Abstract
The purpose of this study was to assess vitamin B6 intake and status in Korean patients with newly diagnosed type 2 diabetes. Sixty-four patients with newly diagnosed type 2 diabetes and 8-11% glycated hemoglobin (A1C), along with 28 age-matched non-diabetic subjects, participated. Dietary vitamin B6 intake was estimated by the 24 hour recall method and plasma pyridoxal 5'-phosphate (PLP) was measured. There was a significant difference in daily total calorie intake between the diabetic and non-diabetic groups (1,917 ± 376 vs 2,093 ± 311 kcal). There were no differences in intake of total vitamin B6 (2.51 ± 0.91 vs 2.53 ± 0.81 mg/d) or vitamin B6/1,000 kcal (1.31 ± 0.42 vs 1.20 ± 0.32 mg) between the diabetic and non-diabetic groups, andI intakes of total vitamin B6 were above the Korean RDA in both groups (180.0 ± 57.9 vs 179.0 ± 65.4). There was a higher percentage of diabetic subjects whose plasma PLP concentration was < 30 nmol/L compared to non-diabetic group. Plasma PLP levels tended to be lower in the diabetic subjects than in the non-diabetic subjects, although the difference was not statistically significant due to a large standard deviation (80.0 ± 61.2 nmol/L vs 68.2 ± 38.5 nmol/L). Nevertheless, plasma PLP levels should be monitored in pre-diabetic patients with diabetic risk factors as well as in newly diagnosed diabetic patients for long-term management of diabetes, even though this factor is not a major risk factor that contributes to the development of degenerative complications in certain patients.
In developed countries, classical vitamin-deficiency syndromes such as scurvy, beriberi, and pellagra are now uncommon, but specific population subgrozups remain at risk for modest vitamin insufficiencies. This is notably the case in diabetes patients who frequently display inadequate vitamin status, including many from the B group. Diabetes mellitus is a metabolic disorder characterized by hyperglycemia and insufficiency of secretion or action of endogenous insulin. Although the etiology of diabetes is not well defined, aging is a major factor in the development and progression of diabetes. Due to functional insufficiency, the vitamin B6 status of elderly individuals may be subject to higher variability than that of younger adults who are frequently taken as references. Moreover, it is reported that plasma PLP level is affected by age and gender [1].
It has been reported that vitamin B6 may be involved in the metabolism of carbohydrate. Pyridoxal 5'-phosphate (PLP), the active form of vitamin B6, acts as an integral part of glycogen phosphorylase (EC 2.4.1.1.) which catalyzes the breakdown of glycogen [2]. A deficiency of vitamin B6 is associated with impaired gluconeogenesis [3] and impaired glucose tolerance [4]. It has also been reported that vitamin B6 deficiency can lead to a decrease in the level of circulating insulin as well as pancreas function and relates to increased risk of coronary artery disease in animal models [5,6]. Thus, proper vitamin B6 status can be deemed an important factor in the care of type 2 diabetes for the prevention of degenerative complications. However, there have been few reports on vitamin B6 status in the Korean elderly population or in those with diabetes.
Therefore, the aim of the present study was to assess vitamin B6 status using plasma PLP levels and vitamin B6 intakes of Korean patients with newly diagnosed type 2 diabetes since plasma PLP level [7,8] and vitamin B6 intake have been the most accepted and widely used indices of vitamin B6 status in the last decade. In addition, these status indices were compared to those of age and gender-matched healthy non-diabetic subjects to exclude variance from age, as well as gender effects.
Sixty-four patients with newly diagnosed type 2 diabetes and 8-11% glycated hemoglobin (A1C), which is used primarily to identify average plasma glucose concentrations over a prolonged period of time, and 28 age-matched healthy non-diabetic subjects were recruited consecutively from the diabetes clinic at E Hospital between February and April, 2005. Subjects were excluded before recruitment if they were taking supplemental vitamins, including multivitamins.
Dietary vitamin B6 intake and food sources were estimated with the 24 hour recall method. The subjects each reported three consecutive daily dietary intakes with the help of a trained interviewer. Food portion sizes were estimated by using standard household measures and published average portion sizes [9]. Nutrient intakes were estimated using a computer-aided nutritional analysis program developed by the Korean Nutrition Society [10]. When information was unavailable for a particular food, a value was assigned based on values for similar foods. The foods in the vitamin B6 database were categorized into those of animal or plant origin, and the amount of daily vitamin B6 provided by these two categories was calculated for each person. On the day of dietary data collection, weights and heights were measured and body mass index (BMI) was calculated from the measurements of body weight and height.
