Abstract
BACKGROUND/OBJECTIVES
Dietary pattern and its association with cardio-cerebrovascular disease have not been studied in Baoji city by now. This study was aimed to identify the dietary patterns among Chinese adults in Baoji, and explore the association between these dietary patterns and cardio-cerebrovascular disease.
SUBJECTS/METHODS
A total of 4,968 participants were included in this study at 12 counties. With multistage stratified random sampling and semi quantitative food frequency questionnaire, the prevalence of cardio-cerebrovascular disease and dietary intake were investigated in 2013. We used factor analysis to establish dietary patterns.
RESULTS
A total of 4,968 participants over 15 years old were included in this study. Five dietary patterns were identified in Baoji: protein, balanced, beans, prudent, and traditional patterns. The protein dietary pattern mainly included animal and plant proteins and was negatively associated with hypertension as well as stroke. The balanced pattern included carbohydrates, protein, and fat and was negatively associated with hypertension as well as stroke. The beans pattern was mainly beans and beans products and was negatively associated with hypertension. The prudent pattern only included staple foods and pickled vegetables and was positively associated with hypertension as well as coronary heart disease. The traditional pattern was representative of local Baoji traditional recipes and was positively associated with hypertension.
CONCLUSIONS
The protein, balanced, and beans dietary patterns showed many protective effects on cardio-cerebrovascular disease. Based on these results, Baoji city residents should be encouraged to choose protein, balanced, and beans dietary patterns and abandon prudent and traditional patterns to prevent incidence of hypertension, coronary heart disease, and stroke.
According to a study by the World Health Organization (WHO), cardiovascular disease is responsible for 33.7% of all deaths worldwide, whereas other chronic diseases are responsible for 26.5% [1]. Globally, it has been estimated that premature deaths resulting from hypertension reach approximately 7.1 million annually, which account for 64 million disability-adjusted life years (DALYs) [2]. Hypertension plays a major etiologic role in the development of ischemic heart disease, cerebrovascular disease, and cardiac and renal failure, and it is a significant risk factor for mortality and disability rates throughout the world [3].
Dietary patterns consider the interactions between all kinds of foods and nutrients and represent a broader picture of food and nutrient consumption, suggesting they may be more predictive of disease risk than individual food or nutrients [4]. In addition, dietary patterns have become a focus for nutritional research [5]. Factor analysis of dietary patterns can elucidate the proportions of all types of foods by dimension reduction. Factor loading represents the correlation coefficient between foods and patterns. A positive loading indicates a positive association with the factor while a negative loading indicates a negative association with the factor. Larger loading of a given food item indicates greater contribution of that food item to the specific factor.
Dietary habits in Asians such as Chinese [6] are substantially different from those of Westerners. Therefore, it is important to examine dietary patterns and their associations with non-communicable diseases among people in China. Dietary habits in Northwest China such as Baoji are different from those in other cities. Further, dietary patterns and their associations with hypertension, coronary heart disease, stroke, and other chronic diseases have not been studied in Baoji, which is a representative city of western China.
The present study surveyed the dietary and health status of residents over 15 years old in Baoji, identified dietary patterns among Chinese adults, and determined whether or not these dietary patterns are associated with chronic diseases (e.g. hypertension, coronary heart disease, stroke) in order to provide recommendations for improving food intakes.
We designed "The epidemiology questionnaire of Non Communicable Diseases and related risk factors in Baoji city" based on health interviews focused on dietary patterns, family background, body measurement, etc. according to the 2010 Chinese National Chronic Diseases Survey and the Fifth National Health Service Survey.
This study was based on a population sampling survey according to the Handbook of Baoji city of Shaanxi Province in China using multistage stratified random sampling from the total Baoji population and the Kish Grid method, which was organized by the Baoji City Health Bureau and performed by the Baoji CDC. Inclusion criteria were as follows: age over 15 years, residence in Baoji city for more than 6 months, participated in the study voluntarily, and actively completed the questionnaire and measurement. Exclusion criteria were as follows: age less than 15 years and non-residents. A total of 5,020 participants were included in this study from 12 counties, resulting in 4,968 valid samples. Men numbered 2,519 (50.7%), women numbered 2,449 (49.3%), mean age (standard deviation) was 41.6 (16.3) years, and urban and rural percentages were 36.7% and 63.3%, respectively. The composition of the study population was in accordance with the 2010 Baoji city population.
The questionnaire and anthropometric survey were carried out by well-trained medical examiners. The field investigation was conducted in April 2013. Pre-survey was arranged in each county before the formal investigation using unified survey methods. Height, weight, waist circumference, and blood pressure were obtained using standardized techniques and equipment in an early morning fasting state. Height was measured to the nearest 0.1 cm with subjects standing without shoes. Weight in light clothes was measured to the nearest 0.1 kg. Body mass index (BMI) was calculated as weight divided by the square of height (kg/m2). Blood pressure was measured in a sitting position. Three measurements were made on all subjects at 5-min intervals, and the average of three measurement was used in the analysis. All subjects in the survey participated voluntarily, and written informed consent was obtained from all subjects. All aspects of design, train, sample, field investigation, data entry, and checks were subjected to quality control.
