Abstract
BACKGROUND/OBJECTIVES
The body composition changes in aging increased the risk of metabolic disorder. Recent dietary studies have increasingly focused on the correlations between dietary patterns and chronic diseases to overcome the limitations of traditional single-nutrient studies because nutrients in food have complex relations that interact.
SUBJECTS/METHODS
This study was conducted to classify a dietary pattern among Korean elderly using cluster analysis and to explore the relationships between dietary patterns and body composition changes in Korean elderly aged 65 years or older. The study subjects (n = 1,435) were individuals who participated in the Korean National Health Examination and Nutrition Survey (KNHANES) in 2011.
RESULTS
There were three dietary patterns derived by cluster analysis in this study: 'Traditional Korean' (37.49% of total population), 'Meat and Alcohol' (19.65%) and 'Westernized Korean' (42.86%). The (1) 'Traditional Korean' pattern was characterized by high consumptions of white rice and low protein, low fat, and low milk products, while (2) 'Westernized Korean' pattern ate a Korean-style diet base with various foods such as noodles, bread, eggs and milk, (3) 'Meat and Alcohol' pattern had high consumptions of meat and alcohol. In body composition changes, compared with the 'Traditional Korean' pattern, the 'Meat & alcohol' pattern was associated with a 50% increased risk of having elevated BMI (kg/m2), 'Westernized Korean' pattern was associated with a 74% increased abnormality of ASM/Wt (kg) by logistics analysis. Most of the Korean adult population continues to follow ether a traditional Korean having beneficial effects for successful aging. However, the 'Traditional Korean' pattern showed low protein intake (0.7 g/kg), calcium intake, and vitamin D intake as well as low of appendicular skeletal muscle mass (ASM (kg)) among 3 groups.
The Korean population is rapidly aging and becoming an aged society as other developed countries. Approximately 10.3% of the Korean population was aged 65 and older in 2008, and the percentage is expected to rapidly rise to 20.3% in 2027 and 34.4% in 2050 [1]. Aging causes typically physiological changes such as a progressive loss of muscle mass and an increase of fat mass called sarcopenic obesity (SO) [2]. These body composition changes reduce insulin sensitivity which is associated with an increase of the risk of metabolic syndromes (MS) and causes loss of muscle mass results in muscle weakness, increased fall risk, and fat infiltration in the skeletal muscle [3]. Despite their enormous clinical importance, body composition changes such as SO in the elderly are often under-recognized. This change is a life-long process, and result from complex factors such as reduced levels of physical activity and the age-associated decline in anabolic hormones (reduced vitamin D, testosterone, estrogen, and growth hormone levels), insulin resistance, inflammation and imbalanced dietary intake in aging [4]. Even though the specific contribution of body composition changes are unknown, there is emerging evidence that the disruption of several positive regulators (Akt; Rac-alpha serine/threonine-protein kinas/mTOR; mammalian target of rapamycin, signaling pathway related insulin signaling) of muscle mass is associated with insulin sensitivity [5,6]. Insulin resistance and impaired glucose tolerance association with proinflammatory cytokines from adiopocytes in central obesity possibly stimulate a vicious cycle leading to accelerated loss of muscle mass and additional weight gain [7]. Actually muscle tissue is an important role in reserving of body proteins, generating energy, and disposing glucose. Recently, nutritional research has considered epigenetics that lifestyle and nutrients have a influence on preventing some of metabolic disorders [8,9]. According to Ilanne-Parikka et al. [10], these disorders were significantly reduced in a lifestyle intervention. So, to prevent body composition changes, it has been suggested that we need to understand lifestyle-associated risk factors including a high body mass index (BMI), smoking, low level of physical activity, and bad eating habits. Among them, the most effective way was a nutrient intervention, nutritional research has considered that nutrients such as good quality of protein, vitamin D, calcium, omega-3 fatty acids, and vitamin C stimulate protein synthesis by initiating mTOR (mammalian target of rapamycin) signaling pathway and also decrease inflammation cytokines [11]. There are many studies has been reported that calcium intake and vitamin D status could be correlated with body weight, body composition, and insulin resistance [12]. Recently, dietary studies have increasingly focus on the correlations between dietary pattern and chronic