Abstract
Diet attrition and failure of long term treatment are very frequent in obese patients. This study aimed to identify pre-treatment variables determining dropout and to customise the characteristics of those most likely to abandon the program before treatment, thus making it possible to modify the therapy to increase compliance. A total of 146 outpatients were consecutively enrolled; 73 patients followed a prescriptive diet while 73 followed a novel brief group Cognitive Behavioural Treatment (CBT) in addition to prescriptive diet. The two interventions lasted for six months. Anthropometric, demographic, psychological parameters and feeding behaviour were assessed, the last two with the Italian instrument VCAO Ansisa; than, a semi-structured interview was performed on motivation to lose weight. To identify the baseline dropout risk factors among these parameters, univariate and multivariate logistic models were used. Comparison of the results in the two different treatments showed a higher attrition rate in CBT group, despite no statistically significant difference between the two treatment arms (P = 0.127). Dropout patients did not differ significantly from those who did not dropout with regards to sex, age, Body Mass Index (BMI), history of cycling, education, work and marriage. Regardless of weight loss, the most important factor that determines the dropout appears to be a high level of stress revealed by General Health Questionnaire-28 items (GHQ-28) score within VCAO test. The identification of hindering factors during the assessment is fundamental to reduce the dropout risk. For subjects at risk, it would be useful to dedicate a stress management program before beginning a dietary restriction.
Obesity is a multi-factorial disease, consisting of somatic and psychological co-morbidities implicated in chronic distress and a poor quality of life, affecting not only psychosocial but also physical domains [1]. Quality of life improvement can be attained by a specific dietary program. However, diet attrition and failure of long-term treatment are frequent in obese patients, reaching 80% with a mean of approximately 30% [2-4]. In recent literature, several authors focused their attention in weight-loss failure [1,5,6]. In their analysis, Wadden and Letizia [7] pointed out that several factors, such as binge eating, distress and a small weight loss early in the treatment, were the most important predictors of attrition. As reported in many studies, researchers identified different variables that are able to condition the patient's compliance to dietary protocols positively or negatively. In fact, attrition seems to be associated negatively with binge eating [8-10] and previous weight-reducing programs [11,12], positively to emotional disorders [13] and full-time job [14]. In contrast, in literature, the role of depression in dropout appears controversial, influencing both positively and negatively the patient acceptance of nutritional regimen [13,15]. Furthermore, recent studies demonstrate that excessive weight-loss expectation determines diet's attrition [11,12]. Therefore, obese and overweight patients need a strong primary motivation to tackle the weight-loss challenge [16]. The compliance to clinical therapy is fundamental to obtain successful and long-lasting results [11,17]. Observational studies underline the importance of making a point of "individual needs" to avoid dropout behaviour. However, our experience demonstrates that individual medical attention is not sufficient. The study of physical and psychological predictors of weight-loss program dropout is particularly important in clinical practice as it can serve as a basis for program improvement [18,19]. The present study evaluated the influence of the descriptive variables (such as sex, age, Body Mass Index, marital and job status, educational level and previous dietary programs) and the psychological profile (such as current weight satisfaction, weight-loss expectation, individual and external motivations) as baseline significant predictors of dropout. The goal of our investigation is to identify "weak subjects" who need a specific and detailed step-by-step clinical and psychological approach.
This study is part of a pragmatic randomized clinical trial [20] on the effectiveness of a novel brief group Cognitive Behavioural Treatment (CBT), accepted and performed in clinical practice, in addition to a prescriptive diet compared with the prescriptive diet alone (standard care), in obese and overweight outpatients without eating disorders. A total of 146 patients attending the Outpatient Clinic for Treatment of Obesity of Clinica Medica 2-I.R.C.C.S San Matteo General Hospital in Pavia were consecutively enrolled between March 2007 and March 2008. Among them, 73 patients followed the standard care and 73 the CBT in addition to the standard care. The study population was composed of 37 men and 109 women, with mean age of 45 ± 11 years and a Body Mass Index (BMI) ranging from 27 to 39.9. Although the trial lasted for 24 months, in the present study we analyse the dropout trend in the first six months.
Exclusion criteria were history of diabetes mellitus, pregnancy, endocrine disease, cancer or severe mental illness, the latter diagnosed according to the criteria of the Fourth Edition of Diagnostic and Statistical Manual of Mental Disorders (DSM-IV) [21]. Furthermore, subjects under pharmacological treatments that might induce weight variation, such as antidepressant, cortisone, oestrogen or progestin, were excluded. Patients with hypertension (defined according to European Hypertension Guidelines, 2007) [22] and dyslipidemia (defined according to Adult Treatment Panel III, 2004) [23] were eligible, if not treated.
The protocol was approved by Policlinico S. Matteo Ethic Committee (IRB 4861/2007/836) and written consent to the study was obtained before the weight-loss program enrolment. The study was registered on the internet as NCT01686854 at Clinical Trials.gov.