We investigated dietary consumption frequency and quantity over the past year using a semi-quantitative food frequency questionnaire. Amount of each nutrient was converted into grams per person per day using nutrition calculator software and finally merged into daily nutrient consumption per person. Dietary questionnaire contained questions on edible oil, spices, and 27 types of food. For dietary patterns, similar foods were consolidated as follows: fresh milk, milk powder, and yogurt into milk; pickles, pickled cabbage, and sauerkraut into pickled vegetables; fruit juice drinks and other beverages into beverages. Daily intakes of 22 kinds of food were obtained.
According to the "Chinese guidelines for prevention and treatment of hypertension (2010 Edition)", hypertension is defined as a systolic blood pressure ≥ 140 mmHg or diastolic blood pressure ≥ 90 mmHg. Information on chronic diseases was collected by a self-reported questionnaire. Coronary heart disease generally refers to coronary atherosclerotic cardiopathy, which can be divided into five clinical types according to the WHO: asymptomatic myocardial ischemia (latent coronary heart disease), ischemic heart failure, angina, myocardial infarction (ischemic heart disease), and sudden death. Stroke, also referred to as cerebral vascular accident, is divided into ischemic stroke and hemorrhagic stroke.
Epidata 3.1 was used to double input data, and database was analyzed with SPSS17.0 software after checks. Measurement data were analyzed by mean ± standard deviation, t test, chi-square test, and ANOVA statistical test, and all analyses were performed at a significance level of P < 0.05. Principal component factor analysis was used to identify dietary patterns. Factors were rotated by varimax orthogonal transformation in order to achieve a simpler structure with greater interpretability [7]. Factor number was selected as follows: 1. eigenvalue > 1.0; 2. plot showing main distribution; 3. proportion of variance explained by each factor but only as a reference; 4. probability of factor extraction.
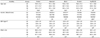
Factor analysis of the Kaiser-Meyer-Olkin measurement was 0.803. Bartlett test of spherical showed P < 0.001. Factor analysis extracted five dietary patterns with eigenvalues all larger than 1.0. The five factors of the cumulative variance contribution rate reached 41.124%, as shown in Table 1.
Factor loadings higher than 0.20 (absolute value) were analyzed, and factors were named according to foods contained in the dietary pattern: protein, balanced, beans, prudent, and traditional dietary pattern (Table 2). Factor 1 was characterized as high positive loadings of fried pasta, beef and mutton, poultry, organ meat, seafood, dried tofu, seaweed, pickled vegetables, pastry, and beverages. Factor 2 showed high positive loadings of rice, fried pasta, pork, dairy, eggs, soybean milk, fresh vegetables, pastry, fresh fruits, and beverages. Factor 3 showed high positive loadings of dried tofu, soybean milk, dry beans, seaweed, and fresh fruits. Factor 4 showed high positive loadings of whole grains, potatoes, fried pasta, and pickled vegetables. Factor 5 showed high positive loadings of wheat, whole grains, fried pasta, pork, fresh vegetables, and pickled vegetables.
Each factor was divided into Q1 (low percentile), Q2 (middle percentile), or Q3 (high percentile) by score. A higher score indicates greater association with a particular dietary pattern. Research has suggested that dietary patterns are related to demographic characteristics, lifestyles, and movement of populations [8]. The demography and body indices of dietary patterns across percentiles are shown in Table 3. Average ages of the protein, balanced, and beans dietary patterns in Q3 were younger than in Q1. Average age of the prudent dietary pattern in Q3 was older than in Q1. Traditional dietary pattern and BMI of each pattern showed no significant difference. Waist circumferences of the protein, balanced, and beans dietary patterns in Q3 were longer than in Q1. Prudent and traditional dietary patterns showed no significant difference. Protein and beans patterns in Q3 had more females than males, whereas prudent and traditional patterns in Q3 had more males than females. Balanced pattern showed no difference in gender.
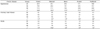
Table 4 shows seven chronic diseases according to dietary pattern.
The prevalence rates of hypertension among the protein, balanced, and beans patterns were significantly lower in Q3 than in Q1, whereas prevalence rates of hypertension among prudent and traditional patterns were higher in Q3 than in Q1.
The prevalence rate of coronary heart disease among the prudent pattern was higher in Q3 than in Q1. The other four patterns showed no significant difference.
The prevalence rate of stroke among the protein and balanced patterns were lower in Q3 than in Q1. The other three patterns showed no significant difference.
At present, there has been little research into the association between dietary nutrition and chronic diseases among Baoji city residents living in Shaanxi Province, northwest China. In this study, we investigated the relationship between nutrient intakes, dietary patterns, and cardio-cerebrovascular disease to provide baseline data for nutritional intervention.
In this study, five dietary patterns were identified by factor analysis in a Chinese adult population: protein, balanced, beans, prudent, and traditional patterns. Factor loadings higher than 0.20 (absolute value) were analyzed. Factor 1 mainly included animal protein and plant protein. Factor 2 included carbohydrates, protein, and fat. Factor 3 included beans and bean products. Factor 4 included staple foods and pickled vegetables. Factor 5 included Baoji local traditional recipes. Contribution rates were 16.1%, 7.9%, 7.0%, 5.2%, and 5.0%, respectively, reaching 41.1% of the accumulative variance contribution rate. This rate is high compared to other dietary studies that found a cumulative contribution rate of 30% or less [9,10]. In addition to factor analysis, other methods were used to identify dietary patterns (e.g., Reduced rank regression, RRR) [11]. RRR provides linear functions of predictor variables that explain as much of the variation in response variables as possible, whereas factor analysis derives dietary patterns by maximizing the explained variation among all predictor variables [12].
