Abstract
The purpose of this study was to determine if Theory of Planned Behavior (TPB) variables predict soy milk intake in a sample of WIC participants in 2 Illinois counties (n = 380). A cross-sectional survey was used, which examined soy foods intake, behavioral beliefs, subjective norms, motivation, and intention. Soy product intake was low at both sites, and many participants (40%) did not know that soy milk was WIC approved. Most (> 70%) wanted to comply with their health care providers, but didn't know their opinions about soy milk (50-66%). Intention was significantly correlated with intake (0.507, P ≤ 0.01; 0.308, P ≤ 0.05). Environmental beliefs (0.282 and 0.410, P ≤ 0.01) and expectancy beliefs (0.490 and 0.636, P ≤ 0.01) were correlated with intention. At site 1, 30% of the variance in intention to consume soy milk was explained by expectancy beliefs and subjective norm beliefs (P < 0.0001); at site 2, 40% of the variance in intention was explained by expectancy beliefs. The TPB variables of expectancy beliefs predicted intention to consume soy milk in WIC participants. Therefore, knowing more about the health benefits of soy and how to cook with soy milk would increase WIC participants' intention to consume soy milk. Positive messages about soy milk from health care providers could influence intake.
The Special Supplemental Nutrition Program for Women, Infants, and Children (WIC) is the third largest food assistance program administered by the United States Department of Agriculture (USDA) [1]. The program served approximately 9.3 million low-income women, infants, and children younger than 5 years who were at nutritional risk during the final quarter of fiscal year 2009. Similar to the Korean nutrition program NutriPlus (+), which provides supplemental food, improves the nutrition knowledge of participants, and promotes breastfeeding [2], women and children participating in the WIC program also receive vouchers from local clinics for supplemental food as well as nutrition and breastfeeding education and referrals to health and social services.
For the fiscal year 2010, Congress appropriated $7.3 billion to cover WIC program costs, with WIC availability in all 50 states and the District of Columbia, as well as in tribal organizations and select American commonwealths. Ninety state agencies administer the program through approximately 2,200 local agencies and 9,000 clinic sites. Congress also appropriated $15 million for research related to the program for fiscal year 2010, which ended a long period in which there was very little funding for WIC research [3].
In October 2009, the USDA issued regulations that substantially revised the WIC food "package". A package does not represent actual food, but foods included on a WIC-approved list. These revisions are the first major change in the food package since the program's inception in 1972 [1]. The report WIC Food Packages: Time for a Change issued by the Institute of Medicine [4] largely influenced the changes to WIC-approved foods by bringing the packages into alignment with the recommendations from the Dietary Guidelines for Americans 2005 [5]. These revised packages include more fruits, vegetables, whole grains, placed priority on breastfeeding, and include soy foods [3].
Soy foods, such as fortified soy milk and calcium-set tofu, are excellent sources of calcium and high quality protein and are free of saturated fat and cholesterol. Calcium carbonate-fortified soy milk has the same calcium bioavailability as cow's milk, although availability from tricalcium-phosphate-fortified soy milk is somewhat lower [6]. However, consumption of soy milk has a similar positive effect on lowering osteoporosis risk as does cow's milk [7]. Additionally, in 1999 [8], and later modified [9], the U.S. Food and Drug Administration (FDA) approved the health claim that consuming 25 grams of soy protein per day may reduce the risk of coronary heart disease, when consumed as part of a diet low in saturated fat and cholesterol. Finally, the addition of soy foods to WIC packages is important because it expands options for milk for women and children, allows for cultural food preferences, and provides more choices for vegetarians/vegans and lactose intolerant individuals [10]. By including these alternative sources of calcium in the WIC food packages, the USDA has created a more flexible program that better serves the diverse WIC population. Before the 2009 revision of the WIC food packages, soy beverages were limited to infant formula and required a physician's recommendation that the patient should not consume cow's milk [11].
Twenty-six states and the District of Columbia have approved soy foods for their state WIC food packages. However, soy milk often requires a physician's authorization stating that there is a medical need before it can be an approved food for children. An additional 22 states have approved soy foods with certain restrictions. Soy beverages that are approved by WIC must be fortified to meet nutrient levels including 276 mg calcium per cup and 100 IU vitamin D per cup (Table 1).
Deciding to choose particular foods is a result of many psychosocial variables. To explain food-related behavior, numerous theories have been employed. One such theory, the Theory of Planned Behavior (TPB), states that attitudes, subjective norms surrounding the performance of the behavior, and perceived behavioral control predict the intention of an individual to perform a behavior (Fig. 1). This theory was chosen as a foundation for the soy milk questionnaire as it is appropriate for the analysis of discrete behaviors such as the intake of a specific food. Attitudes are one's attitude towards performing the behavior, and are based on behavioral beliefs. Subjective norm describes the beliefs of a group of people an individual perceives as important and is weighted by the normative beliefs of the individual to conform with that group. Perceived behavior control is a measurement of how difficult the individual perceives it to be to perform the behavior, and can include several perspectives on why or to what extent the behavior is difficult to [12,13]. The TPB has been used to identify mediators of intake of several foods and supplements, including novel foods enriched with omega-3 fatty acids [14], sustainably-produced foods [15], multivitamin use [16], fish consumption [17], family meal frequency [18], as well as soy foods [19,20].
