Abstract
BACKGROUND/OBJECTIVES
We investigated the effect of Pycnogenol (Pyc) on survival and immune dysfunction of C57BL/6 mice induced by low micronutrient supplementation.
MATERIALS/METHODS
Female C57/BL/6 mice were fed a diet containing 7.5% of the recommended amount of micronutrients for a period of 12 wks (immunological assay) and 18 wks (survival test). For immunological assay, lymphocyte proliferation, cytokine regulation, and hepatic oxidative status were determined.
RESLUTS
Pyc supplementation with 50 and 100 mg·kg-1·bw·d-1 resulted in partial extension of the median survival time. Pyc supplementation led to increased T and B cell response against mitogens and recovery of an abnormal shift of cytokine pattern designated by the decreased secretion of Th1 cytokine and increased secretion of Th2 cytokine. Hepatic vitamin E level was significantly decreased by micronutrient deficiency, in accordance with increased hepatic lipid peroxidation level. However, Pyc supplementation resulted in a dose-dependent reduction of hepatic lipid peroxidation, which may result from restoration of hepatic vitamin E level.
Malnutrition is the underlying cause of death in 45% of all deaths among children under the age of five in developing countries [1]. A diet consistently low in micronutrients results in cells that lack the nutrients essential for normal metabolic functions. In addition, micronutrient deficiency is a common cause of secondary immune dysfunction and is related to increased susceptibility to infection in humans [2]. Longitudinal studies have reported that 89% of immune deficient people had inadequate nutritional status with respect to at least one nutrient, and 41% had multiple abnormalities, the most predominant of which was inadequate plasma levels of micronutrients such as vitamin A, C, E, zinc, and selenium [2]. Another descriptive study found that 46% of subjects had below normal levels of zinc and iron, and 21% of subjects showed below normal albumin levels [3]. Although micronutrient status is not likely to be the most important etiological determinant, it may alter immune function to facilitate disease progression, influence viral expression, and have a significant impact on morbidity and mortality.
Pycnogenol (Pyc), a standardized extract from the French maritime pine bark (Pinus pinaster Ait.), consists of a concentrate of polyphenols whose main constituents are procyanidins, pharmacologically active biopolymers composed of units of catechin and epicatechin. In addition, Pyc contains the bioflavonoids catechin and taxifolin and a number of phenolic acids [4]. Pyc is known to exhibit efficient antioxidant activity and it may act as a modulator of metabolic and antioxidant enzymes and other cellular functions [5]. Several studies have reported that PYC inhibits LDL oxidation, lipid peroxidation in phospholipid liposomes, lipid peroxidation caused by t-butylhydroperoxide, and inflammation in capillary tissues [6,7]. However, evidence for relationship between Pyc supplementation and immune regulation is limited. Thus, the aim of this study was to evaluate the function of Pyc as a potent antioxidant to delay premature death caused by micronutrient deficiency and to investigate the immune parameters such as lymphocyte response and cytokine secretion during Pyc supplementation.
Female C57BL/6 mice, four weeks old, were obtained from SLC (Japan). They were housed in transparent plastic cages with stainless wire lids (3-4 mice per cage) in the animal facility of Kyung Hee University. Our animal use protocol was approved by the Institutional Animal Care and Use Committee of Kyung Hee University (KHUASP(SU)-12-12). The housing facility was maintained at 20-22℃ and 60-80% relative humidity with a 12-h light:dark cycle. For the study, mice were randomly assigned to four groups; normal group with AIN-93M rodent diet, micronutrient deficient group with AIN-93M diet only containing 7.5% of the recommended amounts of micronutrients in the AIN93M diet, and two groups with Pyc supplementation (50 or 100 mg·kg-1·bw·d-1) along with a low micronutrient AIN-93M diet. Oral administration of Pyc treatment began at two days before feeding the AIN-93M diet only containing 7.5% micronutrients and continued for 18 weeks for survival (12 mice/group) and 12 weeks for immunological analysis (six mice/group).
Pyc was generously donated from Jupiter International (Korean Branch of Horphag Research Ltd, Guernsey, FRA). Female C57BL/6 mice were administered either PYC or vehicle once daily by oral gavage at a dose of 50 or 100 mg·kg-1·bw·d-1 in 100 µl ethanol. A dose of 50 or 100 mg·kg-1·bw·d-1 was chosen as this dose was shown to be effective against lipogenesis or lipid metabolism in a previous study [8]. When immune dysfunction developed, all mice were sacrificed by ethyl ether anesthesia. Spleens were dissected and primarily cultured for measurement of lymphocyte mitogenesis and cytokine release. Livers for vitamin E and lipid peroxidation analysis were collected and stored at -70℃ until assayed.