Demography and body indices analysis by dietary pattern showed that ages of the protein, balanced, and beans dietary patterns were younger, whereas age of the prudent pattern was older. There were more females in the protein and beans patterns, whereas males were more prominent in the prudent and traditional patterns. This indicates that young people preferred the protein, balanced, and beans dietary patterns, whereas old people preferred the prudent pattern. There are two types of obesity, general obesity based on BMI and abdominal obesity (also known as central obesity) based on waist circumference. In this study, BMI of each pattern was not significantly different, whereas waist circumference was longer in the protein, balanced, and beans patterns. This result suggests that dietary factors more easily lead to abdominal obesity than general obesity.
The protein, balanced, and beans patterns were associated with reduced prevalence of hypertension. The protein and balanced patterns were associated with reduced prevalence of stroke, whereas the prudent and traditional patterns were associated with increased prevalence of hypertension. The prudent pattern was associated with increased prevalence of coronary heart disease.
Prior studies have investigated correlations between dietary patterns and hypertension, cardiovascular disease, stroke, and cancer [13,14]. Previous studies investigating dietary patterns and their associations with chronic diseases have been reported from the USA [15,16,17], Canada [18], Germany [19], Portugal [20], Iran [21], and other Asian countries [22,23,24]. These studies have found that dietary patterns characterized by high intakes of vegetables, fruits, and fish are inversely associated with diseases, whereas dietary patterns characterized by high intakes of red meat, processed meat, refined grains, and fried foods are associated with increased risk.
Our results are comparable to those of previous studies. The balanced dietary pattern in the present study is resembles the healthy dietary pattern identified in Western countries, which is characterized by comprehensive intakes of protein, carbohydrates, and fat. A systematic review study indicated that fruit and vegetable concentrates are effective in significantly improving circulating concentrations of antioxidant vitamins, provitamins, and folate as well as decreasing markers of oxidative stress [25], which has been associated with reduced risk of chronic diseases [26]. High intakes of fruits, vegetables, cereals, fishes, nuts, low-fat dairy products, and poultry in addition to relatively low intakes of fat and sugars appear to be effective in lowering blood pressures and hypertension [27]. Dietary patterns characterized by frequent intakes of fruits and dairy products have been shown to significantly decrease blood pressure among Chinese [28]. The Dietary Approaches to Stop Hypertension (DASH) dietary pattern, which is rich in fruits, vegetables, and low-fat dairy products and low in saturated fat, red meat, and sweets, is successful in controlling hypertension [29]. On the other hand, increased consumption of a Western dietary pattern is typically associated with higher prevalence of chronic diseases such as coronary heart diseases [30]. Western dietary patterns with high intakes of red and processed meats, butter, oils, fats, sweets and desserts, refined grains, and high-fat dairy are associated with significantly increased risk of cardiovascular disease [31]. Hu reported that Western dietary pattern score is positively associated with fat intake percentage as well as prevalence of coronary heart disease [32]. A cohort study in Japan also demonstrated that dietary patterns with high meat intakes are closely related to increased risk of cardiovascular diseases [33]. In this study, although we did not identify Western dietary patterns, the prudent pattern rich in whole grains, potatoes, fried pasta, and pickled vegetables was positively associated with prevalence of coronary heart disease. The Baoji traditional dietary pattern rich in whole grains, fried pasta, and vegetables did not show any protective effect against chronic diseases, which corroborates a Korean study [34].
This study has several limitations. Firstly, confounding factors could not be avoided, although we used multistage stratified random sampling. Secondly, there was some potential recall and reporting biases in the semi-quantitative food frequency questionnaire. Future prospective cohort and clinical trials are warranted to verify our findings.
In conclusion, five major dietary patterns were identified by factor analysis and were associated with prevalence of chronic diseases among Chinese adults. The protein dietary pattern was negatively associated with hypertension and stroke, the balanced pattern was negatively associated with hypertension and stroke, the beans pattern was negatively associated with hypertension, the prudent pattern was positively associated with hypertension and coronary heart disease, and the traditional pattern was positively associated with hypertension. In the future, these results should be confirmed by prospective cohort and clinical trials. On the whole, we should encourage Baoji city residents to choose protein, balanced, and beans dietary patterns and abandon prudent and traditional patterns to prevent incidence of hypertension, coronary heart disease, stroke, and other chronic diseases.
ACKNOWLEDGMENTS
We thank the study participants for their contribution to the research. We also thank the guidance of Xi'an Jiao Tong University in research design, and the the strong support and help of Health Bureau and CDC of Baoji City and 12 counties to process in the field survey.
References
1. Gaziano TA, Bitton A, Anand S, Abrahams-Gessel S, Murphy A. Growing epidemic of coronary heart disease in low- and middle-income countries. Curr Probl Cardiol. 2010; 35:72–115.

