Abstract
BACKGROUND/OBJECTIVES
Breast milk is the best available food for optimum growth and development of infants and the breastfeeding rate is increasing in Korea. The purpose of this study is to measure the concentrations of macronutrients and to evaluate their changes according to lactation period in breast milk from lactating Korean women.
SUBJECTS/METHODS
Milk samples were obtained from 2,632 healthy lactating women (mean age; 32.0 ± 3.3 years), where the lactating period was up to a period of 8 months, who also volunteered to participate in the Human Milk Macronutrient Analysis Research. Lactose, protein, fat and water content in the breast milk samples were analyzed with infrared spectrometry using MilkoScan FT-2.
RESULTS
The mean macronutrient composition per 100 mL of mature breast milk was 7.1 g for lactose, 1.4 g for protein and 3.0 g for fat, and energy content was 61.1 kcal. The protein concentration was significantly lower in milk samples at 1-2 weeks (2.0 g/dL) to 2-3 months (1.4 g/dL) than those at 0-1 week (2.2 g/dL), but it was similar among samples from 3-4 months to 7-8 months (1.3 g/dL). Mean lipid levels varied among different lactational period groups (2.7-3.2 g/dL), but presented no significant difference. Lactose concentration in the milk samples did not differ with lactation period. Maternal body mass index was positively related to protein and lipid breast milk contents, but was negatively related to lactose content. General linear models examining the associations between maternal variables and milk macronutrient content revealed that lactation period had a major impact on protein and lipid, but not on lactose content in breast milk.
Human breast milk, with its unique combination of essential nutrients and numerous bioactive factors [1], provides ideal nourishment and benefits to human infants for their survival, growth and development including brain development and cognition [23]. Exclusive breast milk feeding for the first 6 months is recommended by the WHO [4] and UNICEF [5], and, this recommendation is adopted by many nations [67] including Korea [8].
Owing to increased awareness of the nutritional, immunological and cognitive benefits of human breast milk as well as food safety issues, there was a rising trend in the exclusive breast feeding rate during the first 6 months from less than 10% in 2000 to 36.2% in 2009 [9]. However, the breast feeding rate in Korea failed to continue to increase and is rather stagnant to a current level of 25% [10] to 23.9% [11].
Determination of human breast milk composition has been a topic of extensive research among various populations and ethnic groups around the world [112131415]. Despite the heightened interest in breastfeeding, only a few reports have been published in Korea on the composition of human milk let alone other bioactive factors. Most of the existing studies, however, were conducted in the 1980s and 1990s [161718192021], more than 20 years ago and were subject to small sample numbers using separate analytical instruments for protein, fat, and lactose, which was time consuming.
Recent advancements in human milk analytical instruments using infrared spectrometry have made rapid analysis of macronutrient composition in breast milk samples possible. Although many reports on the macronutrient and energy level of human milk samples are available in several countries [122223] using this rapid analysis, only one study report is available in Korea [24]. Using a simplified model of the infrared spectrometry instrument, the report showed that macronutrient and energy level in breast milk vary significantly according to the body weight of infants, with protein and lactose being more variable than lipids. No other studies in Korea, to the best of our knowledge, have reported the macronutrient composition of breast milk in a large number of samples using a full spectrum infrared spectrometry method. We report in this paper the macronutrient and energy content of breast milk during the lactation periods of up to 240 days in Korean lactating women (n = 2,632).
Study subjects were lactating mothers from Postpartum Care Centers, Baby Fairs, and Breastfeeding Seminars, who agreed to participate in the study. From March 2013 to July 2014, a total of 3,271 lactating mothers were recruited. They were from Postpartum Care Centers in Seoul (n = 429) and 6 metropolitan cities [Busan (n = 64), Daejeon (n = 306), Daegu (n = 15), Gwangju (n = 140), Incheon (n = 15), Ulsan (n = 28)] and 21 cities from 5 provinces [Gyeonggi 9 cities (n = 201), Chungcheong 3 cities (n = 73), Gangwon 3 cities (n = 191), Gyeongsang 5 cities (n = 168), Jeonla 2 cities (n = 76) and an unidentified residential area (n = 1)]. Human milk samples were collected from lactating mothers who attended the Baby Fair held in Seoul (n = 361), Daejeon (n = 154), Daegu (n = 350), Gwangju (n = 157) and Busan (n = 489), and also from Breastfeeding Seminars held in 4 cities from 4 provinces [Gyeonggi Suwon (n = 13), Kangwon Wonju (n = 8), Chungcheong Cheonan (n = 13), Jeju Island (n = 19)].
Study participants were interviewed by trained interviewers. General information on demographic factors, socioeconomic factors, anthropometry (height, body weight before pregnancy and at the time of data collection), and health-related behaviors (cigarette smoking, alcohol drinking, and use of dietary supplements) was collected. Further information on pregnancy outcomes such as gestational age at delivery (weeks), neonatal gender, birth weight (g) and length (cm), as well as age (days) and body weight at sample collection was obtained from baby record books. The study protocols and consent forms were approved by the Institutional Review Boards (0627-201408-HRBR-002-03) at Maeil Human Milk R & D Center. All participants provided informed consent to participate in the study.
