Abstract
BACKGROUND/OBJECTIVES
Vitamin D deficiency is common in hemodialysis patients. The aim of this study was to identify whether or not sun exposure and dietary vitamin D intake have effects on serum 25-hydroxyvitamin D (25(OH)D) status in hemodialysis (HD) patients. The objective was to identify the main determinants of serum vitamin D status in the study subjects.
SUBJECTS/METHODS
A cross-sectional study of 47 HD patients (19 males and 28 females) was performed. We assessed serum 25(OH)D and 1,25(OH)2D levels between August and September 2012 and analyzed the prevalence of vitamin D deficiency in HD patients. To evaluate the determinants of serum 25(OH)D levels, we surveyed dietary vitamin D intake, degree of sun exposure, and outdoor activities. To compare biological variables, serum 25(OH)D was stratified as below 15 ng/ml or above 15 ng/ml.
RESULTS
Mean 25(OH)D and 1,25(OH)2D levels were 13.5 ± 5.8 ng/ml and 20.6 ± 11.8 pg/ml, respectively. The proportions of serum 25(OH)D deficiency (< 15 ng/ml), insufficiency (15-< 30 ng/ml), and sufficiency (≥ 30 ng/ml) in subjects were 72.4%, 23.4%, and 4.3%, respectively. Prevalence of vitamin D deficiency in female patients was 78.6%, whereas that in males was 63.2% (P = 0.046). Vitamin D intake and sun exposure time were not significantly different between the two stratified serum 25(OH)D levels. Dietary intake of vitamin D did not contribute to increased serum 25(OH)D levels in HD patients. The main effective factors affecting serum 25(OH)D status were found to be the sun exposure and active outdoor exercise.
Vitamin D deficiency is common in all stages of chronic kidney disease (CKD), especially in hemodialysis (HD) patients. A recent study on CKD patients in Korea showed that hypovitaminosis D is prevalent even in early stages of CKD, and prevalence of vitamin D deficiency increases up to 92.8% in stage 5 CKD [eGFR < 15 (ml/min/1,73 m2)] in the winter [1]. Reasonable mechanisms for the high prevalence of vitamin D deficiency in the CKD population have been reported [2,3,4,5,6,7,8,9]. Renal megalin is an endocytic receptor that is induced by active vitamin D and the vitamin D receptor (VDR) complex [3], and its levels are reduced in patients with renal disease, losing large amounts of vitamin D and vitamin D binding protein in their urine. Therefore, vitamin D deficiency is caused by decreased megalin levels, resulting in inhibition of both 25-hydroxyvitamin D (25(OH)D) uptake and active vitamin D production [4]. Another mechanism explaining vitamin D deficiency in CKD patients is elevated levels of fibroblast growth factor 23 (FGF-23), which induces degradation of 1,25-dihydroxyvitamin D (1,25(OH)2D) [2,3,4,5,6]. Other mechanisms of hypovitaminosis D in CKD may involve reduced activity of renal 1α-hydroxylase in response to uremic toxin [7], poor dietary vitamin D intake, and inadequate sun exposure [8,9].
Vitamin D is an essential nutrient due to both its classical effects on the skeletal system as well as its extra-skeletal benefits, which include lowered blood pressure, reduction of inflammatory biomarkers, improved insulin sensitivity [10], and elevated immune function via regulation of innate and adaptive immunity [11]. Moreover, higher levels of circulating 25(OH)D are associated with lower mortality risk in CKD patients [12,13,14]. In support of this, another study reported a connection between lower plasma 1,25(OH)2D concentrations and increased mortality in advanced CKD patients [15]. In this regard, guidelines for management of CKD-related bone and mineral disorders should emphasize treatment of hypovitaminosis D. National Kidney Foundation guidelines state that optimal 25(OH)D levels are higher than 30 ng/ml [16]. Guidelines suggest that an active vitamin D sterol such as calcitriol, alfacalcidol, or paricalcitol should be administered to dialysis patients with serum PTH levels greater than 300 pg/ml [16]. However, active vitamin D sterols may induce side effects such as elevated levels of serum phosphorus and calcium. Therefore, recent studies have investigated the effects of dietary vitamin D intake and sun exposure or cholecalciferol (vitamin D3) supplementation on serum 25(OH)D levels [17,18,19].
HD patients are prescribed to avoid foods such as fish, dairy products (milk, yogurt, and cheese), and eggs, all of which contain vitamin D and phosphorus. Dietary surveys have shown that HD patients consume less vitamin D than recommended daily allowances and specifically avoid foods containing vitamin D or phosphorus [8]. One study concluded that dialysis restrictions imposed to reduce dietary phosphorus intake likely contribute to the development of hypovitaminosis D in end-stage renal disease (ESRD) patients. Further, sun exposure has been reported to be an effective inducer of serum 25(OH)D levels in CKD and HD patients. A seasonal study reported that vitamin D deficiency among HD patients was higher in winter (86%) compared to summer (54%) [20]. In another study on Korean HD patients, the prevalence of 25(OH)D deficiency was 86.2% at the end of summer and increased to 96.2% by the end of winter, and mean concentrations of 25(OH)D and 1,25(OH)2D were significantly reduced in winter compared to summer [21]. Thus, sun exposure is a main determinant of serum 25(OH)D and 1,25(OH)2D levels.