diseases to overcome the limitations of traditional single-nutrient studies because ''food'' does not contain a single nutrient but is a combination of nutrients and non-nutrients that interact [13]. In this regard, several nutritional epidemiologists have tried to identify dietary patterns by countries because unique dietary patterns possibly can influence the chronic disease [14]. Clearly, there was a unique dietary pattern existed in Korea but also has modified, along with western dietary culture. Up to this date, many studies have reported associations between dietary patterns and MS [15]. Even though there were several reports that the body composition changes in aging increased the risk of metabolic disorder, there were few studies which directly examined the effects of dietary patterns and body composition changes on Korean elderly [16]. Therefore, this study classified current dietary patterns with nutrient intake for Korean elderly aged 65 yr or more and investigated associations between body composition factors and dietary patterns.
This study was based on data obtained from the KNHANES 2011, a nationally-representative survey conducted by the Korean Ministry of Health and Welfare. The survey's target population included non-institutionalized Korean civilians. Sampling units consisted of households selected through a stratified, multistage, probability-sampling design, based on geographic area, sex and age group using household registries [17]. KNHANES 2011 consisted of the following four components: a health interview survey, a health behaviors survey, a health examination survey, and a nutrition survey. Among 10,589 individuals, subjects who were aged 65 yr or more and who had participated in the health examination survey as well as the nutrition survey were included in this study. We excluded those who reported implausibly low or high daily energy intakes (< 500 kcal day_1 or > 5,000 kcal day_1), resulting in a final analytical sample of 1,435 subjects.
Health examination and dietary measurement height, weight, and waist circumference (WC) were obtained using standardized techniques and calibrated equipment. BMI was calculated by dividing weight by height squared. Blood pressure was measured by standard methods, using a sphygmomanometer with the subject in a sitting position. Three measurements were made on all subjects at 5-min intervals, and the average of the second and third measurements was used in the analysis. Blood samples were collected in the morning after having fasted for at least 8 h. Fasting glucose, total cholesterol, triglycerides were analyzed in a central, certified laboratory. The DXA (Dual-Energy X-Ray Absorptiometry) scan was performed for each subject to measure total body fat mass and total body fat percentage using fan-beam technology (Lunar Corp., Madison, WI). A general questionnaire was administered for basic demographic and health-related information. Socio-demographic factors such as age, gender, education, smoking, and physical activity were chosen as confounding factors [18]. Smoking status was attained by asking whether he/she currently smoked, and physical activity data were gathered by asking whether he/she engaged in physical activity at least 3 days or more per week and lasting at least 20 min or more at moderate intensity over the previous week. Dietary intake was measured by the single 24-h dietary recall method. Trained staff instructed the respondents to recall and describe all the foods and beverages they had consumed in the previous day. Food models and measuring bowls, cups and spoons were used to assist in estimating portion sizes.
Appendicular skeletal muscle mass (ASM) was measured by DXA. ASM was defined as the sum oflean soft tissue masses for the arms and legs, after the method of Heymsfield et al. [19]. International Obesity Task Force (IOTF) and the WHO Regional Office for the Western Pacific Region recommend using the definition of obesity in Asians as those with BMI 25 (kg/m2). Thus, a subject was classified as obese if his or her BMI was 25 or higher according to the standard of IOTF, WHO, and KSSO [20].