From a total of 3,271 lactating women, 128 women whose gestational ages were < 37 weeks or ≥ 43 weeks and 65 who delivered babies with low birth weight (< 2.5 kg) or macrosomia (> 4.5 kg) were excluded. Of the remaining women, 210 women whose babies were ≥ 240 days old were excluded. Among the remaining subjects, 236 women whose BMI (body mass index) data were missing were excluded. Therefore, a total of 2,632 women and their babies were eligible for the final analysis.
The breast was cleaned with water and the breast milk (45 mL) was pumped, collected into a sterilized conical tube, and sent to the Maeil Human Milk R & D Center in an ice packed container. The breast milk samples were stored at -20 until analysis. No specific time during the day was defined for expressing breast milk samples. The full expression of milk was collected to prevent the collection of hindmilk or foremilk.
The frozen samples were thawed in a refrigerator and heated in waterbath until 37℃ then homogenized before analysis. The fat, lactose and protein in the breast milk samples were analyzed using MilkoScan FT2 (Foss Analytical, Denmark). The MilkoScan is an infrared based milk analyzer that determines milk components (i.e. fat, protein, lactose, total solids and solids-non-fat). Within the infrared spectrum, fat, lactose and protein have characteristic absorption wavelengths. When the intensity of the light transmitted at precisely these wavelengths is measured, the concentration of the component is determined. The MilkoScan analysis data was in good agreement with that of conventional methods [252627] (r = 0.990, 0.999, 0.989 for protein, fat and lactose concentrations, respectively).
Statistical analyses were carried out using SAS 9.3 software (SAS Inc., Cary, NC, USA). The analysis of variance (ANOVA) and Scheffe's Test were used to compare milk composition at each lactation period. Partial correlation analyses, adjusted for lactating women's age, were used to examine the relationships between the current BMI of lactating women and the concentrations of milk components at each lactation period. After adjusting for age and current BMI of lactating women, general linear models were used to examine the associations between maternal variables and macronutrient concentrations in human milk. The regression coefficients of the other seven periods were relative values compared to the reference (0-1 week). The significance was defined as P < 0.05.
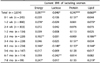
The maternal subjects were 32.0 ± 3.3 years old and had a pre-pregnancy BMI of 20.9 ± 2.8 kg/m2 (Table 1). The mean macronutrient composition per 100 mL of mature breast milk (1-8 months) was 7.1 g for lactose, 1.4 g for protein and 3.0 g for fat, and energy content was 61.1 kcal. Mean energy and lipid levels varied among the different 10 groups according to the lactation period, but compared to milk samples at 0-1 week, energy and lipid levels of those at 1-2 weeks, 2-4 weeks, 1-2 months, 2-3 months, 3-4 months, 4-5 months, 5-6 months, 6-7 months and 7-8 months presented no statistical differences. Lactose concentration also did not differ among all groups according to the lactation period. Protein concentration was significantly lower in samples at 1-2 weeks, 2-4 weeks, 1-2 months, and 2-3 months than those at 0-1 week and did not differ among samples at 3-4 months, 4-5 months, 5-6 months, 6-7 months and 7-8 months (Table 2).
After adjusting for maternal age, the current BMI was positively correlated with energy levels at 1-2 weeks, 2-3 months, 4-5 months, and 7-8 months, with protein levels at 0-1 week, 3-4 months, and 4-5 months, and with lipid levels at 1-2 weeks, 2-3 months, and 7-8 months, respectively. The current BMI was negatively correlated with lactose concentrations at 4-5 months and 6-7 months (Table 3).
Results from the general linear models examining the associations between maternal variables and milk macronutrients concentrations are shown in Table 4. The lactation period had a major impact on protein and lipid levels in breast milk, but not on lactose. The explanatory power of the regression model was 56.9% for protein. The current BMI of lactating women was positively associated with energy, protein and lipid, and negatively with lactose concentration.
We found that, among the macronutrients, protein and lipid levels were different depending of the periods of lactation. As for protein, the concentration was low in the later periods of lactation compared to that at 0-1 week, whereas for lipids, it was vice versa with no statistical difference. Lactose concentration did not differ with lactation periods. Maternal current BMI was positively associated with the breast milk content of protein, lipids and energy, and negatively associated to that of lactose.
The milk protein content in our study was high compared to mature milk from well-nourished Swedish mothers (0.8-0.9 g/dL [28]) but comparable to that of Chinese (1.58 g/ dL [29]) and Japanese mother (1.26 g/ dL [30]). The mean protein concentration was lower in samples at 1-2 weeks (2.0 g/dL), 2-4 weeks (1.8 g/ dL), 1-2 months (1.5 g/dL), and 2-3 months (1.4 g/dL) than those at 0-1 week (2.2 g/ dL) and did not differ among samples at 3-4 months (1.3 g/dL), 4-5 months (1.3 g/dL), 5-6 months (1.3 g/dL), 6-7 months (1.3 g/dL) and 7-8 months (1.2 g/dL). The high protein content in the breast milk of our subjects is in part due to the inclusion of non-protein nitrogenous substances. When we consider the amount of nitrogen from non-protein sources (approximately 25% of total nitrogen) in human milk, the protein concentration in mature breast milk samples (1.3 g/dL) from our study subjects is similar to that of other developed nations (0.9 g/dL [1]). In our study, the protein concentration was positively related with maternal current BMI, confirming the reports of other investigators [31].