Weight-loss was obtained with a hypo-caloric balanced diet (15% of total calories as protein, 55-60% as carbohydrates, 30% as lipids), in accordance with the Italian and European Guidelines [24-26]. Basal metabolism and energy intake (kcal/day) were calculated according to the LARN [25] tables, based on the Shofield equation. All participants received a booklet explaining about food groups and portions' distribution, as recommended in the Italian Food Pyramid [26].
The treatment consisted of seven group sessions of 90 minutes each. All the meetings were held monthly in the first six months, then a control visit of 30 minutes was performed every three months until 12 month (at nine and 12 month) and every six months from 12 to 24 month. The groups were led by a physician, a therapist psychologist and a dietician; the first introductory meeting coincided with the first visit. The purpose of the seven CBT group sessions was to teach a self-instructional training approach.
The topics analyzed were:
1. The control of food intake (performed by a psychologist)
2. Hunger and satiety (performed by a physician)
3. Realistic goals and motivation to change (performed by a psychologist)
4. From weight to ration: self-care without weighing the food (performed by a dietician)
5. The management of "moments at risk" and relapse prevention (performed by a psychologist)
6. Physical activity and its importance in weight maintenance (performed by a dietician)
7. The drugs in the obesity treatment (performed by a physician)
Session themes were developed through multimedia, lectures and discussions among the participants, in order to involve them as much as possible; patients were helped to identify situations in which they found hard to control their eating behaviours, failing to quantify the daily food intake; at the same time, they were educated to self-manage hunger moments, or to self-control in social gatherings, such as at the restaurant, where it is difficult to detect the food composition. We not only underlined the importance of self-monitoring the energy intake as well as the physical activity, but also trained patients to set specific and realistic goals, aiming to change the cognitive process related to the weight gain. At the end of the sessions, the printed lesson summary was delivered to the patients to review the topics at home. The final sessions were devoted to review the materials and to talk about relapse prevention. At the beginning of every session, each subject was weighed privately and a blood pressure reading was taken. At the end of the treatment phase (six month) and on 12 month, participants in group B were re-evaluated by repeating all the blood and instrumental controls performed at baseline.
After baseline, eligible patients underwent randomized assignment to one of the two treatment conditions: standard care or CBT group. The clinical trial lasted for 24 months; in the present study, we examine the attrition trend in the first six months. Standard care consisted in a low calorie diet structured as mentioned above, with a deficit of about 500 calories from the daily requirement. Additionally, a control visit of about 30 minutes was performed every 3 months until 12 month and every 6 months from 12 to 24 month, for a total of five visits in the first year (considering the first visit the baseline), and of two visits in the second year. After randomization, patients and evaluators were not blinded to the condition. Patients in CBT group received the same diet pattern of standard care group, but in addition, they attended a series of seven subsequent meetings divided into small groups. At baseline, after familiar and personal anamnesis, patients were first examined by a physician who collected anthropometric and demographic parameters, blood pressure, and then by a trained dietician, who investigated their alimentary habits and previous diets. Patients underwent laboratory tests (glycaemia, lipid profile [Architect c-16000, Abbott Diagnostics], thyroid hormones [Immulite 2000, Siemens Helathcare Diagnostic]), Bioelectrical Impedance Analysis (BIA) [Omron BF 302] to estimate their body composition.
All patients underwent a semi-structured interview on weight-loss motivation, self-confidence in losing weight, satisfaction level with current weight; we also investigated if the patients' perception about weight-loss could be considered realistic or idealistic when compared with the final measured body weight. Realistic weight-loss goal was calculated as the percentage difference between desired goal and the same fixed by Italian Guidelines (10% Weight-loss on respect to basal weight at 6th month); we defined unrealistic goal a difference of more than 2% on respect to the guideline target. Realistic perception of one's own weight was calculated as percentage difference between the weight referred at the first examination by the subject and the real weight, as measured at basal anthropometric assessment; in this case, a gap of more than 2% was considered unrealistic perception. All participants completed VCAO-ANSISA test [27], an Italian psychological screening test consisting a combination of three questionnaires: Bulimic Investigatory Test of Edinburgh (BITE) in a short version of 16 items [28], Decision Balance Inventory (DBI) [29] and General Health Questionnaire-28 items (GHQ-28) [30]. On top of the patient's test score, a specialist enters within the computer program of the VCAO model some anthropometric data: age, sex, BMI, age of onset of overweigh, particularly relevant for their implications in the treatment success. The VCAO © (acronym that stands for assessment of eating behaviors in obese patients) model comes from a study carried out from 1990 to 1997 on 3,147 patients of many Italian centres for obesity treatment. The aim of the Italian researchers Ardovini, Caputo and Ostuzzi was to qualify the intervention of a specialist to improve the approach to the obese patient; their fields of interest in particular were feeding behaviour, mood disorders, motivation, cognitive restriction, risk for anorexia and bulimia and Body Image. They selected three tests and ideated a single tool, easy to self-compile, to contemplate in a single session either psychometric or anthropometric areas, for a first screening specifically devoted to obese subjects.