Dietary data were collected by a 24-h recall, and the food data were categorized into 23 food groups based on common groups classified in the Korean Nutrient Database to simplify the interpretation of components, and the percentage of total energy intake was determined from each food group. Grains and their products accounted for almost half of daily energy intake; hence, this food group was further divided into four subgroups to address the following types of staple foods: white rice, other grains, noodles and dumpling, and flour and bread. Kimchi (traditional fermented cabbage) was also separated into a single group because it is a traditional Korean side dish [21]. The dietary patterns were derived by cluster analysis using the k-means algorithm. Three clusters were examined for sensible patterns and labeled by descriptive names based on the predominant food groups. The Korean diet typically consists of white rice, soup and side dishes with plenty of plant foods, and is characterized as a low-fat and high-vegetable diet [21]. About 40% of the subjects were assigned to a 'Traditional Korean' dietary pattern, in which consumption of white rice accounted for 76.21% of total energy intake. Then, 19.65% of subjects were assigned to a 'Meat and Alcohol' dietary pattern because they had a higher consumption of meat and alcohol. The other 42.86% of the subjects were assigned to a 'Westernized Korean' dietary pattern, which was based on a rice and vegetable diet but was characterized by a variety of food groups such as other grains, fruit, bread, eggs, fish, milk, and alcohol.
All statistical analyses were conducted using SPSS version 20.0 (SPSS, IBM, NY, USA). The dietary patterns were derived by cluster analysis using the k-means algorithm. Basic characteristics were tested using chi-square tests according to the dietary pattern groups. The generalized linear model was used to test for significant differences in mean values by the dietary pattern groups for biochemical parameters, anthropometric parameters, and nutrient intakes. Logistic regression was used to calculate odds ratios (ORs) with 95% confidence intervals (CIs) for the body composition traits. All models were adjusted for age, gender, education, smoking, and physical activity in all logistic regression models.
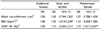
Table 1 shows the key characteristics of the three dietary patterns and nutrient intakes. Thirty seven point forty nine percent of subjects was assigned to 'Traditional Korean' pattern which had its percent daily energy intake (76.21%) solely from white rice, and much lower milk & dairy consumption than other two groups. Nineteenpoint sixty five percent of subjects was assigned to 'Meat & Alcohol' pattern, 42.86% of subjects were assigned to 'Westernized Korean' pattern which had higher consumption of its percent daily energy from noodles (4.21%) and from bread (2.57%) than 'Traditional Korean' pattern. In addition, 'Westernized Korean' pattern received 49.65% of energy from white rice, 9.57% from other grains, which resulted in its percent daily energy intake (66%) from total grain products. Besides consumptions of various food groups include fruit, eggs, fish, milk, meat, legumes, and oil in 'Westernized Korean' pattern were a middle of intake of the other two groups.
There is no difference of consumption of kimchi and vegetable among 3 groups because elderly aged 65 yr or more are likely to have basic Korean meals with kimchi and vegetable. Energy intake was notably different according to the dietary pattern groups, and the 'Traditional Korean' pattern had the lowest in the total energy and fat intake as well. Energy intake calculated by body weight was 25.55 kcal/kg. 24-36 kcal/kg body weight a day was generally recommended for the elderly [22] and we might expect calorie restriction effect in 'Traditional Korean' pattern. Protein and iron intake were higher in 'Meat & Alcohol' pattern. Protein intake per body weight (0.7 g/kg) in the 'Traditional Korean' pattern group was deficient compared with RDA 0.8 g/kg. Calcium intake (299.04 mg/day) in the 'Traditional Korean' pattern was lowest, and the level of calcium intake in all three pattern groups was deficient compared with RDA 700 mg/day.
Demographic characteristics and anthropometric & biochemical parameters which are related with body composition according to the dietary pattern groups are presented in Tables 2 and 3. There are significant differences in education, subject body type recognition, gender, and income among 3 groups. Members of the 'Traditional Korean' pattern were more likely to be older, low educated, low income, low subjective body type recognitionas overweight, and higher physical activity compared with other two groups. Weight, BMI, whole body fat mass, and total cholesterol were significantly different by the dietary pattern groups. 'Traditional Korean' pattern had lower muscle mass, BMI, serum triglyceride levels, and serum ferritin levels and ASM was higher in the 'Meat & Alcohol' pattern whereas fasting blood glucose level was significantly higher in the 'Traditional Korean' pattern. Serum vitamin D influencing body composition was under 20 (ng/mL) and deficient in all three groups. The multivariate-adjusted ORs (95% CI) for body composition were presented in Table 4. In body composition changes, the 'Meat & Alcohol' pattern showed a 50% increased of BMI (P = 0.043), 'Westernized Korean' pattern showed a 74% increased abnormality of ASM/Wt (kg) (P = 0.005), compared with the 'Traditional Korean' pattern. Other factors were not associated with the dietary patterns.