The lipid content in the breast milk of our participants was lower in transitional milk (2.7 g/dL) than in mature milk (3.0 g/dL), which did not differ during the lactation period. Similar to milk protein, milk fat content was positively related with maternal BMI. This is in line with results from previous studies [1232]. The milk fat content in our study was low compared to that in China (3.4 g/dL [12]), Japan (3.56 g/dL [30]) and US (3.6 g/dL [31]). Fat is known to be the most variable macronutrient in human milk. It has been reported that fat content varies depending on maternal diet [33], hind- or fore-milk [34], morning/night or daytime/early evening feeding [35], and storage conditions [36].
Lactose concentration (7.1 g/dL) did not differ according to the lactation period with very little inter-individual variations. This was similar to recent data from China (7.1 g/dL [12]), but higher than that from Australia (6.0 g/dL [34]) and Brazil (6.4-6.5 g/dL [13]). Although, the concentration of lactose in human milk is known to be the least variable of the macronutrients, it has been reported to vary from 6.3 to 8.1 g/dL [37]. Lactose, a source of galactose, is essential in the production of galactolipids in the central nervous system. Human milk contains the highest level of lactose [38] suitable for the development of the large human brain. Lactose is also believed to provide beneficial effects for gut physiology, including prebiotic effects, softening of stools, and enhancement of water, sodium and calcium absorption [39].
Energy content in mature milk [2-4 weeks (64.7 kcal/dL)] was higher than that in colostrum [0-1 weeks (61.4 kcal/dL)] as well during later periods of lactation [4-5 months (59.7 kcal/dL), 5-6 months (60.3 kcal/dL)]. The differences in protein contents contributed to the energy content variations in mature milk depending on periods of lactation.
Our study results showed that the nutritional composition of breast milk from Korean mothers is comparable to other developed countries [4041]. Confirmation that the nutritional composition of their breast milk is acceptable will serve as positive feedback and motivational factor for Korean lactating mothers to maintain continued breastfeeding. Breastfeeding rates during the first six months in Korea have changed dramatically in recent decades [1042] due to increased awareness of the nutritional, psychological, cognitive and economic benefits of breastfeeding among Korean mothers. A more supportive socio-environment such as breastfeeding room facilities that are easily accessible to lactating mothers has facilitated a rising trend in breastfeeding [4243]. Sporadic but recurrent outbreak of food safety issues in infant formula [4445] has also been a significant contributing factor for a surge in the breastfeeding rate in Korea. And yet, exclusive breastfeeding for 6 months in Korea is still far from the 2015 goal of 56% [46]. One of the major factors for such low exclusive breastfeeding rate in Korea is the mother's lack of confidence in the milk volume and nutritional composition of her own milk [47].
Our study has several limitations. Even though our study participants were from all regions of Korea, the results of our study cannot be generalized as country representative because our data were generated from convenience samples. All of the breast milk samples were not necessarily from mothers practicing exclusive breast feeding. We have no way of knowing whether a particular sample was from a mother practicing exclusive breast feeding or not. The volume and nutritional composition of breast milk is known to fluctuate most according to the infant's needs as well as the time of day, foremilk or hindmilk of a particular feeding. No specific time during the day was defined for expressing breast milk samples. However, we asked lactating women to express their breast milk samples at a time other than the babies' feeding time to minimize the chances of collecting foremilk or hindmilk from a particular feeding. The protein content in our breast milk samples did not take into consideration the nitrogen content of non-protein nitrogen sources. Considering the fact that approximately 25% of total nitrogen in human milk is from non-protein sources, the actual protein content will be much lower, which is similar (-1 g/dL) to other reports. Determination of amino acids and total protein will need to be performed in future research. Nevertheless, by utilizing a very large sample size from all regions of Korea in combination with a well-calibrated analytical method with high precision for analysis, our study provided, for the first time, reliable data on the macronutrient composition of breast milk in Korea.
Human milk macronutrient composition research is important because human milk not only provides energy but also essential amino acids, essential fatty acids and lactose, critical for infant growth and development. These data on breast milk composition have many potential practical applications such as developing infant formulas that more closely resemble human milk and setting nutrition standards such as the Dietary Reference Intakes for infants. All of these efforts will contribute toward achieving optimum health and development in infants.
Figures and Tables
References
1. Ballard O, Morrow AL. Human milk composition: nutrients and bioactive factors. Pediatr Clin North Am. 2013; 60:49–74.
2. Isaacs EB, Fischl BR, Quinn BT, Chong WK, Gadian DG, Lucas A. Impact of breast milk on intelligence quotient, brain size, and white matter development. Pediatr Res. 2010; 67:357–362.