The Decisional Balance Inventory (DBI) test was developed on the Tanstheoretical Model of Behavior Change (TTM) by Prochaska and Velicer [31,32] who developed it as a valuable tool to assess motivation to change. It has been applied to different lifestyle changes, as reported in a recent review showing at least 48 fields of application [33]. Despite the near-unanimous agreement between clinicians and researchers on the evaluation and the intervention on weight loss patients' motivation, studies in the conceptualization field are limited if compared to those in the research field. The average time for completion of the questionnaire is less than 10 minutes. Although DBI has never been validated in Italian before, it is currently used to investigate the motivation in weight loss [34,35], and it is also recommended by some Italian scientific societies dealing with feeding [36].
The GHQ is used to detect psychiatric disorder in the general population and within community or non-psychiatric clinical settings such as primary care or general medical out-patients. This questionnaire assesses the respondent's psychological well-being and detects the presence of symptoms of stress that may indicate hypochondria. It estimates the current psychological state and evaluates it to see that differs from the usual state. Therefore, while being sensitive to short-term psychiatric disorders, it is not so to long-standing attributes of the respondent. The 28-item General Health Questionnaire (GHQ-28) is a scaled version: the organization in four subscales allows the physician to develop psychological diagnosis based on the cross-evaluation of scores derived from each area of investigation and not on the individual one, making the GHQ-28 version really useful as a diagnostic/prognostic tool. It contains 28 items that have been divided into four sub-scales through factor analysis. The GHQ-28 is the most well-known and popular version of the GHQ. The average time for completion of the questionnaire is less than 10 minutes. As for its application on obese patients GHQ, the study of Kivimaki and co-workers carried out on 6,000 obese patients makes a significant contribution [37]. This 'scaled' version of the GHQ has been developed on the basis of the results of principal components analysis. The four sub-scales, each containing seven items, are as follows:
A - somatic symptoms (items 1-7)
B - anxiety/insomnia (items 8-14)
C - social dysfunction (items 15-21)
D - severe depression (items 22-28)
The Bulimic Investigatory Test of Edinburgh (BITE) [23] is a test ideated in 1987 by Henderson and Freeman to estimate the presence of compulsive eating behaviour in order to reveal the true prevalence rate of binge-eating in a population. It is a screening test easy to administer, acceptable to subjects and simple to score; it is self-explanatory and can easily be given to large numbers of subjects for completion. Those subjects who have significant scores can be easily identified. The average time for completion of the questionnaire is less than 10 minutes. If the test is used as a screening instrument or in survey work, the subjects should be asked to complete the questionnaire based on their feelings and behavior over the past three months. Recently, this test has also been studied as a screening method for Binge Eating Disorder (BED) in obese patients [34]. The test was originally structured in a version of 33 items, and this complete version has been validated in Italian by Orlandi and co-workers [24]. The original version has been revised in a reduced, more agile form, as a result of an empirical study on the total sample of 3,147 patients (unpublished aforementioned data), using only 16 of the 33 original items.
- DBI test consists of 20 items, 10 representing processes that benefit and 10 factors that hinder weight loss (called Pro and Cons). A five point Likert scale was used for each item ranging from 1 (= not important) to 5 (= extremely important). Subjects were asked to rate the importance of each statement in influencing their decision whether or not to lose weight. The score is calculated by the ratio between the sum of the Cons and Pro. If the ratio is high, it means there are more Cons and the readiness to change is low. The cut off is considered a score > 1.5.
- GHQ-28: zero points are assigned to the first two responses and 1 point to the others. Total score ranges from 0 to 28. Higher scores indicate a greater probability of psychiatric distress. Total score that exceeds four out of 28 suggests probable distress. The test discriminates psychological health from mental illness, without establishing a hierarchy among diagnostic psychiatric disorders.
- BITE 16: the test was derived from the BITE test 33 items, using for the short form the numbers 2-3-5-10-12-13-14-15-19-20-22-23-24-25-29-30 of the original one. In the BITE test16 items, the score is calculated considering the items number 13 and 23, one point if the answer is NO, zero for YES: for all the other answers, one point if the answer is YES. Scores from 0 to 4 indicate the absence of disorder (zero points): one point if between 5 and 7, that is the presence of dysfunctional eating disorder, without bulimia: three points if > 7, that is highly dysfunctional eating behaviour and the presence of binge.
The scoring of the three tests produces an overall score that covers two main areas: the anthropometric-motivational area and psychiatric area. The overall score of the anthropometric-motivational area is the sum of the score of the anthropometric variables and of DBI score; the patient is at risk if the score is ≥ 5. The overall score of the psychiatric area is the sum of the score obtained from the BITE (one point if between 5and 7, three points if > 7) and GHQ-28 (three points if > 4). The patient is at risk if the score is ≥ 3.