In this study, we evaluated the prevalence of vitamin D deficiency in HD patients, investigated the effects of sun exposure and dietary vitamin D intake on serum 25(OH)D status, and identifies main determinants of serum vitamin D status in our study subjects.
The subjects of this study were 50 hemodialysis (HD) patients undergoing maintenance HD treatment three times weekly at an artificial kidney center at Hanyang University Seoul Hospital between August and September 2012. The inclusion criteria were as follows: (1) patients had been on HD for more than 3 months, (2) patients were over 19-years-old, (3) patients did not have cancer and showed no active inflammation or infection; (4) patients did not have renal osteodystrophy; (5) patients did not have active hepatitis or any other active liver disease. One patient dropped out due to hospitalization at another hospital while two refused to answer the questionnaire. A total 47 HD patients (19 males and 28 females) completed the questionnaire. All participants gave written informed consent, which was approved by the Institutional Review Board of Hanyang University Hospital (HYUH IRB 2012-06-023).
Blood pressure was evaluated prior to mid-week HD sessions for 1 month before blood biochemical sampling, and four results were averaged. Pre-dialysis blood pressure was measured by automated monitors (Fresenius Medical Care AG & Co, Bad Homburg, Germany). Blood samples were obtained at predialysis for this study. Serum 25(OH)D levels were determined using a chemiluminescent immunoassay (Liaison 25 OH vitamin D Total Assay, Liaison, USA); serum 1,25(OH)2D levels were determined using a radioimmunoassay (1,25 dihydroxyvitamin D RIA-CT, Liaison, USA); intact parathyroid hormone (iPTH) was determined using an electro-chemiluminesent immunoassay (PTH, Roche, Germany); high-sensitivity C-reactive protein (hs-CRP) was determined using immunoturbidmetry (CRPH, Beckman coulter, USA). In order to compare serum 25(OH)D levels by gender, we defined vitamin D insufficiency and deficiency according to the Kidney Disease Outcome Quality Initiative (K/DOQI) guidelines from the National Kidney Foundation [16]. Vitamin D status was considered adequate (≥ 30 ng/ml), insufficient (15-< 30 ng/ml), or deficient (≤ 15 ng/ml). Vitamin D deficiency was further subdivided into moderate (10-≤ 15 ng/ml) or severe (< 10 ng/ml). Biological variables were assessed according to serum 25(OH)D level (15 ng/ml), which is a criterion of deficiency and insufficiency in the K/DOQI guidelines. Serum creatinine, albumin, blood urea nitrogen (BUN), alkaline phosphatase (ALP), calcium, and phosphorus were measured by standard laboratory methods.
Body mass index (BMI, kg/m2) was calculated using dry weight and height. Age, duration of hemodialysis, main causes of kidney disease, and types and dosages of medication were investigated from medical records at the beginning of the study. Subjects answered questionnaires about sun exposure (sunscreen usage, time of outdoor activity, and frequency of outdoor activity per week), physical activity, supplement usage, smoking habits, and alcohol consumption. Active outdoor exercisers were categorized into two groups, "yes" or "no", according to the following questions: "Do you exercise outdoors?", "Do you exercise outdoors more than 3 times per week?", "Do you exercise more than 30 minutes to 1 hour outdoors?", "Do you use sun protection during outdoor exercise or when leaving the house?", and "Do you usually wear a hat, long sleeves, or long pants when you participate in outdoor activities?"
Dietary vitamin D and calcium intakes were collected by using 24-hour recall and 2-day food diaries. Dietary data for the first day were assessed by a dietitian using 24-hour recall with plastic food models, whereas data for the second and third days were completed using 2-day food diaries. Subjects were given a scale for weighing foods. Average daily vitamin D and calcium intakes were calculated using Can-pro 4.0 (Computer Aided Nutritional Analysis Program 4.0, The Korean Nutrition Society, Korea). Subjects answered a 37-item modified food frequency questionnaire (FFQ) that was primarily derived from a 63-item FFQ developed from the Korean National Health and Nutrition Examination Surveys (KNHANES IV). The FFQ for this study was modified to estimate vitamin D intake and consumption frequencies across nine categories (almost never, 1 time/mo, 2-3 times/mo, 1 time/wk, 2-4 times/wk, 5-6 times/wk, 1 time/d, 2 times/d, and 3 times/d). The FFQ also included three categories for intake amount (1/2 serving size, 1 serving size, or 1 and 1/2 serving size). To analyze the association between serum 25(OH)D level and major vitamin D food sources, three food groups were selected based on previous studies [22] as follows: total fish (50 g/serving), including anchovy, tuna, croaker, codfish, hairtail, mackerel, and salmon; eggs (50 g/serving); and milk (200 ml/serving). All consumption frequencies were standardized into servings per week.