3. Kramer MS, Aboud F, Mironova E, Vanilovich I, Platt RW, Matush L, Igumnov S, Fombonne E, Bogdanovich N, Ducruet T, Collet JP, Chalmers B, Hodnett E, Davidovsky S, Skugarevsky O, Trofimovich O, Kozlova L, Shapiro S. Promotion of Breastfeeding Intervention Trial (PROBIT) Study Group. PROBIT) Study Group. Breastfeeding and child cognitive development: new evidence from a large randomized trial. Arch Gen Psychiatry. 2008; 65:578–584.
4. World Health Organization (CH). Unicef (US). Global Strategy for Infant and Young Child Feeding. Geneva: World Health Organization;2003.
5. Unicef (US). Infant and young child feeding [Internet]. New York (NY): Unicef;2014. cited 2015 June 1. Available from: http://www.unicef.org/nutrition/index_breastfeeding.html.
6. Section on Breastfeeding. Breastfeeding and the use of human milk. Pediatrics. 2012; 129:e827–e841.
7. Department of Health (GB). Infant feeding recommendation [Internet]. London: Department of Health;2003. cited 2015 June 1. Available from: http://www.dh.gov.uk/prod_consum_dh/groups/dh_digitalassets/@dh/@en/documents/digitalasset/dh_4096999.pdf.
8. Ministry of Health and Welfare, Korea Center for Disease Prevention and Control. National Health Insurance Service. Manual of Pediatric Physical Examination 2015. Cheongju: Korea Center for Disease Prevention and Control;2015.
9. Kim SG, Kim YK, Kim HR, Park JS, Son CK, Choi YJ, Kim YW, Lee GE, Yoon AR. The status of breast-feeding. The 2012 National Survey on Fertility, Family Health & Welfare in Korea. Seoul: Korea Institute for Health and Social Affairs;2012. p. 415–441.
10. Lee WS, Cho J, Choi YS, Chung SH, Bae CW, Jung JA. Breastfeeding rate in below 6 months infants during recent 6-year in Korea based on childcare database. Neonatal Med. 2013; 20:221–227.