In standard care group, we defined as dropout patients those who did not attend two consecutive visits, whereas in CBT group, a dropout was defined as a subject who did not attend four meetings. Before the withdrawal became definitive, each patient had been contacted by telephone and an explicit declaration of intent to withdraw from the trial was requested.
Categorical variables were described with counts and percentages: quantitative with mean and standard deviation (sd), if normally distributed, or median and interquartile range (IQR). Univariate logistic regression was performed using dropout as the dependent variable and those listed in Tables 1 and 2 as the explicatory variables. Odds ratios (OR) and 95% confidence intervals are reported (95% CI), together with P values, which were considered significant if below 0.05. All variables with P < 0.10 at univariate analysis were entered in multivariate analysis (GHQ, baseline one-self weight dissatisfaction degree, number of diets undertaken). The treatment arm (standard care group A versus CBT group) was not included in this analysis since it did not reach a significant P value (P = 0.127). All analyses were performed with Stata v. 11 (Stata Corporation, College Station, TX, USA).
Six months after baseline, 102 patients (69.9%) were still attending the weight-loss program, while 44 (30.1%) were lost to follow-up; nine of them dropped out for objective reasons (three women for pregnancy, four patients for acute illness and two subjects for unforeseen job difficulties); 26 patients (39.7%) dropped in CBT group while 18 patients (24.7%) dropped in standard care group, but not to a significant degree (P = 0.127). The two groups (completers and dropouts) were characterised for descriptive and psychological variables, as shown in Table 1. At the time of enrolment, 68.8% of completers and 61.4% of dropouts reported a BMI ≥ 30 kg/m2 (32.2 ± 3.7 kg/m2 and 32.4 ± 4.0 kg/m2, respectively); at three month after the beginning into the diet program, both groups reduced their BMI index (31 ± 4.8 kg/m2 for completers and 31 ± 2.4 kg/m2 for dropouts). As shown in Table 1, six months after the enrolment, 44 patients did not turn up for the appointment, while the 102 responders carried on nutritional protocol, further decreasing their BMI to 30.4 ± 4.5 kg/m2. Both groups showed a prevalence of female gender (73.5% in completers and 77.3% in dropouts); all patients were also characterized by high educational level and employed job status. They were more frequently married, with a mean age of 45 ± 10.2 years for responders and 43 ± 12.0 years for dropouts. The large majority of the participants reported previous attempts to lose weight, admitting several diet-cycling periods in their own life [25 patients (56.8%) among dropout and 77 patients (75.5 %) among completers; P = 0.0026]. At baseline, all patients were also investigated for psychological profile, as summarised in Table 1. Both groups, 99% of completers and 93.2% of dropouts, reported a baseline one-self weight dissatisfaction, but only 26.5% and 27.3%, respectively, expected to significantly decrease their weight in less than one year. Interestingly, the majority of the completers [25 patients (24.8%) P = 0.13] declared to pursue weight-loss for health motivations; on the other hand, the majority of the dropouts agreed to the dietary restraint program, primarily driven by aesthetics purpose [14 patients (31.8%) P = 0.13]. At first observation, there were no differences in median IQR scores concerning interview and psychometric tests between the two groups, thus suggesting the same psychological compliance to clinical nutrition program (Table 1).
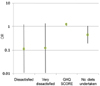
Logistic regression analysis was applied to identify behavioural (Table 2, Fig. 1) and psychological (Table 2, Fig. 1) factors responsible for dietary program's dropout. As shown in Table 2, only a history of previous weight-loss program attempts was implicated in completing the nutritional trial. In particular, patients experiencing previous dietary programs were prepared to follow out a new weight-loss protocol (P = 0.026, with OR = 0.43 and 0.20 < 95% CI > 0.90). In relation to psychological dropout's predictors, only GHQ-28 score produced a statistically significant P < 0.10 in the univariate logistic regression analysis (P = 0.017, with OR = 1.09 and 1.02 < 95% CI > 1.2), thus suggesting that the combination of somatic symptoms, anxiety, insomnia, social dysfunction and sever depression determine diet program's failure (Table 2). In the multivariate model, only GHQ-28 was significant [P < 0.10 in the univariate logistic regression analysis (Table 2)], and it can be considered a predictor of attrition, independently from both the dissatisfaction level and the previous treatment experiences. Otherwise, at the multivariate analysis, the level of satisfaction and the number of previously undertaken diets seem to be protective factors, but without any statistical significance. (Fig. 1).
Attrition is one of the major causes of treatment failure in the field of obesity. In obesity trials, attrition rates range from 10 to 80% [39] and vary according to the experimental design (randomized vs. observational study), and the type of treatment (drugs, behaviours, bariatric surgery). Since adherence to weight loss programs is a key component of long-term success [11,17], strategies are needed to reduce the dropout rates. In our study, six months after baseline, the majority of patients 102 patients (69.9%) were still attending the weight-loss program, while 44 (30.1%) dropped, with an attrition rate of 30.1%; this is in line with the literature. Comparison of the results in the two different treatments showed that 26 patients of the 73 enrolled (39.7%) dropped in CBT group while 18 patients of the 73 enrolled (24.7%) dropped in standard care group, although without any statistically significant difference (P = 0.127). Any factors may influence the adherence to a diet, such as disease state, the length of intervention, restrictiveness, and patient support. Specifically, the high attrition rate in CBT group can be explained by a more challenging program in terms of time, session frequency, and