Knowledge of the consumption patterns of WIC mothers concerning soy milk and soy foods could have a large impact for developing guidance relative to the inclusion of soy products in WIC supplemental packages and educational programs about soy foods. In addition, increased intake of soy milk could improve the nutritional status for those whose dairy or calcium-rich food intake is low.
Therefore, the objectives of this study were to investigate adult, female WIC participants' intake of and intention to consume soy milk using the TPB and identify key TPB variables that could be used to strengthen nutrition education efforts targeting soy milk intake.
A 2004 soy intake survey using the TPB [19] that was developed for use with Central Illinois women who had a wide range of socioeconomic levels was modified to reflect the WIC population. Questions related to WIC enrollment and demographics were added and the language was changed to focus on soy milk rather than all soy foods. There were 29 questions in addition to demographic items, which pertained to the TPB as follows: There were 3 items measuring subjective norm, 3 items measuring normative beliefs, 4 items measuring perceived behavioral control (2 related to outcome expectancies and 2 related to perceived environment), 4 items measuring control beliefs, 6 items measuring attitudes, and 4 items measuring intention. Five questions addressed the intake of soy foods (soy milk, veggie burgers and hotdogs, soy baked products, tofu, and edamame), and the remaining questions were related to soy milk specifically.
Cronbach alpha for constructs of the TPB were strong with one exception. Internal reliability for perceived behavioral control was not strong when the four items were grouped (0.57 and 0.59, for sites 1 and 2, respectively), but rose to a stronger level when split into two groups to reflect two concepts: outcomes expectancies (perceived knowledge of soy milk use and benefits) and perceived environment (availability and expense). Outcome expectancies and perceived environment were multiplied by control beliefs to create two new variables: environmental beliefs and outcome expectancy beliefs. Normative beliefs, or the motivation to comply with others' desires, was multiplied by subjective norm to create the variable subjective norm beliefs [12]. All survey items were measured on a 7-point Likert scale ranging from "strongly disagree" to "strongly agree", "extremely unlikely" to "extremely likely" and "extremely unpleasant" to "extremely pleasant." Where Cronbach alpha was ≥ 0.70 for multiple items within one behavioral construct, a composite value was derived and used in analyses [21].
The study was approved by the University Institutional Review Board who deemed it exempt from requiring informed consent of participants. A sheet providing information pertaining to the purpose of the study was provided to participants at the time of the survey. Two WIC Directors were invited to participate in the study, chosen because they had worked with the investigators previously on other projects, agreed to participate, and would have a fairly large client pool to recruit from, (active rosters of 4,400 participants enrolled at site 1 and 1,370 participants enrolled at site 2). To participate in the study, adults or their children must have been enrolled in WIC at one of the two sites, able to read English, and not have previously completed the survey. At site 1, an investigator was present in the waiting area several times per week to recruit participants for the self-administered survey. At site 2, WIC staff offered surveys to clients at the time of their appointment. Recruitment and data collection did not exceed 3 months to prevent duplication in surveys, since the 3-month period reflects the approximate time between routine clinic visits. After completing the surveys, participants could choose to be entered into a drawing for $50 by providing their contact information.
Data collected were entered into SPSS (version 18, Chicago, IL, 2009) and Microsoft Excel (Redmond, WA, 2010) for analysis. Distributions for demographics were not normally distributed as tested by kurtosis and skewness. Gender and age were normally distributed between the two sites. Data were significantly different (P < 0.05, Mann-Whitney U Test) for the two sites based on race/ethnicity and education. Therefore, separate analyses were conducted for the two clinics. The effects of site location and ethnicity on TPB variables were examined using Kruskal-Wallis independent analyses. Age categories were based on quartile distribution: Age category one (< 21 years), category 2 (22-25), category 3 (26-32), and category 4 (> 33). As responses were measured on 7-point Likert scale with neutral responses represented as 4, neutral responses were omitted from the calculation of composites in order to obtain an accurate representation of participants' beliefs. Bivariate correlations determined associations between TPB constructs and behavioral intention. Stepwise regression analyses were used to determine if the variance in intention could be explained by other TPB variables.
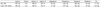
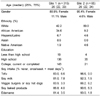