11. Ministry of Health and Welfare, Korea Centers for Disease Control and Prevention. Korea Health Statistics 2013: Korea National Health and Nutrition Examination Survey [KNHANES VI-1]. Cheongju: Korea Centers for Disease Control and Prevention;2014.
12. Yang T, Zhang Y, Ning Y, You L, Ma D, Zheng Y, Yang X, Li W, Wang J, Wang P. Breast milk macronutrient composition and the associated factors in urban Chinese mothers. Chin Med J (Engl). 2014; 127:1721–1725.
13. Abranches AD, Soares FV, Junior SC, Moreira ME. Freezing and thawing effects on fat, protein, and lactose levels of human natural milk administered by gavage and continuous infusion. J Pediatr (Rio J). 2014; 90:384–388.

14. Quinn EA, Largado F, Power M, Kuzawa CW. Predictors of breast milk macronutrient composition in Filipino mothers. Am J Hum Biol. 2012; 24:533–540.

15. Thakkar SK, Giuffrida F, Cristina CH, De Castro CA, Mukherjee R, Tran LA, Steenhout P, Lee le Y, Destaillats F. Dynamics of human milk nutrient composition of women from Singapore with a special focus on lipids. Am J Hum Biol. 2013; 25:770–779.

16. Lee JS. Changes in specific gravity, total solid and protein contents of human milk during the course of lactation in Korean women. Korean J Nutr. 1988; 21:129–133.
17. Lee SG, Chung TH. Lipid content of breast milk in Korean women. J Korean Pediatr Soc. 1985; 28:977–988.
18. Kim SK, Ra CS. Quantitative determination of lipids in breast milk of Korean woman. J Korean Pediatr Soc. 1986; 29:67–74.
19. Song SW, Moon SJ, Ahn HS. Ecological study of the changes in the components of human milk during the breast feeding and the relationships between the dietary behavior of lactating women and the growth of breastfed infants: I. A study on the nitrogen content in human milk. Korean J Nutr. 1990; 23:179–186.
20. Choi MH, Moon SJ, Ahn HS. An ecological study of changes in the components of human milk during the breast feeding and the relationships between the dietary behavior of lactating women and the growth of breast-fed infants: II. A study on the lipids content in human milk. Korean J Nutr. 1991; 24:77–86.
21. Moon SJ, Lee MJ, Kim JH, Kang JS, Ahn HS, Song SW, Choi MH. A longitudinal study of the total nitrogen, total lipid, and lactose contents in human milk and energy intake of breast-fed infants. Korean J Nutr. 1992; 25:233–247.
22. Michaelsen KF, Pedersen SB, Skafte L, Jaeger P, Peitersen B. Infrared analysis for determining macronutrients in human milk. J Pediatr Gastroenterol Nutr. 1988; 7:229–235.

23. de Halleux V, Close A, Stalport S, Studzinski F, Habibi F, Rigo J. Advantages of individualized fortification of human milk for preterm infants. Arch Pediatr. 2007; 14:Suppl 1. S5–S10.
24. Min KB, Lee SM, Eun HS, Park MS, Park KI, Namgung R, Lee C. Analysis of the macronutrient composition of breast milk from Korean women and growth of infants. Korean J Perinatol. 2012; 23:259–265.
25. Corvaglia L, Battistini B, Paoletti V, Aceti A, Capretti MG, Faldella G. Near-infrared reflectance analysis to evaluate the nitrogen and fat content of human milk in neonatal intensive care units. Arch Dis Child Fetal Neonatal Ed. 2008; 93:F372–F375.

26. Casadio YS, Williams TM, Lai CT, Olsson SE, Hepworth AR, Hartmann PE. Evaluation of a mid-infrared analyzer for the determination of the macronutrient composition of human milk. J Hum Lact. 2010; 26:376–383.

27. Menjo A, Mizuno K, Murase M, Nishida Y, Taki M, Itabashi K, Shimono T, Namba K. Bedside analysis of human milk for adjustable nutrition strategy. Acta Paediatr. 2009; 98:380–384.

28. Lönnerdal B, Forsum E, Gebre-Medhin M, Hambraeus L. Breast milk composition in Ethiopian and Swedish mothers. II. Lactose, nitrogen, and protein contents. Am J Clin Nutr. 1976; 29:1134–1141.