in particular, personal involvement. In fact, in the CBT group, the patient is no longer a passive subject, but directly interacts and is involved in the weight loss program. Given the high dropout percentage of patients entering a weight-loss program, it would be important to identify the main prognostic risk factors in the early phases of treatment [5]. In our study, the strongest predictor of dropout seems to be significant stress level. Two studies observed that the overall level of stress discriminates patients who discontinue treatment from those who complete their program [13,40]. Perhaps a pre-diet stress management program could be therapeutic for these "weak patients". Interestingly, if we focus our attention on compulsory eating and psychological trouble, only the latter is significantly associated with abandoning weight-loss program. Our data are in agreement with the most recent results disclaiming binge eating as a inevitable element of dropout [3,9,10], as well as with previous data showing a positive association between dropout and emotional disorders [3,7,11,13]. Furthermore, a high level of pre-treatment psychological troubles in patients attending our Department has been observed (data not shown). This concurs with studies which report that obese patients, declaring in anamnesis many weight-loss treatments, presented higher levels of psychopathologies when compared to obese patients who never looked for any treatment by a specialist [41-43]. Also, the multivariate analysis confirms the positive association between the psychiatric distress and dropout; in fact, a high GHQ score represents a risk factor for early dropout. One's current weight dissatisfaction could act as a stimulus, since patients who are unsatisfied with their weight could be strongly motivated to run out of the nutritional program; subjects experiencing previous diets might be less likely to dropout, because of their ability to cope with the program's difficulties, despite their unrealistic expectations. Our results show a higher trend of unrealistic expectations in those patients who finally dropped the nutritional program, and this is in line with literature [4]. Subjects experiencing previous diet programs declare the same unrealistic expectations, if compared with patients not used to diet protocols; previous experiences do not seem to have affected their detachment from reality. These data concur with other studies indicating that previous dietary experiences are insufficient to decrease unrealistic expectations, suggesting that an ideal "out of reach" body image was deep-seated in obese patients [2,4,11,17]. It would be interesting to study what extent the external environment (diet industry, media, etc.) and the individual personality affects this misperception. Moreover, our data are in contrast with previous findings indicating weight fluctuations as a barrier to successful treatment or a risk factor for attrition [3]; in fact, our study shows a lower dropout percentage in patients with cycling syndrome. In addition, patients subscribing to weight-loss program for health reasons could be strongly motivated not to abandon. According to Della Dalle Grave et al. [4], the primary motivation for weight-loss is the concern for one's future or present health. However, a strong baseline self-motivation is not sufficient to guarantee successful results; likewise, a continuous clinicians' pressure does not always result in attrition. Our analysis also shows that there are no differences between dropouts and completers in self-confidence, self-consciousness of the current body size and the weight-loss effort. As reported in literature, we find no differences in the anthropometric parameters (sex, age, BMI). Furthermore, our studies confirm that advanced age protects against dropout [3,4]; in fact, in our sample, completers are older than dropouts, even though without any statistical significance. Some authors hypothesized that older patients were conscious of weight-loss health benefits [44]. Interestingly, our study underlines job-status as a key role in pursuing dietary protocol, in contrast with previous findings [2,15], thus suggesting that job restrictions could protect patients from dropping the diet program, just as outside activities could prevent any transgress feeding behaviour. Psychometric tests seem to be an efficient baseline instrument to identify patients at risk of dropout. Although variables evaluated by semi-structured interview appear very useful to establish a strong therapeutic relationship with the patient, they appear less accurate in identifying predictors of dropout. We hypothesize that psychological troubles could represent the most important cause of dropout. Therefore, a psychological characterisation would be required not only at the enrolment, but also all over the six months trial, in order to create a step-by-step individual weight-loss program. In fact, dietary program alone is not the proper therapy for overweight and obese patients with psychological distress, because they are unable to control anxiety derived from nutritional strictness. In the presence of psychological troubles, a strong weight loss motivation appears insufficient in achieving the goal. Selection of participants according to prognostic factors for weight loss may be a valuable approach towards enhancing the efficiency of a program and the compliance to the therapy.
Figures and Tables
Fig. 1
Logistic multivariate analyses. Square represent OR (logaritmic scale) and bars 95% CI. High GHQ score represent a significant risk factor for abandoning weight loss program, while an high level of one-self weight dissatisfaction and previous diets are protective factor.
Acknowledgment
We thank Maria Zugnoni, Cristina Curti, Anna Crippa and Cristina Rava for their valuable contribution in the preparation of the diets.
References
1. Mannucci E, Petroni ML, Villanova N, Rotella CM, Apolone G, Marchesini G. QUOVADIS Study Group. Clinical and psychological correlates of health-related quality of life in obese patients. Health Qual Life Outcomes. 2010; 8:90.