Female C57BL/6 mice, four weeks old, were randomly assigned to one of the groups and fed a low micronutrient AIN93M rodent diet for 18 weeks to assess the effects of Pyc supplementation on survival. Mice were monitored everyday for survival and conditions while their drinking water and specified diets were changed every three days. Median survival time was defined as the expected number of days until occurrence of 50% of deaths in the treatment group.
Production of IL-2, IL-4, IL-6, IFN-γ, and TNF-α from mitogen-stimulated splenocytes was determined as described previously [9]. Briefly, spleens were gently teased with forceps in culture medium (RPMI 1640 CM containing 10% fetal bovine serum, 2 mmol/L glutamine, 1 × 105 units/L of penicillin and streptomycin), producing a suspension of spleen cells. Red blood cells were eliminated by addition of a lysis buffer (0.16 mol/L ammonia chloride tris buffer, pH 7.2) at 37℃ for 3 min. Then the primary cells were washed twice with culture medium. Cell concentrations were counted and adjusted to 1 × 107 cells/ml. The cell viability was > 95% as determined by trypan blue exclusion. Primary splenocytes [0.1 ml/well (1 × 107 cells/ml)] were cultured in triplicate on 96-well flat-bottom culture plates (Falcon 3072, Lincoln Park, NJ), and were then stimulated with concanavalin A (Con A, 1 × 10-2 g/L, 0.1 mL/well, Sigma, St. Louis, MO) to determine their production of IL-2 and IL-4 after incubation for 24 hours and IFN-γ after incubation for 72 hours in a 37℃, 5% CO2 incubator. Splenocytes were also simultaneously incubated for 24 hours after addition of lipopolysaccharide (LPS, 1 × 10-2 g/L, 0.1 mL/well, GibcoBRL, Grand Island, NY) to induce production of IL-6 and TNF-α. After incubation, supernatants were collected and stored at -70℃ until analysis. Cytokines were determined by sandwich ELISA.
Splenic T and B cell proliferation was determined by 3H-thymidine incorporation as described previously [6]. Briefly, splenocytes in 0.1 ml of culture medium (1 × 107 cells/ml) cultured in 96-well flat-bottom cultured plates (Falcon) with Con A(10 µg/ml) and LPS (10 µg/ml), were incubated at 37℃, 5% CO2 incubator for 24 hour, and then pulsed with 3H-thymidine (0.5 µCi / well, New England Nuclear, Boston, MA). After 24-hour incubation, they were harvested using a cell sample harvester (Cambridge Technology, Cambridge, MA). Radioactivity was determined using a liquid scintillation counter (Tri-Carb, 2200 CA, Packard, Laguna Hills, CA). Data were collected as counts per minute (cpm).
Lipid peroxidation (LPO) in liver was measured by K-Assay™ using a LPO-CC Assay Kit obtained from Kamiya Biomedical Company (Seattle, WA). This method has previously been shown to be a more sensitive lipid peroxide measurement (assay range: 2-300 nmol/ml) than conventional chemical analysis [10]. Briefly, ~0.2 g of liver tissue was homogenized in 3 ml of CHCl3/methanol (2:1, v/v). 0.6 ml of 0.9% NaCl was added to clarify and the mixture was centrifuged at 3000x g for 10 min. The supernatant was discarded while the bottom layer that includes CHCl3 was evaporated under N2 gas. 100 µl of isopropanol was added to dissolve lipid residue and 20 µl of sample was used for measurement of lipid peroxides using the LPO Kit. In the presence of hemoglobin, lipid hydroperoxides are reduced to hydroxyl derivatives (lipid alcohols) and the MCDP (10-N-Methylcarbamoyl-3, 7-dimethylamino-10 H-phenolthiazine) chromagen is oxidatively cleaved to form methylene blue in an equal molar reaction. Lipid peroxides are quantitated by colorimetric measurement of methylene blue at 675 nm. Lipid peroxidation values were calculated using the equation given from the manual. LPO value was converted to the percent unit for illustration.
Hepatic vitamin E levels were measured by HPLC as described previously [11]. Briefly, 0.2 g of tissues was homogenized in 1 ml of water. Butylated hydroxytoluene (BHT) was added to prevent oxidation of α-tocopherol. Pentane, ethanol, and sodium dodecyl sulfate were used for extraction of α-tocopherol from the homogenate. Extracts were evaporated under steady flow of nitrogen gas at 20℃ and then redissolved in 0.5 mL of methanol injected onto a C18 column (3.9 × 150-mm NovaPak, Millipore, Bedford, MA). A mobile phase composed of methanol and 1 mol/L sodium acetate in the ratio of 98:2 (v/v) at a flow rate of 1.5 ml/min was used. α-tocopherol with a retention time of approximately 5 min, was monitored using a fluorescence detector (Millipore, Bedford, MA) at 290-nm excitation and 320-nm emission wavelength.
The probability of treatment effects was assessed in this study using one-way ANOVA. Mean differences between treatment groups of micronutrient deficiency diets and the control groups were tested using two-tailed Student's t test. Test statistics were considered significant at the P < 0.05 level.