Most of the respondents at both sites were less than 34 years old (median for each county = 26 years) and female (87% at site 1 and 95% at site 2). Most participants were non-Hispanic white at site 2 (80%); however, site 1 participants were more diverse, with 42% non-Hispanic white and 35% African American. Most had completed high school (43% site 1; 54% site 2), with 45% either in college or having completed college at site 1 and 32% at site 2. Most in both counties did their own shopping and cooking. Few were vegetarian, had allergies to soy, or had children with allergies to soy. Approximately 40% of respondents in each county did not think soy was a WIC-approved food.
Intake of soy products was low. Most (64% site 1; 80% site 2) reported to rarely or never consume soy products. Similarly, 78% and 92% at sites 1 and 2, respectively, claimed to rarely or never drink soy milk in particular. There were 112 participants at site 1 (n = 315) and 13 at site 2 (n = 65) who reported consuming soy products.
The composite for subjective norm was measured on a scale of 1-6. The median response was 3.0 at site 1 and 2.0 at site 2, indicating that participants did not believe that healthcare professionals or their families thought they should consume soy milk. However, most participants (77.3% and 74.2% for sites 1 and 2, respectively) wanted to comply with what their own particular health care providers instructed them to do, and most felt that they wanted to comply with what health care providers in general wanted them to do (82.4% and 83.9%). About half to two-thirds (depending on site) reported not knowing what their health care provider thought about soy milk. Forty percent of participants at site 1 agreed health care experts would think people should drink soy milk whereas 50% of participants ate site 2 thought that health care experts neither agreed nor disagreed that they should consume soy milk. The other two items measuring normative beliefs related to health experts and family/friends were primarily neutral.
Medians measuring perceived behavioral control to consume soy milk, specifically regarding environmental beliefs and outcome expectancy beliefs, were also low. At site 1, 42% of participants said that the price of soy milk would make it unlikely for them to purchase it. However, at site 2, 44% indicated that price did not affect their decision. When asked about the availability of soy milk, 35% of site 1 participants and 43% of site 2 participants stated that the availability of soy milk did not make it more likely or less likely for them to consume it. Most at each site felt they did not know about the health benefits of soy milk (64% and 74%, sites 1, 2, respectively) and did not know how to cook with it (69% and 74%, sites 1, 2, respectively).
Bivariate correlations revealed that intention to consume soy milk was significantly correlated with intake for both sites (0.507, P ≤ 0.01; 0.308, P ≤ 0.05). Intention was also correlated with environmental beliefs (0.282 and 0.410, P ≤ 0.01) and expectancy beliefs (0.490 and 0.636, P ≤ 0.01).
Analysis by Kruskal-Wallis test for non-parametric data showed that the distribution of intake of soy products was significantly different between the 2 sites (P = 0.028), with site 2 soy consumers eating soy more frequently. However, no significant differences existed between sites for intention, attitudes, environmental beliefs, and expectancy beliefs related to soy milk intake. Distributions of intake, intention, and subjective norm beliefs were statistically different among ethnicities at site 1; however, data for attitudes, environmental beliefs, and expectancy beliefs were not different between the ethnicities. Tests to determine significant difference were not conducted at site 2 due to the high rate of white participants (80%).
Statistically significant equations were found using stepwise regression to predict the variance in behavioral intention for both counties. At site 1, 30% of the variance in intention to consume soy milk was explained by expectancy beliefs (β = 0.422) and subjective norm beliefs (β = 0.255) (P < 0.0001). At site 2, 40% of the variance in intention was explained by expectancy beliefs (β = 0.638) (P < 0.0001).
As reported in other U.S. studies, few participants in this study consumed soy milk regularly. A survey of Expanded Food and Nutrition Education Program (EFNEP) participants in Pennsylvania found only 13% consuming soy [22]. Intention to consume soymilk was generally negative, similar to a survey of attitudes towards changes in the WIC food basket in Maryland, where few consumed soy (13%) and most were not interested in trying those foods in the future [23]. Most of those respondents consumed whole milk (56%) and were not interested in low-fat milk. However, intention to consume soy has been shown to improve after tasting and education about the products [20]. Thus, education about the availability of new food products in the WIC food basket may help increase awareness and acceptability. In this study, 40% of participants at each site did not think that soy milk was a WIC-approved food. Nutrition education has been shown to move women through the stages of change toward more healthful diets [24]. The low intake of soy products in this study and other studies in the U.S. is in contrast to higher soy intake in other countries. For instance, a study of soy foods behavior in Korean housewives demonstrated a high intake in most participants of soy foods including soybean curd, soybean paste, Dambuk, soybean sprouts, and soy milk [25].
Regarding participants' beliefs and the subjective norm, the current study had similar findings to a study of North Carolina WIC participants who strongly agreed with the statement "I would eat nuts on most days of a week if my doctor recommended me to do so" [26]. Participants in this study in North Carolina, much like participants in the current study examining WIC participants and soy milk, had a low intake (7%) of the food of interest, nuts. This indicates a need for education about the benefits of soy delivered by medical professionals and WIC nutritionists.