2. Grossi E, Dalle Grave R, Mannucci E, Molinari E, Compare A, Cuzzolaro M, Marchesini G. Complexity of attrition in the treatment of obesity: clues from a structured telephone interview. Int J Obes (Lond). 2006; 30:1132–1137.

3. Olivieri M, Minniti A, Bosello O. Predittori di esito e prevenzione delle ricadute. In : Bosello O, editor. Obesità: un Trattato Multidimensionale. 2th Ed. Milano: Kurtis;2009. p. 845–851.
4. Dalle Grave R, Calugi S, Molinari E, Petroni ML, Bondi M, Compare A, Marchesini G. QUOVADIS Study Group. Weight loss expectations in obese patients and treatment attrition: an observational multicenter study. Obes Res. 2005; 13:1961–1969.

5. Moroshko I, Brennan L, O'Brien P. Predictors of dropout in weight loss interventions: a systematic review of the literature. Obes Rev. 2011; 12:912–934.

6. Vanderlinden J, Adriaensen A, Vancampfort D, Pieters G, Probst M, Vansteelandt K. A cognitive-behavioral therapeutic program for patients with obesity and binge eating disorder: short- and long-term follow-up data of a prospective study. Behav Modif. 2012; 36:670–686.

7. Wadden TA, Letizia KA. Predictors of attrition in weight loss in patients treated by moderate and severe caloric restriction. In : Wadden TA, Vanitallie TB, editors. Treatment of the Seriously Obese Patients. New York (NY): Guilford Press;1992. p. 383–410.
8. Ho KS, Nichaman MZ, Taylor WC, Lee ES, Foreyt JP. Binge eating disorder, retention, and dropout in an adult obesity program. Int J Eat Disord. 1995; 18:291–294.

9. de Zwaan M. Binge eating disorder and obesity. Int J Obes Relat Metab Disord. 2001; 25:Suppl 1. S51–S55.

10. Stunkard AJ, Allison KC. Two forms of disordered eating in obesity: binge eating and night eating. Int J Obes Relat Metab Disord. 2003; 27:1–12.

