Abstract
BACKGROUND/OBJECTIVES
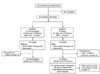
SUBJECTS AND METHODS
RESULTS
CONCLUSIONS
Figures and Tables
Table 1

Values are the mean ± standard error. Variables were examined for normality, and values not normally distributed were analyzed using non-parametric tests. Significance was tested using a paired t-test or Wilcoxon's signed-rank test based on normality; significance of weight, BMI, hip circumference, and fat mass were determined using Wilcoxon's signed-rank test.
*Significant difference between the two weight groups at baseline (P < 0.05). NS: not significant (P > 0.05).
Table 2

Values are the mean ± standard error. Variables were examined for normality, and values not normally distributed were analyzed using non-parametric tests. Significance was tested using a paired t-test or Wilcoxon's signed-rank test based on normality; significance of triglyceride, glucose, Total:HDL cholesterol, LDL:HDL cholesterol, serum leptin, and serum adiponectin were determined using Wilcoxon's signed-rank test. LDL:HDL cholesterol, ratio of LDL to HDL cholesterol; Total:HDL cholesterol, ratio of total to HDL cholesterol.
*Significant difference between the two weight groups at baseline (P < 0.05). NS: not significant (P > 0.05).
#A tendency towards a difference between the two weight groups at baseline (P < 0.1).
Table 3

Four obese men did not submit 3-day diet records at week 12.
Values are the mean ± standard error. Variables were examined for normality, and values not normally distributed were analyzed using non-parametric tests. Significance was tested using a paired t-test or Wilcoxon's signed-rank test based on normality. Significance of protein intake and percent calories from protein were determined using Wilcoxon's signed-rank test.
*Significant difference between the two weight groups at baseline (P < 0.05).
#A tendency towards a difference between the two weight groups at baseline (P < 0.1). NS: not significant (P > 0.05).
Table 4

Four obese men did not submit 3-day diet records at week 12.
Values are the mean ± standard error. Variables were examined for normality, and values not normally distributed were analyzed using non-parametric tests. Significance was tested using a paired t-test or Wilcoxon's signed-rank test based on normality. Significance of intakes of vitamin A, vitamin B6, folate, iron, and zinc were determined using Wilcoxon's signed-rank test.
*Significant difference between the two weight groups at baseline (P < 0.05).
#A tendency towards a difference between the two weight groups at baseline (P < 0.1). NS: not significant (P > 0.05).




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download