Per bivariate correlation, soy consumption behavior was positively associated with intention. Thus, women with stronger intentions were more likely to consume more soy milk. This has been shown previously with a convenience sample of African American and non-Hispanic white women. Rah et al. [19] reported that intake, intention, beliefs about taste and health benefits, and control beliefs were not statistically different between African American and non-Hispanic white participants who were surveyed concerning their soy food intake. However, in the current sample of WIC participants, data for intake, intention, beliefs about taste and texture, and control beliefs were statistically different between ethnicities. Data for health beliefs (knowledge and behavior beliefs) were similar to those of Rah et al.
This was a cross-sectional survey to gauge intake and variables that may impact intake of soy milk in WIC mothers in Illinois. Previous work found that attitudes towards taste played a significant role in predicting intention. Therefore, changing the taste-related attitude may be important in planning programs to increase acceptance of soy [19]. Although taste testing is sometimes used to introduce new or novel foods, taste testing does not always change behavior. A study that provided yogurt as part of the WIC package with an educational component compared to a control group that did not receive yogurt found no significant difference in yogurt intake (P = 0.09) [27]. In another study, participants attending a diabetes education class were given a variety of soy products to taste. Although most tasted the samples, attitudes about taste and textures had no impact on intention to consume soy foods [20]. In that study, subjective norm and behavioral control were most important determinants in intention to consume soy. In the present study, subjective norm beliefs were important determinants of intention to consume soy milk. However, behavioral and control beliefs have been shown to be more easily influenced through education than normative beliefs in regards to dairy or calcium-rich foods intake [28,29]. Many, but not all, of the current participants felt that soy milk was a healthy food. Other studies have found that perceived food healthiness can affect intake of that food [30].
A study of soy and non-soy consumers reported that barriers to soy consumption include its unfamiliarity, negative image, and lack of preparation skills, which is similar to the present study [31]. However, Schyver and Smith found that those who did not consume soy expressed interest in learning how to prepare soy foods so they would taste good, whereas the current study participants did not explore interests in this area. These barriers can be addressed through WIC education that emphasizes how to incorporate soy foods into recipes and the diet. In another study, participants attending a diabetes education class were given a variety of soy products to taste. Although most tasted the samples, attitudes about taste and textures had no impact on intention to consume soy foods [20]. In that study, subjective norm and behavioral control were most important determinants in intention to consume soy. In the present study, subjective norm beliefs were important determinants of intention to consume soy milk.
There are several limitations to consider in this study including the smaller sample size in site 2 due to a shorter period of data collection. The survey was a convenience sample that consisted of mostly African American and non-Hispanic white participants and cannot be generalized to WIC populations with greater racial diversity. The soy consumption data was based on self-reported frequency of intake with the assumption that participants were using standard serving sizes and may not represent actual quantities of soy products consumed. In addition, other intake of other calcium-rich foods was not evaluated, so potential improvement in calcium intake with soy milk consumption cannot be estimated. At the time of this study, only one brand of soy milk, 8th Continent Original, was approved for WIC vouchers [32] and special authorization was required by a WIC nutritionist to purchase soy milk rather than cow's milk [33]. Finally, the TPB is useful at the individual level but cannot be used to address issues at the community level [34].
Positive correlations between TPB variables and behavioral intention indicate that WIC participants should be educated on the availability of soy in WIC packages and WIC nutritionists should emphasize its health benefits and information on how to use soy in recipes. Participants valued the opinions of health care providers. Therefore positive messages about soy milk could influence intake. In addition, more research is needed on soy intake among WIC participants, its impact on calcium intake, and the role soy milk may play in addressing lactose intolerance, vegetarian diets, and taste preferences.
Figures and Tables
 | Fig. 2
Correlations between theory of planned behavior constructs and intake of soy milk at site 1. Spearman's rho correlation **Significant at the 0.01 level (2-tailed) *Significant at the 0.05 level (2-tailed). |
 | Fig. 3
Correlations between theory of planned behavior constructs and intake of soy milk at site 2. Spearman's rho correlation **Significant at the 0.01 level (2-tailed) *Significant at the 0.05 level (2-tailed). |
Acknowledgements
This research was funded by the Illinois Soybean Association. Special thanks to the Champaign Urbana Public Health Department and the Marion County Health Department.
References
1. Oliveira V, Frazão E. The WIC Program Background, Trends, and Economic Issues, 2009 Edition. Economic Research Report Number 73. Washington D.C.: United States Department of Agriculture;2009.
2. Kim CI, Lee Y, Kim BH, Lee HS, Jang YA. Development of supplemental nutrition care program for women, infants and children in Korea: NutriPlus. Nutr Res Pract. 2009; 3:171–179.