The study subjects were asked to take self-selected dietary supplements containing calcium and vitamin D as well as other dietary supplements such as vitamin C, omega-3, and red ginseng. Daily intake and frequency per week were recorded. Prescribed amounts of vitamin D and calcium derived from patients' medical records were collected. An active vitamin D analogue, paricalcitol (Zemplar), and a calcium supplement as a phosphate-binder (Phoslo, calcium acetate 710 mg) were used.
Comparison between males and females was carried out by independent t-test for continuous variables, and chi-square test was performed for categorical variables. For comparison of serum 25(OH)D levels, subjects were divided into two groups by serum 25(OH)D concentration, deficiency (< 15 ng/ml) and non-deficiency (≥ 15 ng/ml). Biological variables according to serum 25(OH)D level were assessed through ANCOVA adjusted for age, gender, and HD duration. To assess determinants of serum 25(OH)D concentration, simple and multiple linear regression analyses were conducted to describe the relationship between serum 25(OH)D level and possible explanatory variables. Continuous variables were dietary vitamin D intake (µg/day) and sun exposure time (h/week). Categorical variables were total fish (< 2 or ≥ 2 servings/week), milk (< 200 ml or ≥ 200 ml/week), eggs (< 150 g or ≥ 150 g/week), sun exposure (< 6 h or ≥ 6 h/week), active outdoor exercise (yes or no), sunscreen use (yes or no), gender (male or female), and BMI (< 23 or ≥ 23 kg/m2). To analyze the relationships between sun exposure or vitamin D intake and serum 25(OH)D levels, sun exposure time was set to 6 h/wk (mean value of the subjects) as a criterion for categorical variables, whereas vitamin D intake was set to 2 µg/day (median value of the subjects). Statistical analyses were conducted using PASW Statistics Version 18.0 (IBM Inc).
The general characteristics of the 47 hemodialysis (HD) patients (19 males and 28 females) are shown in Table 1. The mean age was 57.4 ± 11.7 years, mean body mass index (BMI) was 22.1 ± 3.0 kg/m2, and mean HD duration was 8.0 ± 7.4 years. The mean systolic blood pressure (SBP) and diastolic blood pressure (DBP) were 143.5 ± 16.8 mmHg and 71.3 ± 9.2 mmHg, respectively. The main causes of HD were hypertensive nephrosclerosis (17.0%), diabetic nephropathy (34.1%), chronic glomerulonephritis (8.5%), and others (40.4%). Eight patients (17.0%) had used a vitamin D analogue (paricalcitol, Zemplar), 36 (76.6%) had taken a calcium-based phosphate-binder (calcium acetate, Phoslo), and 44 (93.6%) had taken a multi-vitamin (vitamin B and C complex, Renalmin) in the previous 3 months.
Serum 25(OH)D and 1,25(OH)2D concentrations of males and females are shown in Table 2. Mean 25(OH)D and 1,25(OH)2D levels were 13.5 ± 5.8 ng/ml and 20.6 ± 11.8 pg/ml, respectively. Only two patients (4.3%) showed sufficient vitamin D levels [25(OH)D ≥ 30 ng/ml], whereas 13 patients (27.7%) showed severe vitamin D deficiency [25(OH)D < 10 ng/ml]. Prevalence of vitamin D deficiency [25(OH)D < 15 ng/ml] in female patients was 78.6% (n = 22), whereas prevalence in males was 63.2% (n = 12). Distribution of serum 25(OH)D status was significantly different according to gender (P = 0.046). Serum albumin levels were significantly lower in females (P = 0.013) compared to males, whereas alkaline phosphatase levels were significantly higher in females (P = 0.041). Average dietary intake of vitamin D was 3.25 µg/day for males and 2.47 µg/day for females. Sun exposure time per week was 8.91 h for males and 5.40 h for females. Dietary vitamin D intake and sun exposure time were higher in males compared to females, although there were no significant differences.
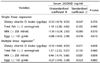
Biological variables according to serum 25(OH)D levels are shown in Table 3. To compare biochemical variables according to serum 25(OH)D levels, we divided them into two vitamin D subgroups: deficient (< 15 ng/ml) and non-deficient (≥ 15 ng/ml). Concentrations of 1,25(OH)2D in the non-deficient group were significantly higher compared to the deficient group (P < 0.001). However, iPTH and other biological variables were not significantly different between the two groups after adjusting for age, gender, and HD duration. Dietary vitamin D intake and sun exposure were also not significantly different between the non-deficient and deficient groups. Paricalcitol (Zemplar), a vitamin D analogue, was prescribed to all eight patients, and seven patients were in the deficient 25(OH)D group over the previous 3 months. Paricalcitol did not increase serum 25(OH)D levels. In terms of physical activity, regular exercise was classified as those who exercise for ≥ 30 min at least three times per week. Active outdoor exercise was classified as one who exercises outside regularly. The proportion of regular exercise was not significantly different between the two groups, whereas the proportion of active outdoor exercise in the non-deficient group (≥ 15 ng/ml) was significantly higher than that in the deficient group (< 15 ng/ml) (P = 0.022).