After a 12-hour fast, venous blood was used for the assessment of vitamin B6 status and biochemical indices. Immediately following blood draw into heparinized vacutainers, the blood was centrifuged at 3,000 rpm for 15 min to separate the plasma. The plasma was stored at -20℃ in aliquots until analyzed. Plasma PLP concentration was measured using the HPLC method [11], which was modified as follows: Mobile phase (0.1 M potassium dihydrogen phosphate containing 0.1 M sodium perchlorate, 0.5 g/L sodium bisulfite, pH 3) was pumped at a flow rate of 1.0 ml/min into the column (Bondapack ODS column, 3.9×300 mm, 10 µm porus packing, C18, Waters). The plasma was added to perchloric acid (0.8 M) and allowed to sit for one hour to release PLP from the protein. This mixture was then centrifuged (18,000 rpm, 4℃, 15 min) and the supernatant removed. One hundred microliters of supernatant was loaded in the sample loop and then injected into the column.
Statistical analyses were carried out using the Statistical Analysis System (SAS). Pearson's correlation coefficient was used to determine possible relationships among the indices of vitamin B6 status and blood biochemical indices. Values for vitamin B6 status were regressed based on vitamin B6 intake and dietary vitamin B6 to protein ratio.
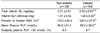
Because aging is one of the major factors affecting both plasma PLP levels and the development and progression of diabetes, comparisons of plasma PLP concentrations of diabetic patients to those of age-matched healthy non-diabetic subjects are important. Sixty-four diabetic patients and 28 age-matched non-diabetic subjects participated in this study, with mean age being 50 years for the diabetic patients and 51.5 years for the non-diabetic subjects. The characteristics of the subjects are given in Table 1. Table 2 shows the nutrient intakes of the diabetic patients and non-diabetic subjects. There was a significant difference in daily total calorie intake between the diabetic and non-diabetic groups (1,917 ± 376 vs 2,093 ± 311 kcal/d) due to excess weight in the diabetic subjects. However, there were no differences in intakes of other nutrients including vitamin B6. Table 3 shows dietary vitamin B6 intake and plasma PLP levels for the non-diabetic and diabetic subjects. There were no differences in intake of total vitamin B6 (2.51 ± 0.91 vs 2.53 ± 0.81 mg/d) or vitamin B6/1,000 kcal (1.31 ± 0.42 vs 1.20 ± 0.32 mg) between the diabetic and non-diabetic groups. The intakes of total vitamin B6 were above the Korean RDA for both groups. In the diabetic patients, the mean plasma PLP level was 15% lower as compared to the non-diabetic subjects (80.0 ± 61.2 vs 68.2 ± 38.5 nmol/L), but this difference was not statistically significant due to a large standard deviation. This indicates that the percentage of diabetic subjects whose plasma PLP concentration was < 30 nmol/L was higher than that of the non-diabetic group. Fig. 1 shows the frequency distribution of daily vitamin B6 intake, and its relative intake to daily protein intake ratio. Daily vitamin B6 intake was not normally distributed in either the non-diabetic or diabetic subjects, and the declination was steeper in the diabetic patients. Fig. 2 shows there was no significant correlation between plasma PLP level and intake of vitamin B6 in either the non-diabetic subjects or diabetic patients. Also, plasma PLP levels and intakes of vitamin B6 were more widely scattered in the diabetic patients compared to the non-diabetic subjects. Table 4 shows that no significant correlations were found between plasma PLP level and biochemical risk indices including plasma levels of fasting glucose, postprandial glucose, triglyceride, albumin, and total cholesterol in either the non-diabetic subjects or diabetic patients.
Because there were no differences in total vitamin B6 intake and vitamin B6/1,000 kcal between the diabetic and non-diabetic groups, it is considered that the higher energy intake in diabetes patients did not affect intake of vitamin B6. A possible explanation for the tendency of lower vitamin B6 status is based on plasma PLP level, which has been suggested as the best single status indicator because it appears to reflect tissue stores. In the diabetic subjects, the mean plasma PLP level was 15% lower than that of the non-diabetic subjects (80.0 ± 61.2 nmol/L vs 68.2 ± 38.5 nmol/L), but this difference was not statistically significant due to a large standard deviation.
However, even though there were no differences in total vitamin B6 intake and vitamin B6/1,000 kcal between the diabetic and non-diabetic groups, and intakes of total vitamin B6 were above the Korean RDA in both groups, the percentage of subjects with a plasma PLP concentration < 30 nmol/L (the proposed cutoff as an index of adequacy in diabetic patients) was higher in the diabetic subjects as compared to non-diabetic subjects. Also, plasma PLP levels and intakes of vitamin B6 were more widely scattered in the non-diabetic group as compared to those of the diabetic group. Thus, if an eccentric value were considered, the 15% lower mean plasma PLP level in the diabetic subjects compared to that of the non-diabetic subjects is thought to be a meaningful decrease in a clinical situation, although this difference was not statistically significant. In addition, the results of this study are consistent with previous studies where circulating levels of plasma pyridoxal 5'-phosphate and total vitamin B6 significantly decreased under conditions of hyperglycemia [12-14].