3. Suitor CW. Institute of Medicine, Food and Nutrition Board. National Academies Press (US). Planning a WIC Research Agenda: Workshop Summary. Washington, D.C.: National Academies Press;2011.
4. Institute of Medicine, Committee to Review the WIC Food Packages (US). WIC Food Packages: Time for a Change. Washington, D.C.: National Academies Press;2006.
5. U.S. Department of Health and Human Services. U.S. Department of Agriculture (US). Dietary Guidelines for Americans 2005. 6th ed. Washington, D.C.: U.S. Government Printing Office;2005.
6. Zhao Y, Martin BR, Weaver CM. Calcium bioavailability of calcium carbonate fortified soymilk is equivalent to cow's milk in young women. J Nutr. 2005; 135:2379–2382.

7. Matthews VL, Knutsen SF, Beeson WL, Fraser GE. Soy milk and dairy consumption is independently associated with ultrasound attenuation of the heel bone among postmenopausal women: the Adventist Health Study-2. Nutr Res. 2011; 31:766–775.

8. U.S. Food and Drug Administration, Department of Health and Human Services (US). Food Labeling: Health Claims; Soy Protein and Coronary Heart Disease [Internet]. Silver Spring (MD): U.S. Food and Drug Administration;1999. 10. 26. cited 2012 Feb 21. Available from: http://www.gpo.gov/fdsys/pkg/FR-1999-10-26/pdf/99-27693.pdf.
9. U.S. Food and Drug Administration (US). Code of Federal Regulations. Title 21: Food and Drugs [Internet]. Silver Spring (MD): U.S. Food and Drug Administration;2011. cited 2012 Feb 21. Available from: http://www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfcfr/CFRSearch.cfm?fr=101.82.
10. Food Research and Action Center (US). New WIC Food Packages Proposed [Internet]. Washington D.C.: Food Research and Action Center;2006. cited 2012 Feb 21. Available from: http://frac.org/new-wic-food-packages-proposed/.
11. U.S. Department of Agriculture, Food and Nutrition Service (US). Special supplemental nutrition program for women, infants and children (WIC): revisions in the WIC food packages; interim rule. Fed Regist. 2007; 72:68965–69032.
12. Ajzen I. Attitudes, Personality and Behavior. Chicago (IL): Dorsey Press;1988.
14. Patch CS, Tapsell LC, Williams PG. Overweight consumers' salient beliefs on omega-3-enriched functional foods in Australia's Illawarra region. J Nutr Educ Behav. 2005; 37:83–89.