No significant difference in dietary intake was observed between groups during a period of 10 weeks. However, a decrease in dietary consumption was observed in the 7.5% micronutrient group from 11 weeks until time for sacrifice. According to this result, significant difference in body weight was observed between mice consuming the normal AIN93M diet (29.62 ± 1.37 g/mouse) and the 7.5% micronutrient diet (19.9 ± 2.43 g/mouse). This result is in accordance with that of our previous study indicating the effect of micronutrient deficiency on immunomodulation [12]. This observation was ameliorated in part by Pyc supplementation with 50 and 100 mg·kg-1·bw·d-1 (23.4 ± 1.2 and 25.7 ± 1.4 g/mouse), which showed significant difference compared to the control group. However, no statistical difference was observed between mice with Pyc supplementation. Spleen weights showed a slight but significant (P < 0.05) reduction in the 7.5% micronutrient group (data not shown). Of particular interest, spleen size was found to be normal in Pyc supplementation groups, indicating that both 50 and 100 mg·kg-1·bw·d-1 may be sufficient to compensate for size reduction of spleen caused by the 7.5% micronutrient diet.
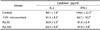
Based on the study by Lee et al. [12], suggesting that intake of 7.5% of micronutrients from the AIN93M diet caused immune deficiency, we decided to feed diets with 7.5% micronutrient content from the standard AIN93M rodent diet. The median survival time was 87 days in mice fed the 7.5% micronutrient diet, consistent with Lee's report in which the median survival time was 81 days. However, the median survival time of mice fed 50 and 100 mg·kg-1·bw·d-1 of Pyc was 108 and 110 days, respectively (Table 1). No significant difference in median survival time was observed between Pyc supplemented groups.
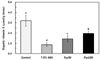
Mice fed the 7.5% micronutrient diet showed significant impairment of B cell proliferation compared to normal control mice (Fig. 1). Similar results were obtained on T cell proliferation in mice fed the 7.5% micronutrient diet (Fig. 1). Both T and B cell response against mitogens showed a significant increase with Pyc supplementation at a dose of 100 mg·kg-1·bw·d-1, however no difference was observed between mice fed 50 mg·kg-1·bw·d-1 and mice fed the 7.5% micronutrient diet.
Production of IL-2 and IFN-γ by Con A-stimulated splenocytes was significantly (P < 0.05) reduced in the group fed the 7.5% micronutrient diet (Table 2). Otherwise, release of TNF-α, IL-4, and IL-6; by LPS-stimulated primary splenocytes was significantly (P < 0.05) increased in the group fed the 7.5% micronutrient diet (Table 3). Intake of Pyc at 50 and 100 mg·kg-1·bw·d-1 resulted in enhanced production of IL-2 and IFN-γ, but only treatment with 100 mg·kg-1·bw·d-1 resulted in reduced production of IL-4 and TNF-α. Unfortunately Pyc supplementation did not change the level of IL-6. These results indicated that Pyc mainly affects Th1 cytokines rather than Th2 cytokines.
Intake of a 7.5% micronutrient diet enhanced hepatic lipid peroxidation by 274%. Consumption of Pyc at a dose of 100 mg·kg-1·bw·d-1 resulted in significantly reduced hepatic lipid peroxidation. Intake of 50 mg·kg-1·bw·d-1 Pyc only resulted in partial reduction of hepatic lipid peroxidation, but its degree was very slight. Hepatic vitamin E level decreases during low levels of antioxidant and/or micronutrient intake due to increased free radicals, resulting in increased tissue lipid peroxidation. To estimate the effects of restricted micronutrient intake on production of free radicals, hepatic vitamin E level was measured. Not surprisingly, intake of a 7.5% micronutrient diet resulted in a significantly decreased level of hepatic vitamin E. However, Pyc supplementation resulted in dose-dependent restoration of the hepatic vitamin E levels (Fig. 3).
In the study of malnutrition and the immune system, it is very interesting to consider that nutritional deficiency primarily affects life span. Pyc contains mainly procyanidins comprised of catechin and epicatechin subunits and other constituents such as polyphenolic monomers, phenolic or cinnamic acids and their glycosides (D'Andrea G). Pyc is also known to be highly bioavailable for several physiological impairments. Thus, it is believed that Pyc could at least in part replace low micronutrient status in physiological functions. In a morbidity and nutritional impairment study of the Zambian population, the author suggested a significant association of nutritional impairment with impairment of the immune system, which results in premature death [13]. Some micronutrients act as antioxidants; these are of particular importance in reference of malnutrition, a status in which increased oxidative stress and antioxidant deficiencies have been described [14]. Thus, our animal survival study may support the idea that Pyc, as a potent antioxidant, partially delayed premature death by compensating for cellular antioxidative status caused by lack of micronutrients.