2. Whitworth JA. World Health Organization, International Society of Hypertension Writing Group. 2003 World Health Organization (WHO)/International Society of Hypertension (ISH) statement on management of hypertension. J Hypertens. 2003; 21:1983–1992.

3. Chockalingam A, Campbell NR, Fodor JG. Worldwide epidemic of hypertension. Can J Cardiol. 2006; 22:553–555.

4. Newby PK, Tucker KL. Empirically derived eating patterns using factor or cluster analysis: a review. Nutr Rev. 2004; 62:177–203.

6. Wang D, He Y, Li Y, Luan D, Yang X, Zhai F, Ma G. Dietary patterns and hypertension among Chinese adults: a nationally representative cross-sectional study. BMC Public Health. 2011; 11:925.

7. Rezazadeh A, Rashidkhani B, Omidvar N. Association of major dietary patterns with socioeconomic and lifestyle factors of adult women living in Tehran, Iran. Nutrition. 2010; 26:337–341.

8. Zhang L, Shi ZF, Chi AL, Zhao ZT. Effects of 11 years' community intervention on hypertension, diabetes and KAP of the diseases among urban residents. Chin J Public Health. 2013; 29:608–611.
9. Luo Y, Chen X, Zuo G, Yuan N. Association between hypertension and dietary patterns in residents of Jiangyin city. Chin J Public Health. 2009; 25:314–316.
10. Shang X, Li Y, Liu A, Zhang Q, Hu X, Du S, Ma J, Xu G, Li Y, Guo H, Du L, Ma G. Dietary pattern and its association with the prevalence of obesity and related cardiometabolic risk factors among Chinese children. PLoS One. 2012; 7:e43183.

11. Song SJ, Lee JE, Paik HY, Park MS, Song YJ. Dietary patterns based on carbohydrate nutrition are associated with the risk for diabetes and dyslipidemia. Nutr Res Pract. 2012; 6:349–356.

12. Hoffmann K, Schulze MB, Schienkiewitz A, Nöthlings U, Boeing H. Application of a new statistical method to derive dietary patterns in nutritional epidemiology. Am J Epidemiol. 2004; 159:935–944.

13. Foroughi M, Akhavanzanjani M, Maghsoudi Z, Ghiasvand R, Khorvash F, Askari G. Stroke and nutrition: a review of studies. Int J Prev Med. 2013; 4:S165–S179.
14. Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008; 118:230–237.

15. Lutsey PL, Steffen LM, Stevens J. Dietary intake and the development of the metabolic syndrome: the Atherosclerosis Risk in Communities study. Circulation. 2008; 117:754–761.