However, recent epidemiology of plasma PLP in the U.S. population showed there was no difference between diabetes and non-diabetes subjects, regardless of using supplemental vitamin B6 [15]. This discrepancy may be explained by differences in major vitamin B6 sources, because several studies have indicated that the utilization of vitamin B6 from animal derived foods is more efficient than that from plant foods [16,17]. Furthermore, it was reported that Koreans obtain approximately 65% of vitamin B6 from plant sources [18,19], whereas in the American diet, approximately 50% of dietary vitamin B6 is from meat and the other 50% is from plant-based foods [20].
There was a previous review on age-associated B vitamin deficiency as a determinant of chronic diseases [21], and estimations of how much vitamin B6 is required in diabetes must take into account all potential age-related alterations. By the comparison of vitamin B6 status in diabetic patients to that of age-matched healthy non-diabetic subjects in this study, the tendency for a lower plasma PLP level in diabetic patients might not be due to age-related alterations.
This lowered level of plasma PLP in diabetic patients may be due to either lower intake of vitamin B6 or altered distribution of PLP in diabetic patients. B vitamin intake is dependent on the food supply and many studies have demonstrated that increased protein intake causes a relative decrease in B6 status, as judged by a variety of B6 status indicators [22-24]. Furthermore, in this study, vitamin B6 intake was highly correlated to intakes of energy and protein. This has led some to define B6 requirements in terms of protein intake or energy intake. However, there was no difference in vitamin B6 intake when expressed as either a ratio of vitamin B6 intake to daily protein intake or as the amount of vitamin B6 intake to a 1,000 calorie intake in this study. These data show that plasma PLP levels tended to be lower in the diabetic subjects than in the non-diabetic subjects although there was no difference in vitamin B6 intake. Thus, in this study, the lower plasma PLP levels of the diabetic patients might not have been due to insufficient intake of vitamin B6, but instead might be due to altered distribution of PLP in diabetic patients.
The mechanism involved in altered distribution of PLP in diabetes could be that elevated plasma glucose reduces plasma PLP levels and xanthurenic acid excretion due to abnormal tryptophan metabolism; xanthurenic acid forms xanthurenic acid-insulin complexes that reduce insulin sensitivity and result in elevated blood glucose levels [25]. Decreases of mitochondria pyridoxal phosphate and aspartate aminotransferase have been observed in diabetic animals [26]. It was also reported that urinary excretions of 3-hydroxykynurenine and 3-hydroxyanthranilic acid were increased in diabetic animals, and this might lead to the inhibition of islet insulin secretion [27].
In clinical situations, the question still remains whether altered distribution of PLP contributes to the development of degenerative complications, or results from those complications. Because no significant correlations were found between plasma PLP levels and any of the biochemical risk indices of degenerative diabetes complications, such as plasma levels of fasting glucose, postprandial glucose, triglyceride, albumin, and total cholesterol, in either the non-diabetic or diabetic subjects of this study, the cause-effect nature of this relationship could not be clarified. However, considering the major complications that occur in diabetic patients, maintaining normal vitamin B6 status is an important diet strategy for diabetic patients since retrospective studies have suggested the association between risk of cardiovascular disease and vitamin B6 status, although the cause-effect nature of this relationship has not been clarified [28-31]. Prospective studies also suggest that populations with higher PLP concentrations have lower risk of coronary heart disease [32,33].
Therefore, despite the many uncertainties regarding the mode of action, these results suggest that plasma PLP levels should be monitored in pre-diabetic patients with diabetic risk factors and in newly diagnosed diabetic patients for long-term management of diabetes, even though this factor is not a major risk factor that contributes to the development of degenerative complications in certain patients. The principal limitations of this study were the cross-sectional design and that a causative nature of the association could not be established.
Figures and Tables
Fig. 1
Distribution of vitamin B6 intake in non-diabetic and diabetic1) subjects. 1) Diabetic subjects had newly diagnosed type 2 diabetes with 8-11% A1C and non diabetic subjects were age-matched.