In present study, we classified current dietary patterns with nutrient intake for Korean elderly age 65 yr or more. Three distinctive dietary patterns were identified by cluster analysis. 37.49% was assigned a 'Traditional Korean' dietary pattern with high consumptions of white rice, whereas 19.65% indicated a 'Meat & Alcohol' pattern and the remaining 42.86% showed a 'Westernized Korean' pattern. According to Song et al. [22], the Korean diet is traditionally high in carbohydrate, low in fat, and abundant in vegetables. In this study focused on body composition change, we found that intake of protein, vitamin D, and calcium was low in 'Traditional Korean' pattern. Diet rich in protein, omega 3, vitamin D, calcium, and vitamin C has been reported as having benefits on stimulating protein synthesis and also decreasing inflammation cytokines to maintain body composition. Previous studies suggested the nutrient strategy for healthy body composition in the elderly as follows 1. Energy intake; 24-36 kcal/kg body weight a day and avoidance of extreme over- as well as underweight. 2. Protein intake; 1.0-1.2 g/kg and high quality protein sources at each meal such as milk products, nonfat meat, fish, eggs. 3. Vitamin D intake; 800-1,000 IU/day, regular fish consumption, daily exposure to sunlight and supplementation were required. 4. Calcium intake; 1,000-1,500 mg/day 5. Omega-3; vegetable oils like walnut, and linseed and fatty fish like salmon, mackerel. 5. Vitamin C; 2,000 mg or over/day and diets rich in fruits and vegetables [23,24,25]. In this study, energy intake calculated by average weight was 25.55-31.27 kcal/kg body weight a day which was normal ranges and calcium intake and the serum level of vitamin D were deficient in all three pattern groups. In 2009 Korea National Health and Nutrition Examination Survey, calcium intake is low, with only 50% of elderly aged 65 yr or more achieving the RDA recommended intake levels [26]. Many studies supported that daily calcium intake correlated with total body fat percent negatively and with muscle mass positively [27] and Hong et al. [26] showed serum 25(OH) vitamin D levels was maintained within the normal range with high calcium intake. There is also a growing evidence to support the link between vitamin D deficiency and CVD and MS [28]. Bunout et al. [29] supported the importance of combining vitamin D with calcium to increase muscle mass and physical functioning in older adults. In this study, appendicular skeletal muscle mass and BMI were associated with the dietary patterns. The 'Meat & Alcohol' pattern showed a 50% increased of BMI (P = 0.043) and 'Westernized Korean' pattern showed a 74% increased abnormality of ASM/Wt (P = 0.005) compared with the 'Traditional Korean' pattern. 'Meat & Alcohol' pattern group showed higher intakes of energy and fat compared with the other two groups, causing elevated serum triglyceride level, serum ferritin level, total cholesterol, BMI, ASM, WC, and prevalence of obesity. But one of the interesting findings in this study was 'Traditional Korean' patterns showed lots of healthy factors but it had protein deficiency and low ASM while 'Meat & Alcohol' group had higher intake of protein (1.0/kg) and ASM also higher than other groups. Recently, many studies considered on protein intake at the RDA level which resulted in the loss of muscle in the elderly [30]. Hannan et al. [31] found both total and animal protein intake had association favorably with body composition, bone loss, and fracture risk in the elderly. The Korean diet is traditionally high in plant protein like soybean and soy foods which tend to be deficient in one or more essential amino acids and a source of high-biological-value protein. So, Korean elderly who had easily protein deficiency and decreased muscle mass need to increase intake of animal protein. Considering dietary patterns dominated by red and processed meats caused risks of coronary heart disease, diabetes and metabolic syndrome [16], nutrients such as vitamin B6, vitamin B12, and folic acid must be supplied to avoid accumulation of homocystein and leads to inflammation [32]. Rapid nutrition transitions due to the adoption of a western lifestyle have played a role in increasing with the prevalence of metabolic disorder. However, we found that half of the Korean adult population maintained a 'Traditional Korean' dietary pattern or 'Westernized Korean' dietary pattern in the based their eating on the traditional diet. A western dietary pattern did not emerge in this study. Consumption of kimchi and vegetable was not different among 3 groups because all subject of our study are the elderly age 65 yr or more. These