To evaluate the main determinants of serum 25(OH)D concentration, we analyzed dietary and sun exposure factors affecting serum 25(OH)D concentrations in HD patients by simple and multiple linear regression analyses (Tables 4 and 5). Dietary factors in the analysis were daily vitamin D intake as a continuous variable and major dietary sources of vitamin D (total fish, ≥ 2 servings/wk; milk, ≥ 200 ml/wk; eggs, ≥ 150 g/wk) as categorical variables. The results of the multiple linear regression model were adjusted for BMI and gender. Dietary intake of vitamin D and food sources did not increase serum 25(OH)D levels in HD patients. We also evaluated other determinants, including sun exposure time as a continuous variable and categorical variable (1: ≥ 6 h/wk, 0: < 6 h/wk), active outdoor exercise (1: yes, 0: no), and sunscreen use (1: yes, 0: no). From the simple linear regression analysis, the most important relative effects on serum 25(OH)D status were time of sun exposure and active outdoor exercise. Serum 25(OH)D level increased by 0.27 ng/ml for every 1 h of sun exposure per day and increased by 4.12 ng/ml for every 6 h per week. Active outdoor exercise longer than 30 min at least three times per week was another important relative determinant of serum 25(OH)D status. Specifically, serum 25(OH)D levels increased by 5.21 ng/ml for outdoor exercisers. To assess the association between sun exposure or dietary vitamin D intake and serum 25(OH)D status, dietary factors such as daily vitamin D intake and fish intake were applied to a multiple linear regression model. The results for sun exposure and dietary factors with serum 25(OH)D concentration were adjusted for BMI and gender. Sun exposure time and active outdoor exercise did not increase serum 25(OH)D levels in the multiple linear regression model. Sunscreen use was not significantly associated with serum 25(OH)D status in the simple linear model.
Vitamin D deficiency and insufficiency were observed in most of the HD patients, and female patients showed lower levels. Further, vitamin D deficiency [25(OH)D < 15 ng/ml] was observed in 72.4% of HD patients. In addition, mean 25(OH)D and 1,25(OH)2D levels were 13.5 ± 5.8 ng/ml and 20.6 ± 11.8 pg/ml, respectively, which are similar to results of previous studies in Korea [1,21,23]. Dietary intake of vitamin D was 3.25 ± 3.38 µg/day in males and 2.47 ± 2.09 µg/day in females. Dietary vitamin D intake and sun exposure were not significantly different between deficient (< 15 ng/ml) and non-deficient (≥ 15 ng/ml) groups. Sun exposure and active outdoor exercise were determined to be important factors affecting serum 25(OH)D levels in the simple linear regression model.
Vitamin D deficiency is very common in dialysis populations, even in populations that receive relatively high levels of sunlight [24,25]. Reasonable mechanisms for this could involve defective renal function, reduced delivery of 25(OH)D to kidneys, decreased expression of renal megalin, and increased excretion of vitamin D-binding protein (VDBP) and fibroblast growth factor 23 (FGF-23) expression. Renal megalin induced by active vitamin D responds to renal tubular reabsorption of albumin and VDBP [2,3]. Therefore, reduced megalin expression resulting from lowered circulating 25(OH)D levels may explain the vitamin D deficiency in these CKD patients [4]. Another main determinant of low vitamin D status in CKD patients could be elevated expression of FGF-23, which is stimulated by excess phosphorus [5]. FGF-23 has been shown to directly suppress the activity and expression of 1α-hydroxylase as well as induce expression of 24-hydroxylase, which catalyzes degradation of 1,25(OH)2D. Thus, elevated expression of FGF-23 may contribute to reduced production of 1,25(OH)2D in CKD [6]. For this reason, circulating 25(OH)D and 1,25(OH)2D levels are decreased in HD and CKD patients. In addition, risk factors for hypovitaminosis D in CKD patients are reportedly related to reduced sunlight exposure, female gender, and increased BMI [24,26]. Moreover, HD patients are limited in terms of their dietary vitamin D food sources due to consideration of serum phosphate level, and their lifestyle often involves lack of sun exposure. In our study, sun exposure time and dietary vitamin D intake were typically lower in females compared to males. Vitamin D deficiency was also more frequent in females due to low vitamin D intake and sun exposure, which supports a previous study [26].