Shortage of life span in an animal with low micronutrient intake could be explained by two possible mechanisms, immune dysregulation and excessive free radical production. Low micronutrient intake is thought to involve cytokine dysfunction, since micronutrient deficiencies can modify cytokine production or its receptor expression [15] and cause a shift from balanced Th1/Th2 cell secretion of cytokines to increased Th2 and decreased Th1 cell cytokine production [16]. In another study of undernourishment, 50% of animals fed the nourished diet exhibited an altered cytokine expression profile, resulting in change of Th1/Th2 cytokine balance mainly associated with number of T and B lymphocytes [17]. In addition, Thurnham [18] reported that the main effect of micronutrient deficiencies is the reduction in cell mass that indirectly affects immune cell function, particularly when T cell numbers are reduced. These results are in accordance with our findings of decreased proliferation under conditions of micronutrient deficient dietary intake. The animal study reported by Liu et al. suggested that oral feeding with Pyc for two months significantly augmented the proliferative capacity of T and B lymphocytes [19]. In our study, feeding with only 100 mg·kg-1·bw·d-1 Pyc, but not 50 mg·kg-1·bw·d-1, was sufficient to restore T and B cell function associated with micronutrient deficiency. Decreased cell division by micronutrient deficiency could be expected due to decreased release of IL-2, a major T-cell growth factor. Our laboratory previously showed that reduced micronutrient intake exacerbated the ability of T and B cells to proliferate and altered immunoglobulin production by an increase in the number of B cells stimulated by heightened IL-4 secretion [12]. However, our data indicated suppressed B cell proliferation by both micronutrient deficient diets. It is clear that B-cell proliferation was determined by stimulation of LPS, while IL-4 secretion was induced by ConA. Thus, in our in vitro study, IL-4 production did not affect B-cell proliferation. Therefore, micronutrient deficient diets may directly damage the proliferative function or indirectly block the signal transduction required for stimulation of B lymphocytes.
As another possible mechanism of premature death, excessive free radical induction may be a result of a micronutrient deficient diet, evidenced by increased lipid peroxidation (Fig. 2). Consistent with data on lipid peroxidation, increased free radicals produced during intake of reduced micronutrients could stimulate utilization of antioxidants, including membrane vitamin E (Fig. 3) [20]. For instance, as evidenced by the decreased production of IL-2 during low selenium and zinc intake [20], most cytokine alteration may be due to deficiency of antioxidant nutrients. Pro-inflammatory cytokines (IL-1, IL-6, and TNF-α) and reactive oxygen species (ROS) are mutually stimulatory [21]. Stimulation of cytokine production by ROS involves activation of nuclear factor kappa B (NF-κB), which induces a systemic inflammatory reaction, resulting in premature death. Similarly, our data showed that lipid peroxidation, a marker of increased presence of ROS, was markedly increased by low micronutrient intake and restored by Pyc supplementation (Fig. 2). Since low micronutrient status could increase both cellular and plasma level of oxidants and TNF-α, dietary intake deficient in micronutrients may cause dysregulated production of these parameters. In addition, oxidative stress due to reduced levels of antioxidants may be a potent inducer of DNA damage in micronutrient deficient cells, producing one of the long-term consequences of immunosuppression [22]. Pyc, as a potent antioxidant, can regulate the cellular secretion of cytokines by inhibiting NF-κB and is well estimated to block both non-enzymatic and enzymatic oxidation associated with DNA damage [23]. Thus, in our study, restoration of the immune system by Pyc supplementation could be related to its antioxidative ability to prolong the life span of T and B lymphocytes by suppressing DNA damage. In animal study, vitamin E deficiency impairs cellular and humoral immunity while it increases the incidence of disease. Amarakoon et al. [24]; reported that rats fed diets deficient in vitamin E after injections of endotoxin showed more anorexia and expressed higher IL-6 levels than animals consuming adequate amounts.
In conclusion, our results may indicate that Pyc supplementation helped increase life span in mice associated with micronutrient deficiency by restoring immune dysfunction and cellular antioxidant levels.
Figures and Tables
 | Fig. 1
Effect of reduced micronutrient intake on T and B cell mitogenesis in vitro. Data are presented as mean ± SD of triplicate wells. aP < 0.05 in comparison with uninfected control mice, bP < 0.05 in comparison with infected control mice. |
 | Fig. 2
Effect of reduced micronutrient intake on hepatic lipid peroxidation. Data were converted to percent unit (% = value of treatment group/value of control group × 100). aP < 0.05 in comparison with uninfected control mice, bP < 0.05 in comparison with infected control mice. |
 | Fig. 3
Effect of reduced micronutrient intake on vitamin E levels in liver. Data are represented by mean ± SD of triplicate wells. aP < 0.05 in comparison with uninfected control mice, bP < 0.05 in comparison with infected control mice. |
Table 1
Median survival time of mice in the study of LP-BM5 retrovirus infection and micronutrient deficiency