results are not coincidence with other study with 20 yr or more Korean population that the consumption of kimchi and vegetable was higher in traditional pattern than in the other patterns. Probable explanations are that old people who had already established their dietary habits before the western lifestyle was introduced were not affected on western-style diet rather than younger people. For the same reason, consumption of milk products specially was low in 'Traditional Korean' pattern in our study. The prevalence of sarcopenic obesity (SO), a progressive loss of muscle mass and an increase of fat mass, was 18.4% in men and 25.8% in women among adults age 60 of more [32] and the SO could be worsened in the next decade. Up to this date, many studies have reported associations between dietary patterns and MS [15] but no previous study which directly examined the effects of dietary patterns and body composition changes on Korean elderly, even though there were several reports that the body composition changes in aging increased the risk of metabolic disorder [16]. It is well established that body composition changes in aging like loss of muscle mass and increased fat mass can be reversed with nutrients for elderly. So in epigenetic view, we may emphasize the intake of good quality protein such as milk products, non fatty meat, fish, and bean products and other major nutrients intake such as vitamin D, calcium, omega 3, and vitamin C for the elderly. It may be necessary to advise elderly subject to increase protein synthesis and reduce inflammatory mechanism, focusing on dietary patterns with nutrients related with body composition for the maintenance of muscle mass and function and fat mass as well. There were several limitations in this study. First, the cross-sectional design of this study precluded our ability to identify on causal inference between dietary patterns and body composition. Second, all participants in the present study were relatively healthy because those who were admitted to hospital or nursing homes were not included in KNHANES. Therefore, in the present study, the mean values of body composition index by DAX may have been underestimated. Third, physiologically, due to individual differences in elderly with aging process and dietary patterns divided by subjective technique, therefore it might lead to substantial attenuation of the effect of dietary patterns on outcome. The last, at the population level, 24-h recall which might not represent accurate usual intake could be one of another limitation in our study. We could not control for all of epigenetic influence, thus, these results need to be confirmed by additional study with longitudinal data to make it possible to generalize the results. Additional variables or measurement could also be included in future search. Further studies are necessary to explore that to have combining dietary pattern methods to capture overall diet quality and refine practical as well as useful dietary pattern. The unclear aspects of the Korean diet pattern according to high carbohydrate levels and the quality of protein (e.g., animal protein/vegetable protein) as well as the quantity of protein and their relationship to body composition on Korean elderly are necessary to explore as well.
In conclusion, this study identifies three unique dietary patterns in Korean elderly, which are independently associated with certain body composition changes. Our findings suggest that a 'Traditional Korean' dietary pattern has healthy aspects but negatively associated with body composition attributable to a low consumption of protein, calcium and vitamin D compared with other two patterns. Our study could show a need for greater emphasis on nutrients related with body composition and suggested that efforts could be made to improve provision of these nutrient-rich foods and right knowledge for the elderly. Since SO is a life-long process, prevention should be start early with modification of life style specially nutrition. Thus, this study provides justification for Korean elderly to improve the quality of their dietary pattern and good decisions on food. Also strategies to improve the quality of life for the elderly, providing meals with good quality of protein, less fat, and micro nutrients rich food, and developing an interactive and friendly information system could also change meal quality of catering menu in senior center or nursing home.
The Korean traditional dietary pattern modified for a low animal protein, vitamin D, and calcium intake might be a healthy dietary pattern for Korean elderly.
Figures and Tables
References
1. Jung KW, Won YJ, Park S, Kong HJ, Sung J, Shin HR, Park EC, Lee JS. Cancer statistics in Korea: incidence, mortality and survival in 2005. J Korean Med Sci. 2009; 24:995–1003.