16. Deshmukh-Taskar PR, O'Neil CE, Nicklas TA, Yang SJ, Liu Y, Gustat J, Berenson GS. Dietary patterns associated with metabolic syndrome, sociodemographic and lifestyle factors in young adults: the Bogalusa Heart Study. Public Health Nutr. 2009; 12:2493–2503.

17. Fialkowski MK, McCrory MA, Roberts SM, Tracy JK, Grattan LM, Boushey CJ. Dietary patterns are associated with dietary recommendations but have limited relationship to BMI in the Communities Advancing the Studies of Tribal Nations Across the Lifespan (CoASTAL) cohort. Public Health Nutr. 2012; 15:1948–1958.

18. Langsetmo L, Poliquin S, Hanley DA, Prior JC, Barr S, Anastassiades T, Towheed T, Goltzman D, Kreiger N. CaMos Research Group. Dietary patterns in Canadian men and women ages 25 and older: relationship to demographics, body mass index, and bone mineral density. BMC Musculoskelet Disord. 2010; 11:20.

19. Heidemann C, Scheidt-Nave C, Richter A, Mensink GB. Dietary patterns are associated with cardiometabolic risk factors in a representative study population of German adults. Br J Nutr. 2011; 106:1253–1262.

20. Fonseca MJ, Gaio R, Lopes C, Santos AC. Association between dietary patterns and metabolic syndrome in a sample of Portuguese adults. Nutr J. 2012; 11:64.

21. Khosravi-Boroujeni H, Sarrafzadegan N, Mohammadifard N, Sajjadi F, Maghroun M, Asgari S, Rafieian-Kopaei M, Azadbakht L. White rice consumption and CVD risk factors among Iranian population. J Health Popul Nutr. 2013; 31:252–261.

22. Shin JY, Kim JM, Kim Y. Associations between dietary patterns and hypertension among Korean adults: the Korean National Health and Nutrition Examination Survey (2008-2010). Nutr Res Pract. 2013; 7:224–232.

23. Akter S, Nanri A, Pham NM, Kurotani K, Mizoue T. Dietary patterns and metabolic syndrome in a Japanese working population. Nutr Metab (Lond). 2013; 10:30.

24. Daniel CR, Prabhakaran D, Kapur K, Graubard BI, Devasenapathy N, Ramakrishnan L, George PS, Shetty H, Ferrucci LM, Yurgalevitch S, Chatterjee N, Reddy KS, Rastogi T, Gupta PC, Mathew A, Sinha R. A cross-sectional investigation of regional patterns of diet and cardio-metabolic risk in India. Nutr J. 2011; 10:12.

25. Esfahani A, Wong JM, Truan J, Villa CR, Mirrahimi A, Srichaikul K, Kendall CW. Health effects of mixed fruit and vegetable concentrates: a systematic review of the clinical interventions. J Am Coll Nutr. 2011; 30:285–294.

26. Hung HC, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Colditz GA, Rosner B, Spiegelman D, Willett WC. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004; 96:1577–1584.

27. Appel LJ, Moore TJ, Obarzanek E, Vollmer WM, Svetkey LP, Sacks FM, Bray GA, Vogt TM, Cutler JA, Windhauser MM, Lin PH, Karanja N. A clinical trial of the effects of dietary patterns on blood pressure. DASH Collaborative Research Group. N Engl J Med. 1997; 336:1117–1124.

28. Lee SA, Cai H, Yang G, Xu WH, Zheng W, Li H, Gao YT, Xiang YB, Shu XO. Dietary patterns and blood pressure among middle-aged and elderly Chinese men in Shanghai. Br J Nutr. 2010; 104:265–275.

29. Bhupathiraju SN, Tucker KL. Coronary heart disease prevention: nutrients, foods, and dietary patterns. Clin Chim Acta. 2011; 412:1493–1514.

30. Hu FB, Rimm EB, Stampfer MJ, Ascherio A, Spiegelman D, Willett WC. Prospective study of major dietary patterns and risk of coronary heart disease in men. Am J Clin Nutr. 2000; 72:912–921.

31. Berg CM, Lappas G, Strandhagen E, Wolk A, Torén K, Rosengren A, Aires N, Thelle DS, Lissner L. Food patterns and cardiovascular disease risk factors: the Swedish INTERGENE research program. Am J Clin Nutr. 2008; 88:289–297.

32. Hu FB. Dietary pattern analysis: a new direction in nutritional epidemiology. Curr Opin Lipidol. 2002; 13:3–9.





 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download