Dietary vitamin D intakes were measured using 3-day dietary records. Mean vitamin D intake was 2.78 µg per day, and this amount is very low compared to Korean dietary recommended allowances of vitamin D intake (5 µg/day for 30 to 49-year-olds and 10 µg/day for over 50-year-olds). Data were insufficient to verify dietary vitamin D intake. Recently, Park et al. reported dietary vitamin D intake of 5.71 µg/day in an elderly Korean population [27]. Our study subjects showed lower intakes than this amount. They also avoided intake of vitamin D-rich foods such as fish, milk, yogurt, and eggs, as they have high serum phosphorus levels. Low vitamin D intake was previously observed in American HD patients, who showed a median weekly vitamin D intake of 1044 IU (26 µg/wk) compared to the recommended weekly allowance of 4200 IU (105 µg/wk) and specific avoidance of foods containing both vitamin D and phosphorus [8]. Burgaz et al. [28] investigated the relationship between 25(OH)D levels, vitamin D intake, and sun exposure in Swedish women. The authors found that 2-3 servings of fatty fish/wk increased serum vitamin D concentrations by 45%. In our simple and multiple linear regression analyses, dietary vitamin D intake and food sources such as fish, milk, and eggs had no significant effects on serum 25(OH)D levels. Therefore, the small amount of habitual dietary vitamin D intake in HD patients had no effect on serum 25(OH)D levels. In support of this, cholecalciferol supplementation in HD patients has been shown to be effective in maintaining optimum 25(OH)D levels [17,18,19].
In the present study, serum 25(OH)D levels were classified as deficient (< 15 ng/ml) or non-deficient (≥ 15 ng/ml) to evaluate biological variables (Table 3). Levels of 1,25(OH)2D and active outdoor exercise (69.2%) were significantly higher in the non-deficient group compared to the deficient group. However, other biological variables such as iPTH and ALP were not significantly different between the two groups. The association between serum 25(OH)D and iPTH levels has been investigated previously [15,29,30]. iPTH is a biological indicator of bone mineral density as well as a cardiovascular risk factor [31,32]. Additionally, increased iPTH and phosphorus levels are risk factors of cardiovascular disease and mortality in HD patients [33,34]. Kestenbaum et al. [35] evaluated the association of 25(OH)D and iPTH levels with mortality both separately as well as in combination with cardiovascular events over 14 years. The study found that 25(OH)D deficiency is associated with myocardial infarction and mortality, whereas excess PTH is associated with hypovitaminosis D and heart failure.
Simple linear regression analysis was performed to identify determinants of serum 25(OH)D levels. Sun exposure time and active outdoor exercise were examined as the effective factors. Serum 25(OH)D levels increased by 0.27 ng/ml for each hour of sun exposure, 4.12 ng/ml with sun exposure time ≥ 6 h/wk, and 5.21 ng/ml with active outdoor exercise ≥ 30 min/day and ≥ 3 times/wk. However, in multiple linear regression with dietary factors, sun exposure time ≥ 6 h/wk and active outdoor exercise ≥ 30 min/day and ≥ 3 times/wk were not effective determinants of serum 25(OH)D levels adjusted for BMI and gender. Sun exposure was reported as an effective determinant of serum 25(OH)D levels in subjects with kidney disease. Seasonal variations in vitamin D levels in end-stage renal disease (ESRD) patients have been observed [20,36]. Serum 25(OH)D levels also show seasonal variations in ESRD patients, with peak levels in autumn or end of summer and lowest levels in spring or end of winter. Farrar et al. [37] examined the effect of sunlight exposure on vitamin D status in south Asian adults over 6 weeks. Participants exposed to 45 min of unshaded sunlight showed increased serum 25(OH)D levels (mean rise: 8.7 ± 5.7 ng/ml). Therefore, sun exposure can be considered to be a main determinant of serum 25(OH)D levels.
Our study has some potential limitations. In particular, a small number of subjects participated in this study. Additionally, our study was conducted at only one artificial kidney center in Seoul. Therefore, we could not enroll the patients with adequate 25(OH)D levels and could not compared biological variables and other determinants between deficient and adequate groups. Moreover, vitamin D intake by subjects was analyzed by the Can-pro 4.0 Nutritional Analysis Program, which was only developed recently. Therefore, more basic data are required to verify dietary vitamin D intakes in Koreans as well as for comparison with HD patients.
We investigated the effects of vitamin D intake and sun exposure on serum 25(OH)D levels in 47 HD patients between August and September (end of summer season) in Korea. We observed vitamin D deficiency (≤ 15 ng/ml) in two-thirds of our subjects, with higher incidence in females. Dietary vitamin D intake and food sources such as fish, milk, and eggs were not significantly correlated with their serum 25(OH)D levels, whereas sun exposure time and active outdoor exercise were effective factors. The results suggest that vitamin D supplements and sufficient sun exposure might contribute to prevention of hypovitaminosis D and maintenance of appropriate serum vitamin D levels in HD patients.
Figures and Tables
Table 3
Biological variables and related factors according to 25(OH)D concentration in hemodialysis patients