11. Dalle Grave R, Melchionda N, Calugi S, Centis E, Tufano A, Fatati G, Fusco MA, Marchesini G. Continuous care in the treatment of obesity: an observational multicentre study. J Intern Med. 2005; 258:265–273.

12. Teixeira PJ, Going SB, Houtkooper LB, Cussler EC, Metcalfe LL, Blew RM, Sardinha LB, Lohman TG. Pretreatment predictors of attrition and successful weight management in women. Int J Obes Relat Metab Disord. 2004; 28:1124–1133.

13. Yass-Reed EM, Barry NJ, Dacey CM. Examination of pretreatment predictors of attrition in a VLCD and behavior therapy weight-loss program. Addict Behav. 1993; 18:431–435.

14. Inelmen EM, Toffanello ED, Enzi G, Gasparini G, Miotto F, Sergi G, Busetto L. Predictors of drop-out in overweight and obese outpatients. Int J Obes (Lond). 2005; 29:122–128.

15. Clark MM, Guise BJ, Niaura RS. Obesity level and attrition: support for patient-treatment matching in obesity treatment. Obes Res. 1995; 3:63–64.

16. De Panfilis C, Torre M, Cero S, Salvatore P, Dall'Aglio E, Marchesi C, Cabrino C, Aprile S, Maggini C. Personality and attrition from behavioral weight-loss treatment for obesity. Gen Hosp Psychiatry. 2008; 30:515–520.

17. Perri MG, Sears SF Jr, Clark JE. Strategies for improving maintenance of weight loss. Toward a continuous care model of obesity management. Diabetes Care. 1993; 16:200–209.

18. Petroni ML, Villanova N, Avagnina S, Fusco MA, Fatati G, Compare A, Marchesini G. QUOVADIS Study Group. Psychological distress in morbid obesity in relation to weight history. Obes Surg. 2007; 17:391–399.

19. Womble LG, Williamson DA, Greenway FL, Redmann SM. Psychological and behavioral predictors of weight loss during drug treatment for obesity. Int J Obes Relat Metab Disord. 2001; 25:340–345.

20. Muggia C, Falchi AG, Michelini I, Montagna E, De Silvestri A, Grecchi I, Brondino N, Tinelli C. Brief group cognitive behavioral treatment in addition to prescriptive diet versus standard care in obese and overweight patients. A randomized controlled trial. ESPEN J [Internet]. cited 2013 Dec. Forthcoming 2013 Dec 5, Available from: http://dx.doi.org/10.1016/j.clnme.2013.11.002.
21. American Psychiatric Association (US). Diagnostic and statistical manual of mental disorders. 4th ed. Washington, D.C.: American Psychiatric Association;2000.
22. Mancia G, De Backer G, Dominiczak A, Cifkova R, Fagard R, Germano G, Grassi G, Heagerty AM, Kjeldsen SE, Laurent S, Narkiewicz K, Ruilope L, Rynkiewicz A, Schmieder RE, Boudier HA, Zanchetti A, Vahanian A, Camm J, De Caterina R, Dean V, Dickstein K, Filippatos G, Funck-Brentano C, Hellemans I, Kristensen SD, McGregor K, Sechtem U, Silber S, Tendera M, Widimsky P, Zamorano JL, Erdine S, Kiowski W, Agabiti-Rosei E, Ambrosioni E, Lindholm LH, Viigimaa M, Adamopoulos S, Agabiti-Rosei E, Ambrosioni E, Bertomeu V, Clement D, Erdine S, Farsang C, Gaita D, Lip G, Mallion JM, Manolis AJ, Nilsson PM, O'Brien E, Ponikowski P, Redon J, Ruschitzka F, Tamargo J, van Zwieten P, Waeber B, Williams B. Management of Arterial Hypertension of the European Society of Hypertension. European Society of Cardiology. 2007 Guidelines for the Management of Arterial Hypertension: The Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J Hypertens. 2007; 25:1105–1187.
23. Grundy SM, Cleeman JI, Merz CN, Brewer HB Jr, Clark LT, Hunninghake DB, Pasternak RC, Smith SC Jr, Stone NJ. National Heart, Lung, and Blood Institute. American College of Cardiology Foundation. American Heart Association. Implications of recent clinical trials for the National Cholesterol Education Program Adult Treatment Panel III guidelines. Circulation. 2004; 110:227–239.

24. Orlandi E, Mannucci E, Cuzzolaro M. SISDCA-Study Group on Psychometrics. Bulimic Investigatory Test, Edinburgh (BITE). A validation study of the Italian version. Eat Weight Disord. 2005; 10:e14–e20.

