negatively associated with age. Therefore, aged and underweight women with low income and living alone can be regarded as the most vulnerable group. These environmental factors influence Korean women's postmenopausal bone health through their dietary behaviors.
Korean postmenopausal women's nutrients intakes and foods intake frequencies were both lower than the recommended levels. The odds ratio analysis showed that upon controlling age, BMI, and hormone intakes, higher food intake frequencies of milk and dairy products, beans, fish, seaweeds and fruits and nutrient intake ratios were associated with lower risks of bone loss and osteoporosis. This tendency was stronger for calcium-rich foods.
Controlling for age, hormone intake, and BMI, insufficient intake of calcium and low intake frequencies of such calcium-rich foods as dairy products, beans, and fish were specifically identified as the main factors that cause osteoporosis. In addition, paying attention to such environmental factors as income, education, and family size, which affect dietary behaviors, appears reasonable. Some of the specific policy suggestions include the following: dissuading women from excessively reducing weight as underweight women are vulnerable to bone diseases; providing dietary recommendations including balanced dietary information and RNI; and developing lifestyle intervention programs targeted at low-income and aged women living alone, who are identified as the most vulnerable group against bone diseases as such environmental conditions tend to lead to unhealthy dietary practices.
This study aimed to evaluate the prevalence of osteoporosis according to nutrient and food group intakes in Korean postmenopausal women using cross-sectional databases, with limited explanation for the relationship between risk dietary factor and bone mineral density status. Bone mineral density status rests on a combination of several factors including a healthy diet with an adequate amount of calcium, protein, and mineral nutrients. In this regard, optimal protection of bone requires a diet rich in dairy products, fruits, and vegetables and an adequate amount of meat and fish. Furthermore, mineral supplementation, exercise, and lifestyle should be closely evaluated. Further study is needed for longitudinal study as a guideline for interventions to risk factors related to osteoporosis.
Figures and Tables
References
1. Jang JY, Chung HY, Hwang YC, Jeong IK, Ahn KJ, Kwon MK, Chon S, Oh S, Woo JT, Kim SW, Kim JW, Kim YS. Dietary calcium intake and bone metabolism in Korean postmenopausal women. Korean J Bone Metab. 2008; 15:143–149.
2. Kwon JH, Choi YM, Lee YH, Lee JY. The bone mineral densities in Korean postmenopausal women: a comparison between natural and surgically induced menopause. Korean J Obstet Gynecol. 2000; 43:842–852.
3. Slemenda CW, Hui SL, Longcope C, Johnston CC Jr. Cigarette smoking, obesity, and bone mass. J Bone Miner Res. 1989; 4:737–741.

4. National Osteoporosis Foundation (US). America's Bone Health: The State of Osteoporosis and Low Bone Mass in Our Nation. Washington D.C.: National Osteoporosis Foundation;2002.
5. Ilich JZ, Kerstetter JE. Nutrition in bone health revisited: a story beyond calcium. J Am Coll Nutr. 2000; 19:715–737.

6. Go G, Tserendejid Z, Lim Y, Jung S, Min Y, Park H. The association of dietary quality and food group intake patterns with bone health status among Korean postmenopausal women: a study using the 2010 Korean National Health and Nutrition Examination Survey Data. Nutr Res Pract. 2014; 8:662–669.

7. Koo JO, Park S. Analysis of BMI menopose, blood pressure and dietary habits affecting born mineral density of 30-60 years women. Korean J Community Nutr. 2010; 15:403–414.
8. Kim KH. A study on the development of residential community for aged society [master's thesis]. Suwon: Ajou University;2008.
9. Jeon JD. Prevalent status and associated factor of osteoporosis in adult women [master's thesis]. Gwangju: Chosun University;2000.
10. You MH, Son BS, Park JA, Kim JO, Yang WH. Patterns of bone mineral density of adult women and its causal factors in Suwon, Korea. Korean J Sanit. 2004; 19:71–80.
11. Oh SI, Lee HS, Lee MS, Kim CI, Kwon IS, Park SC. Some factors affecting bone mineral status of postmenopausal women. Korean J Community Nutr. 2002; 7:121–129.
12. Park JC, Kweon HJ, Oh YK, Do HJ, Oh SW, Lym YL, Choi JK, Joh HK, Cho DY. Association of the metabolic syndrome and bone mineral density in postmenopausal women. Korean J Fam Med. 2010; 31:9–15.