2. Zamboni M, Mazzali G, Fantin F, Rossi A, Di Francesco V. Sarcopenic obesity: a new category of obesity in the elderly. Nutr Metab Cardiovasc Dis. 2008; 18:388–395.

3. Roubenoff R. Sarcopenic Obesity: Does Muscle Loss Cause Fat Gain?: Lessons from Rheumatoid Arthritis and Osteoarthritisa. Ann N Y Acad Sci. 2000; 904:553–557.

4. Balagopal P, Proctor D, Sreekumaran Nair K. Sarcopenia and hormonal changes. Endocrine. 1997; 7:57–60.

5. Li Z, Heber D. Sarcopenic obesity in the elderly and strategies for weight management. Nutri Reviews. 2012; 70:57–64.

6. Jackson AA, Burdge GC, Lillicrop K. Diet, nutrition and modulation of genomic expression in fetal origins of adult disease. J Nutrigenet Nutrigenomics. 2011; 3:192–208.

7. Roubenoff R. Catabolism of aging: is it an inflammatory process. Curr Opin Clin Nutr Metab Care. 2003; 6:295–299.

8. Burdge GC, Lillycrop KA. Nutrition, epigenetics, and developmental plasticity: implications for understanding human disease. Ann Rev Nutri. 2010; 30:315–339.

9. Anand P, Kunnumakara AB, Sundaram C, Harikumar KB, Tharakan ST, Lai OS, et al. Cancer is a preventable disease that requires major lifestyle changes. Pharmaceutical Research. 2008; 25:2097–2116.

10. Ilanne-Parikka P, Eriksson JG, Lindström J, Peltonen M, Aunola S, Hämäläinen H, Keinänen-Kiukaanniemi S, Laakso M, Valle TT, Lahtela J, Uusitupa M, Tuomilehto J. Finnish Diabetes Prevention Study Group. Effect of lifestyle intervention on the occurrence of metabolic syndrome and its components in the Finnish Diabetes Prevention Study. Diabetes Care. 2008; 31:805–807.

11. Candow DG, Forbes SC, Little JP, Cornish SM, Pinkoski C, Chilibeck PD. Effect of nutritional interventions and resistance exercise on aging muscle mass and strength. Biogerontology. 2012; 13:345–358.

12. Chung JY, Hong SH. Vitamin D status and its association with cardiometabolic risk factors in Korean adults based on a 2008-2010 Korean National Health and Nutrition Examination Survey. Nutr Res Pract. 2013; 7:495–502.

14. Sánchez-Villegas A, Delgado-Rodriguez M, Martínez-González MÁ, De Irala-Estevez J. Gender, age, socio-demographic and lifestyle factors associated with major dietary patterns in the Spanish Project SUN (Seguimiento Universidad de Navarra). Euro J Clin Nutr. 2003; 57:285–292.

15. Lee JE, Kim JH, Son SJ, Ahn Y, Lee J, Park C, Lee L, Erickson KL, Jung IK. Dietary pattern classifications with nutrient intake and health-risk factors in Korean men. Nutrition. 2011; 27:26–33.