25. Task Force Obesità Italia (IT). LIGIO '99. Linee Guida Italiane Obesità. Bologna: Pendragon;1999.
26. Istituto Nazionale di Ricerca per gli Alimenti e la Nutrizione (IT). Istituto Nazionale Ricerca Alimenti e Nutrizione: Linee Guida per Una Sana Alimentazione Italiana [Internet]. Rome: Istituto Nazionale di Ricerca per gli Alimenti e la Nutrizione;2003. cited 2013 Dec. Available from: http://www.inran.it/files/download/linee_guida/lineeguida_intro.pdf.
27. Ardovini C, Caputo G, Ostuzzi R. La Valutazione del Rischio di Fallimento nel Trattamento dell'Obesità. Razionale dell'Utilizzo del V.C.A.O.-ANSISA nell'Approccio al Paziente Obeso [Internet]. Milano: Associazione Nazionale Specialisti in Scienza dell'Alimentazione;2007. cited 2013 Dec. Available from: http://www.ansisa.it/template.php?pag=46020.
28. Henderson M, Freeman CP. A self-rating scale for bulimia. The 'BITE'. Br J Psychiatry. 1987; 150:18–24.

29. O'Connell D, Velicer WF. A decisional balance measure and the stages of change model for weight loss. Int J Addict. 1988; 23:729–750.
30. Goldberg DP, Hillier VF. A scaled version of the General Health Questionnaire. Psychol Med. 1979; 9:139–145.

31. Prochaska JO, Velicer WF. The transtheoretical model of health behavior change. Am J Health Promot. 1997; 12:38–48.

32. Velicer WF, Prochaska JO, Fava JL, Rossi JS, Redding CA, Laforge RG, Robbins ML. Using the transtheoretical model for population-based approaches to health promotion and disease prevention. Homeost Health Dis. 2000; 40:174–195.
33. Hall KL, Rossi JS. Meta-analytic examination of the strong and weak principles across 48 health behaviors. Prev Med. 2008; 46:266–274.

34. Ricca V, Mannucci E, Moretti S, Di Bernardo M, Zucchi T, Cabras PL, Rotella CM. Screening for binge eating disorder in obese outpatients. Compr Psychiatry. 2000; 41:111–115.

35. Miotto P, De Coppi M, Frezza M, Petretto DR, Masala C, Preti A. Eating disorders and aggressiveness among adolescents. Acta Psychiatr Scand. 2003; 108:183–189.

36. Associazione Nazionale Specialisti in Scienza dell'Alimentazione (IT). Associazione Nazionale Specialisti in Scienza dell'Alimentazione [Internet]. Milano: Associazione Nazionale Specialisti in Scienza dell'Alimentazione;2013. cited 2013 Dec. Available from: www.ansisa.it.
37. Kivimäki M, Batty GD, Singh-Manoux A, Nabi H, Sabia S, Tabak AG, Akbaraly TN, Vahtera J, Marmot MG, Jokela M. Association between common mental disorder and obesity over the adult life course. Br J Psychiatry. 2009; 195:149–155.

38. Tsigos C, Hainer V, Basdevant A, Finer N, Fried M, Mathus-Vliegen E, Micic D, Maislos M, Roman G, Schutz Y, Toplak H, Zahorska-Markiewicz B. Obesity Management Task Force of the European Association for the Study of Obesity. Management of obesity in adults: European clinical practice guidelines. Obes Facts. 2008; 1:106–116.

39. Farley RL, Wade TD, Birchmore L. Factors influencing attendance at cardiac rehabilitation among coronary heart disease patients. Eur J Cardiovasc Nurs. 2003; 2:205–212.

40. Wadden TA, Bartlett S, Letizia KA, Foster GD, Stunkard AJ, Conill A. Relationship of dieting history to resting metabolic rate, body composition, eating behavior, and subsequent weight loss. Am J Clin Nutr. 1992; 56:203S–208S.

41. Obesità come problema psicologico. Dalle Grave R, editor. Terapia Cognitivo Comportamentale dell'Obesità. Verona: Positive Press;2001. p. 63–83.
42. Faith MS, Allison DB. Assessment of psychological status among obese persons. In : Thompson JK, editor. Body Image, Eating Disorders, and Obesity. Washington, D.C.: American Psychological Association;1996. p. 365–387.




 PDF
PDF ePub
ePub Citation
Citation Print
Print




 XML Download
XML Download