Notes: Data are reported as mean ± SD for continuous variables. P-value by ANCOVA between 25(OH)D < 15 and 25(OH)D ≥ 15 after adjusting for age, gender, and hemodialysis duration
1)Three or more times/week and ≥ 30 min/time, 2)Three or more times/week and ≥ 30 min/time outside
Abbreviations: BMI, body mass index; BUN, blood nitrogen urea; ALP, alkaline phosphatase; iPTH, intact parathyroid hormone; hs-CRP, high-sensitivity C-reactive protein
References
1. Lee YM, Park SW, Kim JS, Wang JK, Kim JY, Park MS, Pyo HJ, Kwon YJ. 25-Hydroxyvitamin D status in patients with chronic kidney disease in a single center. Korean J Nephrol. 2010; 29:458–464.
2. Nykjaer A, Dragun D, Walther D, Vorum H, Jacobsen C, Herz J, Melsen F, Christensen EI, Willnow TE. An endocytic pathway essential for renal uptake and activation of the steroid 25-(OH) vitamin D3. Cell. 1999; 96:507–515.

3. Liu W, Yu WR, Carling T, Juhlin C, Rastad J, Ridefelt P, Akerström G, Hellman P. Regulation of gp330/megalin expression by vitamins A and D. Eur J Clin Invest. 1998; 28:100–107.