References
1. Brown KH, Hess SY, Vosti SA, Baker SK. Comparison of the estimated cost-effectiveness of preventive and therapeutic zinc supplementation strategies for reducing child morbidity and mortality in sub-Saharan Africa. Food Nutr Bull. 2013; 34:199–214.

2. Nunnari G, Coco C, Pinzone MR, Pavone P, Berretta M, Di Rosa M, Schnell M, Calabrese G, Cacopardo B. The role of micronutrients in the diet of HIV-1-infected individuals. Front Biosci (Elite Ed). 2012; 4:2442–2456.

3. Campa A, Shor-Posner G, Indacochea F, Zhang G, Lai H, Asthana D, Scott GB, Baum MK. Mortality risk in selenium-deficient HIV-positive children. J Acquir Immune Defic Syndr Hum Retrovirol. 1999; 20:508–513.

4. Rohdewald P. A review of the French maritime pine bark extract (Pycnogenol), a herbal medication with a diverse clinical pharmacology. Int J Clin Pharmacol Ther. 2002; 40:158–168.

5. Maimoona A, Naeem I, Saddiqe Z, Jameel K. A review on biological, nutraceutical and clinical aspects of French maritime pine bark extract. J Ethnopharmacol. 2011; 133:261–277.

6. Zibadi S, Rohdewald PJ, Park D, Watson RR. Reduction of cardiovascular risk factors in subjects with type 2 diabetes by Pycnogenol supplementation. Nutr Res. 2008; 28:315–320.