15. Robinson R, Smith C. Integrating issues of sustainably produced foods into nutrition practice: a survey of Minnesota Dietetic Association members. J Am Diet Assoc. 2003; 103:608–611.

16. Pawlak R, Connell C, Brown D, Meyer MK, Yadrick K. Predictors of multivitamin supplement use among African-American female students: a prospective study utilizing the theory of planned behavior. Ethn Dis. 2005; 15:540–547.
17. Verbeke W, Vackier I. Individual determinants of fish consumption: application of the theory of planned behaviour. Appetite. 2005; 44:67–82.

18. Eto K, Koch P, Contento IR, Adachi M. Variables of the Theory of Planned Behavior are associated with family meal frequency among adolescents. J Nutr Educ Behav. 2011; 43:525–530.

19. Rah JH, Hasler CM, Painter JE, Chapman-Novakofski KM. Applying the theory of planned behavior to women's behavioral attitudes on and consumption of soy products. J Nutr Educ Behav. 2004; 36:238–244.

20. Li S, Camp S, Finck J, Winter M, Chapman-Novakofski K. Behavioral control is an important predictor of soy intake in adults in the USA concerned about diabetes. Asia Pac J Clin Nutr. 2010; 19:358–364.
21. Nunnally JC. Psychometric Theory. 2nd ed. New York (NY): McGraw-Hill;1978.
22. Wenrich TR, Cason KL. Consumption and perceptions of soy among low-income adults. J Nutr Educ Behav. 2004; 36:140–143.

23. Black MM, Hurley KM, Oberlander SE, Hager ER, McGill AE, White NT, Quigg AM. Participants' comments on changes in the revised special supplemental nutrition program for women, infants, and children food packages: the Maryland food preference study. J Am Diet Assoc. 2009; 109:116–123.

24. Ritchie LD, Whaley SE, Spector P, Gomez J, Crawford PB. Favorable impact of nutrition education on California WIC families. J Nutr Educ Behav. 2010; 42:S2–S10.

25. Lee MJ, Park OJ. Soy food intake behavior by socio-demographic characteristics of Korean housewives. Nutr Res Pract. 2008; 2:275–282.

26. Pawlak R, Colby S, Herring J. Beliefs, benefits, barriers, attitude, intake and knowledge about peanuts and tree nuts among WIC participants in eastern North Carolina. Nutr Res Pract. 2009; 3:220–225.

27. Fung EB, Ritchie LD, Walker BH, Gildengorin G, Crawford PB. Randomized, controlled trial to examine the impact of providing yogurt to women enrolled in WIC. J Nutr Educ Behav. 2010; 42:S22–S29.

28. Nolan-Clark DJ, Neale EP, Probst YC, Charlton KE, Tapsell LC. Consumers' salient beliefs regarding dairy products in the functional food era: a qualitative study using concepts from the theory of planned behaviour. BMC Public Health. 2011; 11:843.

29. Lv N, Brown JL. Impact of a nutrition education program to increase intake of calcium-rich foods by Chinese-American women. J Am Diet Assoc. 2011; 111:143–149.

30. Provencher V, Polivy J, Herman CP. Perceived healthiness of food. If it's healthy, you can eat more! Appetite. 2009; 52:340–344.

31. Schyver T, Smith C. Reported attitudes and beliefs toward soy food consumption of soy consumers versus nonconsumers in natural foods or mainstream grocery stores. J Nutr Educ Behav. 2005; 37:292–299.

32. Illinois Department of Human Services (US). WIC Program Illinois Authorized WIC Food List [Internet]. Springfield (IL): Illinois Department of Human Services;2013. cited 2013 Apr 20. Available from: http://www.peoriacounty.org/download?path=/pcchd/IllinoisWICFoodList.pdf.
33. Illinois Department of Human Services (US). WIC Formula and Medical Nutritional Prescriptions [Internet]. Springfield (IL): Illinois Department of Human Services;2013. cited 2013 Apr 20. Available from: http://www.dhs.state.il.us/page.aspx?item=45972.
34. National Cancer Institute. U.S. Department of Health and Human Services. National Institutes of Health (US). Theory at a Glance: A Guide for Health Promotion Practice. NIH Publication No. 05-3896 [Internet]. Bethesda (MD): National Cancer Institute;2005. 09. cited 2013 Sep 5. Available from: http://www.cancer.gov/cancertopics/cancerlibrary/theory.pdf.




 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download