5. Ramos R, Alcázar R, Otero A, de Francisco AL, del Pino MD. Economic impact of vitamin D treatment on chronic kidney disease patients. Nefrologia. 2011; 31:528–536.
6. Dusso A, González EA, Martin KJ. Vitamin D in chronic kidney disease. Best Pract Res Clin Endocrinol Metab. 2011; 25:647–655.

7. Hsu CH, Patel S. Uremic plasma contains factors inhibiting 1 alpha-hydroxylase activity. J Am Soc Nephrol. 1992; 3:947–952.

8. Krassilnikova M, Ostrow K, Bader A, Heeger P, Mehrotra A. Low dietary intake of vitamin D and vitamin D deficiency in hemodialysis patients. J Nephrol Ther. 2014; 4:pii: 166.

9. Mehrotra R, Kermah D, Budoff M, Salusky IB, Mao SS, Gao YL, Takasu J, Adler S, Norris K. Hypovitaminosis D in chronic kidney disease. Clin J Am Soc Nephrol. 2008; 3:1144–1151.

10. Judd SE, Tangpricha V. Vitamin D therapy and cardiovascular health. Curr Hypertens Rep. 2011; 13:187–191.

11. Sterling KA, Eftekhari P, Girndt M, Kimmel PL, Raj DS. The immunoregulatory function of vitamin D: implications in chronic kidney disease. Nat Rev Nephrol. 2012; 8:403–412.

12. Pilz S, Iodice S, Zittermann A, Grant WB, Gandini S. Vitamin D status and mortality risk in CKD: a meta-analysis of prospective studies. Am J Kidney Dis. 2011; 58:374–382.

13. Duranton F, Rodriguez-Ortiz ME, Duny Y, Rodriguez M, Daurès JP, Argilés A. Vitamin D treatment and mortality in chronic kidney disease: a systematic review and meta-analysis. Am J Nephrol. 2013; 37:239–248.

14. Navaneethan SD, Schold JD, Arrigain S, Jolly SE, Jain A, Schreiber MJ Jr, Simon JF, Srinivas TR, Nally JV Jr. Low 25-hydroxyvitamin D levels and mortality in non-dialysis-dependent CKD. Am J Kidney Dis. 2011; 58:536–543.

15. Kendrick J, Cheung AK, Kaufman JS, Greene T, Roberts WL, Smits G, Chonchol M. HOST (Homocysteinemia in Kidney and End Stage Renal Disease) Study Investigators. Associations of plasma 25-hydroxyvitamin D and 1,25-dihydroxyvitamin D concentrations with death and progression to maintenance dialysis in patients with advanced kidney disease. Am J Kidney Dis. 2012; 60:567–575.

16. National Kidney Foundation. K/DOQI clinical practice guidelines for bone metabolism and disease in chronic kidney disease. Am J Kidney Dis. 2003; 42:S1–S201.
17. Kim SM, Choi HJ, Lee JP, Kim DK, Oh YK, Kim YS, Lim CS. Prevalence of vitamin D deficiency and effects of supplementation with cholecalciferol in patients with chronic kidney disease. J Ren Nutr. 2014; 24:20–25.

18. Descombes E, Fellay B, Hemett OM, Magnin JL, Fellay G. Oral postdialysis cholecalciferol supplementation in patients on maintenance hemodialysis: a dose-response approach. Int J Nephrol. 2014; 2014:597429.

19. Mose FH, Vase H, Larsen T, Kancir AS, Kosierkiewic R, Jonczy B, Hansen AB, Oczachowska-Kulik AE, Thomsen IM, Bech JN, Pedersen EB. Cardiovascular effects of cholecalciferol treatment in dialysis patients--a randomized controlled trial. BMC Nephrol. 2014; 15:50.
20. Tolouian R, Rao DS, Goggins M, Bhat S, Gupta A. Seasonal variation of vitamin D in patients on hemodialysis. Clin Nephrol. 2010; 74:19–24.