7. Kim YJ, Kim YA, Yokozawa T. Pycnogenol modulates apoptosis by suppressing oxidative stress and inflammation in high glucose-treated renal tubular cells. Food Chem Toxicol. 2011; 49:2196–2201.

8. Kamińska T, Szuster-Ciesielska A, Wysocka A, Marmurowska-Michałwska H, Dubas-Slemp H, Kandefer-Szerszeń M. Serum cytokine level and production of reactive oxygen species (ROS) by blood neutrophils from a schizophrenic patient with hypersensitivity to neuroleptics. Med Sci Monit. 2003; 9:CS71–CS75.
9. Chouaib S, Welte K, Mertelsmann R, Dupont B. Prostaglandin E2 acts at two distinct pathways of T lymphocyte activation: inhibition of interleukin 2 production and down-regulation of transferrin receptor expression. J Immunol. 1985; 135:1172–1179.
10. Ohishi N, Ohkawa H, Miike A, Tatano T, Yagi K. A new assay method for lipid peroxides using a methylene blue derivative. Biochem Int. 1985; 10:205–211.
11. Burton GW, Webb A, Ingold KU. A mild, rapid, and efficient method of lipid extraction for use in determining vitamin E/lipid ratios. Lipids. 1985; 20:29–39.

12. Lee J, Park CS, Chung MY, Cho DH, Watson RR. Reduced micronutrient intake accentuates premature death caused by immune dysfunction in leukemia retrovirus-infected C57BL/6 mice. Nutr Res. 2005; 25:401–412.

13. Kelly P, Zulu I, Amadi B, Munkanta M, Banda J, Rodrigues LC, Mabey D, Feldman R, Farthing MJ. Morbidity and nutritional impairment in relation to CD4 count in a Zambian population with high HIV prevalence. Acta Trop. 2002; 83:151–158.

14. Ghone RA, Suryakar AN, Kulhalli PM, Bhagat SS, Padalkar RK, Karnik AC, Hundekar PS, Sangle DA. A study of oxidative stress biomarkers and effect of oral antioxidant supplementation in severe acute malnutrition. J Clin Diagn Res. 2013; 7:2146–2148.

15. Wessels I, Haase H, Engelhardt G, Rink L, Uciechowski P. Zinc deficiency induces production of the proinflammatory cytokines IL-1β and TNFα in promyeloid cells via epigenetic and redox-dependent mechanisms. J Nutr Biochem. 2013; 24:289–297.

16. Prasad AS. Effects of zinc deficiency on Th1 and Th2 cytokine shifts. J Infect Dis. 2000; 182:Suppl 1. S62–S68.

17. Dzhagalov I, Chambon P, He YW. Regulation of CD8+ T lymphocyte effector function and macrophage inflammatory cytokine production by retinoic acid receptor gamma. J Immunol. 2007; 178:2113–2121.

18. Thurnham DI. Interactions between nutrition and immune function: using inflammation biomarkers to interpret micronutrient status. Proc Nutr Soc. 2014; 73:1–8.

19. Liu FJ, Zhang YX, Lau BH. Pycnogenol enhances immune and haemopoietic functions in senescence-accelerated mice. Cell Mol Life Sci. 1998; 54:1168–1172.

20. Alvarado C, Alvarez P, Puerto M, Gausserès N, Jiménez L, De la Fuente M. Dietary supplementation with antioxidants improves functions and decreases oxidative stress of leukocytes from prematurely aging mice. Nutrition. 2006; 22:767–777.

21. Bubici C, Papa S, Dean K, Franzoso G. Mutual cross-talk between reactive oxygen species and nuclear factor-kappa B: molecular basis and biological significance. Oncogene. 2006; 25:6731–6748.

22. Vaid M, Prasad R, Singh T, Elmets CA, Xu H, Katiyar SK. Silymarin inhibits ultraviolet radiation-induced immune suppression through DNA repair-dependent activation of dendritic cells and stimulation of effector T cells. Biochem Pharmacol. 2013; 85:1066–1076.





 PDF
PDF ePub
ePub Citation
Citation Print
Print



 XML Download
XML Download