16. Heidemann C, Schulze MB, Franco OH, van Dam RM, Mantzoros CS, Hu FB. Dietary patterns and risk of mortality from cardiovascular disease, cancer, and all causes in a prospective cohort of women. Circulation. 2008; 118:230–237.

17. Korean National Health Examination and Nutrition Survey 2011. cited 2013 December 20. Available from: https://knhanes.cdc.go.kr.
18. Park HS, Oh SW, Cho S-I, Choi WH, Kim YS. The metabolic syndrome and associated lifestyle factors among South Korean adults. Inte J Epid. 2004; 33:328–336.

19. Heymsfield SB, Smith R, Aulet M, Bensen B, Lichtman S, Wang J, Pierson RN Jr. Appendicular skeletal muscle mass: measurement by dual-photon absorptiometry. Amer J Clin Nutri. 1990; 52:214–218.

21. Song Y, Joung H, Engelhardt K, Yoo SY, Paik HY, Traditional v. modified dietary patterns and their influence on adolescents' nutritional profile. British J Nutr. 2005; 93:943–950.
22. Song Y, Joung H. A traditional Korean dietary pattern and metabolic syndrome abnormalities. Nutr Metab Cardiovasc Dis. 2012; 22:456–462.

23. Volkert D. The role of nutrition in the prevention of sarcopenia. Wien Med Wochenschr. 2011; 161:409–415.

24. Lee MJ, Popkin BM, Kim S. The unique aspects of the nutrition transition in South Korea: the retention of healthful elements in their traditional diet. Publ Health Nutr. 2002; 5:197–204.

25. Mithal A, Bonjour J-P, Boonen S, Burckhardt P, Degens H, El Hajj Fuleihan G, Josse R, Lips P, Morales Torres J, Rizzoli R, Yoshimura N, Wahl DA, Cooper C, Dawson-Hughes B. IOF CSA Nutrition Working Group. Impact of nutrition on muscle mass, strength, and performance in older adults. Osteoporos Int. 2012; 1–12.

26. Hong H, Kim EK, Lee JS. Effects of calcium intake, milk and dairy product intake, and blood vitamin D level on osteoporosis risk in Korean adults: analysis of the 2008 and 2009 Korea National Health and Nutrition Examination Survey. Nutr Res Prac. 2013; 7:409–417.

27. Melanson EL, Donahoo WT, Dong F, Ida T, Zemel MB. Effect of Low-and High-Calcium Dairy-Based Diets on Macronutrient Oxidation in Humans. Obesity Research. 2005; 13:2102–2112.

28. Holick MF. Vitamin D: Importance in the prevention of cancers, type 1 diabetes, heart disease, and osteoporosis. Am J Clin Nutr. 2004; 79:362–371.

29. Bunout D, Barrera G, Leiva L, Gattas V, de la Maza MP, Avendaño M, Hirsch S. Effects of vitamin D supplementation and exercise training on physical performance in Chilean vitamin D deficient elderly subjects. Exp Gerontol. 2006; 41:746–752.

30. Volpi E, Campbell WW, Dwyer JT, Johnson MA, Jensen GL, Morley JE, Wolfe RR. Is the optimal level of protein intake for older adults greater than the tecommended dietary allowance? J Gerontol A Biol Sci Med Sci. 2013; 68:677–681.

31. Hannan MT, Tucker KL, Dawson-Hughes B, Cupples LA, Felson DT, Kiel DP. Effect of dietary protein on bone loss in elderly men and women: the Framingham Osteoporosis Study. J Bone Miner Res. 2000; 15:2504–2512.

32. Kruman II, Kumaravel T, Lohani A, Pedersen WA, Cutler RG, Kruman Y, Haughey N, Lee J, Evans M, Mattson MP. Folic acid deficiency and homocysteine impair DNA repair in hippocampal neurons and sensitize them to amyloid toxicity in experimental models of Alzheimer's disease. J Neurosci. 2002; 22:1752–1762.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download