21. Chang JH, Ro H, Kim S, Lee HH, Chung W, Jung JY. Study on the relationship between serum 25-hydroxyvitamin D levels and vascular calcification in hemodialysis patients with consideration of seasonal variation in vitamin D levels. Atherosclerosis. 2012; 220:563–568.

22. Yu A, Kim J, Kwon O, Oh SY, Kim J, Yang YJ. The association between serum 25-hydroxyvitamin D concentration and consumption frequencies of vitamin D food sources in Korean adolescents. Clin Nutr Res. 2013; 2:107–114.

23. Hur SJ, Kim DM, Lim KH, Yoon SH, Chung HC, Lee JS, Park J. Vitamin D levels and their relationship with cardiac biomarkers in chronic hemodialysis patients. J Korean Med Sci. 2009; 24:Suppl. S109–S114.

24. Del Valle E, Negri AL, Aguirre C, Fradinger E, Zanchetta JR. Prevalence of 25(OH) vitamin D insufficiency and deficiency in chronic kidney disease stage 5 patients on hemodialysis. Hemodial Int. 2007; 11:315–321.

25. Matias PJ, Ferreira C, Jorge C, Borges M, Aires I, Amaral T, Gil C, Cortez J, Ferreira A. 25-Hydroxyvitamin D3, arterial calcifications and cardiovascular risk markers in haemodialysis patients. Nephrol Dial Transplant. 2009; 24:611–618.

26. Figuiredo-Dias V, Cuppari L, Garcia-Lopes MG, de Carvalho AB, Draibe SA, Kamimura MA. Risk factors for hypovitaminosis D in nondialyzed chronic kidney disease patients. J Ren Nutr. 2012; 22:4–11.

27. Park YK, Lee YJ, Lee SS. The intake of food and nutrient by the elderly with chronic disease in the Seoul area. Korean J Nutr. 2012; 45:531–540.

28. Burgaz A, Akesson A, Oster A, Michaëlsson K, Wolk A. Associations of diet, supplement use, and ultraviolet B radiation exposure with vitamin D status in Swedish women during winter. Am J Clin Nutr. 2007; 86:1399–1404.

29. Russo R, Ruospo M, Cozzolino M, De Nicola L, Icardi A, Paoletti E, Mazzaferro S. Effects of vitamin D on parathyroid hormone and clinical outcomes in peritoneal dialysis: a narrative review. J Nephrol. 2014; 27:483–494.

30. Coyne DW, Goldberg S, Faber M, Ghossein C, Sprague SM. A randomized multicenter trial of paricalcitol versus calcitriol for secondary hyperparathyroidism in stages 3-4 CKD. Clin J Am Soc Nephrol. 2014; 9:1620–1626.

31. Lee YH, Kim JE, Roh YH, Choi HR, Rhee Y, Kang DR, Lim SK. The combination of vitamin D deficiency and mild to moderate chronic kidney disease is associated with low bone mineral density and deteriorated femoral microarchitecture: results from the KNHANES 2008-2011. J Clin Endocrinol Metab. 2014; 99:3879–3888.

32. Gruson D, Buglioni A, Burnett JC Jr. PTH: Potential role in management of heart failure. Clin Chim Acta. 2014; 433:290–296.

33. Palmer SC, Hayen A, Macaskill P, Pellegrini F, Craig JC, Elder GJ, Strippoli GF. Serum levels of phosphorus, parathyroid hormone, and calcium and risks of death and cardiovascular disease in individuals with chronic kidney disease: a systematic review and meta-analysis. JAMA. 2011; 305:1119–1127.

34. Anderson JL, Vanwoerkom RC, Horne BD, Bair TL, May HT, Lappé DL, Muhlestein JB. Parathyroid hormone, vitamin D, renal dysfunction, and cardiovascular disease: dependent or independent risk factors? Am Heart J. 2011; 162:331–339.e2.

35. Kestenbaum B, Katz R, de Boer I, Hoofnagle A, Sarnak MJ, Shlipak MG, Jenny NS, Siscovick DS. Vitamin D, parathyroid hormone, and cardiovascular events among older adults. J Am Coll Cardiol. 2011; 58:1433–1441.

36. Elder GJ. Vitamin D levels, bone turnover and bone mineral density show seasonal variation in patients with chronic kidney disease stage 5. Nephrology (Carlton). 2007; 12:90–94.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download