29. Ding M, Li W, Zhang Y, Wang X, Zhao A, Zhao X, Wang P, Sheng QH. Amino acid composition of lactating mothers' milk and confinement diet in rural North China. Asia Pac J Clin Nutr. 2010; 19:344–349.
30. Morita A, Yoshiike N, Takimoto H, Tsubota-Utsugi M, Kodama H, Shimizu T, Sugiyama T, Tabata I, Tamai H, Tsutsumi C, Hirahara F, Kuzuya M, Gomi I, Nakamura K, Yoshida H, Nakamura M. Dietary reference intakes for Japanese 2010: lifestage. J Nutr Sci Vitaminol (Tokyo). 2013; 59:Suppl. S103–S109.

31. Nommsen LA, Lovelady CA, Heinig MJ, Lönnerdal B, Dewey KG. Determinants of energy, protein, lipid, and lactose concentrations in human milk during the first 12 mo of lactation: the DARLING Study. Am J Clin Nutr. 1991; 53:457–465.

32. Prentice AM, Goldberg GR, Prentice A. Body mass index and lactation performance. Eur J Clin Nutr. 1994; 48:Suppl 3. S78–S86.
34. Mitoulas LR, Kent JC, Cox DB, Owens RA, Sherriff JL, Hartmann PE. Variation in fat, lactose and protein in human milk over 24 h and throughout the first year of lactation. Br J Nutr. 2002; 88:29–37.

35. Kent JC, Mitoulas LR, Cregan MD, Ramsay DT, Doherty DA, Hartmann PE. Volume and frequency of breastfeedings and fat content of breast milk throughout the day. Pediatrics. 2006; 117:e387–e395.

36. Chang YC, Chen CH, Lin MC. The macronutrients in human milk change after storage in various containers. Pediatr Neonatol. 2012; 53:205–209.

37. Miller EM, Aiello MO, Fujita M, Hinde K, Milligan L, Quinn EA. Field and laboratory methods in human milk research. Am J Hum Biol. 2013; 25:1–11.

38. Picciano MF. Comparative lactation - humans [Internet]. Champaign (IL): Lactation Resource Library;2009. cited 2015 June 1. Available from: http://ansci.illinois.edu/static/ansc438/Lactation/humans.html.
39. Koletzko B, Baker S, Cleghorn G, Neto UF, Gopalan S, Hernell O, Hock QS, Jirapinyo P, Lonnerdal B, Pencharz P, Pzyrembel H, Ramirez-Mayans J, Shamir R, Turck D, Yamashiro Y, Zong-Yi D. Global standard for the composition of infant formula: recommendations of an ESPGHAN coordinated international expert group. J Pediatr Gastroenterol Nutr. 2005; 41:584–599.

40. Butte NF, Lopez-Alarcon MG, Garza C. Nutrient adequacy of exclusive breastfeeding for the term infant during the first six months of life. Geneva: World Health Organization;2002.
41. Wijnhoven TM, Bollars C, Tabacchi G, Hermoso M. Collate and review data on the composition and volume and intake of breast milk: results from a systematic literature review [Internet]. Brussels: EURopean micronutrient RECommendations Aligned;cited 2015 June 1. Available from: http://www.eurreca.org/downloadattachment/8565/9807/Report%20on%20the%20composition,%20volume%20and%20intake%20of%20breast%20milk.pdf.
42. Chung SH, Kim HR, Choi YS, Bae CW. Trends of breastfeeding rate in Korea (1994-2012): comparison with OECD and other countries. J Korean Med Sci. 2013; 28:1573–1580.

43. Kim HR. Trends of breastfeeding in Korea and other nations: strategic policy for improving breastfeeing in Korea. Issue Focus. 2011; 86:1–8.
44. Pei X, Tandon A, Alldrick A, Giorgi L, Huang W, Yang R. The China melamine milk scandal and its implications for food safety regulation. Food Policy. 2011; 36:412–420.

45. Mitternacht M. Botulism threat to infant milk formula [Internet]. place unknown: Sun Herald;2013. cited 2015 June 1. Available from: http://newsstore.fairfax.com.au/apps/viewDocument.ac?page=1&sy=nstore&kw=botulism+threat+AND+infant&pb=all_ffx&dt=selectRange&dr=entire&so=relevance&sf=text&sf=headline&rc=10&rm=200&sp=nrm&clsPage=1&docID=SHD130804DI7L638LA9H.
46. Ministry of Health and Welfare. National Health Plan 2020. Seoul: Ministry of Health and Welfare;2011.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download