13. Song YD, Lim SK, Chung YS, Park SW, Chung CH, Ahn KJ, Lee EJ, Lee HC, Huh KB, Choi MS, Paik IK, Lee JH. The effect of body fat on bone density in pre-and postmenopausal women. J Korean Soc Endocrinol. 1993; 8:251–258.
14. The Korean Nutrition Society. Dietary Reference Intakes for Koreans. Seoul: The Korean Nutrition Society;2010.
15. Kim MS, Koo JO. Analysis of factors affecting bone mineral density with different age among adult women in Seoul area. Korean J Community Nutr. 2007; 12:559–568.
16. Kang TH, Park YK, Kim EH, Kim SM, Oh HJ. Spinal bone mineral density related with YSM in Korean menopausal women. J Korean Acad Fam Med. 2002; 23:224–232.
17. Youk JI. Female bone mineral density in an urban area and its relation with contributing factors [master's thesis]. Daejeon: Chungnam National University;2004.
18. Kim BS. Comparision of related factors of bone mineral density of postmennopausal women in urban and rural areas [master's thesis]. Iksan: Wonkwang University;2007.
19. Kim JG, No JH, Hong JS, Kim SH, Choi YM, Moon SY, Lee JY. A study on risk factors for postmenopausal osteoporosis. Korean J Obstet Gynecol. 2001; 44:1621–1626.
20. Byun YS, Kim OS. Life style and self-efficacy in osteoporsis women. J Korean Acad Nurs. 1999; 29:530–540.

21. Jeon JD. Prevalent status and associated factors of osteoporosis in adult women [master's thesis]. Gwangju: Chosun University;2001.
22. Chung M, Hwang K, Choi E. Study of the level of osteoporosis awareness among women dwelling in urban area. Korean J Women Health Nurs. 2009; 15:362–371.

23. Sung CJ, Choi SH, Kim MH, Choi YH, Lee DH, Baek SK, Kim HK, Choi MK. A study on nutritional status, maternal factors, and lifestyles according to BMD in rural postmenopausal women. Korean J Community Nutr. 2001; 6:192–204.
24. Carranza-Lira S, Rosas M, Murillo A, Martinez N, Santos J. Osteoporosis in postmenopausal women (Mexico City): 1. Risk factors. Int J Fertil Womens Med. 2002; 47:22–25.
25. Lee JS, Yu CH. Some factors affecting bone mineral density of Korean rural women. Korean J Nutr. 1999; 32:935–945.
26. Kim KR, Kim KH, Lee EK, Lee SS. A study on the factors affecting bone mineral density in adult women: besed on the mothers of elementary school students. Korean J Nutr. 2000; 33:241–249.
27. Na NS. A study on factors related to bone density of women living in Seoul [master's thesis]. Seoul: Korea National Open University;2009.
28. Choi SH, Hwang DK, Song HR, Noh HJ, Kang JY, Choi DH, Choi HJ. The predictors of lumbar spinal bone mineral density in pre- and postmenopausal women. J Korean Soc Menopause. 2009; 15:101–109.
29. Hong JY, Choue R. The Effects of vitamin K supplements on serum osteocalcin caraboxylation in postmenopausal women. Korean J Nutr. 1999; 32:726–731.
30. Choi JY, Han S, Shin A, Shin CS, Park SK, Cho SI, Kang D. Prevalence and risk factors of osteoporosis and osteopenia in Korean women: cross-sectional study. J Korean Soc Menopause. 2008; 14:35–49.
32. Daniell HW. Osteoporosis of the slender smoker. Vertebral compression fractures and loss of metacarpal cortex in relation to postmenopausal cigarette smoking and lack of obesity. Arch Intern Med. 1976; 136:298–304.

33. Lufkin EG. Therapeutic alternatives for postmenopausal osteoporosis. Compr Ther. 1992; 18:14–17.
34. Baeksgaard L, Andersen KP, Hyldstrup L. Calcium and vitamin D supplementation increases spinal BMD in healthy, postmenopausal women. Osteoporos Int. 1998; 8:255–260.

35. Wardlaw GM, Insel PM. Perspectives in Nutrition. 3rd ed. St. Louis (MO): Mosby;1995.
36. Na SG, Son HY, Yang GH, Jang JS, Choi YG. Osteoporosis. Seoul: Ses-Heung Publishing Company;2000.
38. Bolland MJ, Barber PA, Doughty RN, Mason B, Horne A, Ames R, Gamble GD, Grey A, Reid IR. Vascular events in healthy older women receiving calcium supplementation: randomised controlled trial. BMJ. 2008; 336:262–266.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download