Fig. 2
Scatter plots of plasma PLP levels and vitamin B6 intake in non-diabetic and diabetic1) subjects. 1) Diabetic subjects had newly diagnosed type 2 diabetes with 8-11% A1C and non diabetic subjects were age-matched.

References
1. Cho YO. Vitamin B6 requirement: Indicators and factors affecting. Korean J Nutr. 2010. 43:315–323.

2. Krebs EG, Fischer EH. Phosphorylase and related enzymes of glycogen metabolism. Vitam Horm. 1964. 22:399–410.

4. Rose DP, Leklem JE, Brown RR, Linkswiler HM. Effect of oral contraceptives and vitamin B6 deficiency on carbohydrate metabolism. Am J Clin Nutr. 1975. 28:872–878.

5. Huber AM, Gershoff SN, Hegsted DM. Carbohydrate and fat metabolism and response to insulin in vitamin B6-deficient rats. J Nutr. 1964. 82:371–378.

6. Makris A, Gershoff SN. Insulin sensitivity in vitamin B6-deficient rats. Effects of acute and chronic growth hormone treatment. Nutr Metab. 1974. 16:337–351.
8. Mason JB. Biomarkers of nutrient exposure and status in one-carbon (methyl) metabolism. J Nutr. 2003. 133:941S–947S.

9. Korean Dietetic Association. Food exchange list. 1995. Seoul:
10. The Korean Nutrition Society. Computer Aided Nutritional analysis program for Professionals 3.0 [Computer software]. 2005. Seoul:
11. Kimura M, Kanehira K, Yokoi K. Highly sensitive and simple liquid chromatographic determination in plasma of B6 vitamers, especially pyridoxal 5'-phosphate. J Chromatogr A. 1996. 722:295–301.

12. Okada M, Shibuya M, Yamamoto E, Murakami Y. Effect of diabetes on vitamin B6 requirement in experimental animals. Diabetes Obes Metab. 1999. 1:221–225.

13. Rogers KS, Higgins ES, Kline ES. Experimental diabetes causes mitochondrial loss and cytoplasmic enrichment of pyridoxal phosphate and aspartate aminotransferase activity. Biochem Med Metab Biol. 1986. 36:91–97.

14. Leklem JE, Hollenbeck CB. Acute ingestion of glucose decreases plasma pyridoxal 5'-phosphate and total vitamin B-6 concentration. Am J Clin Nutr. 1990. 51:832–836.

15. Morris MS, Picciano MF, Jacques PF, Selhub J. Plasma pyridoxal 5'-phosphate in the US population: the National Health and Nutrition Examination Survey, 2003-2004. Am J Clin Nutr. 2008. 87:1446–1454.

16. Gregory JF 3rd. Nutritional properties and significance of vitamin glycosides. Annu Rev Nutr. 1998. 18:277–296.

17. Kabir H, Leklem JE, Miller LT. Comparative vitamin B6 bioavailability from tuna, whole wheat bread and peanut butter in humans. J Nutr. 1983. 113:2412–2420.

18. Cho YO, Kim BY. Evaluation of vitamin B6 status and RDA in young Koreans. Ann Nutr Metab. 2004. 48:235–240.

19. Cho YO, Yun MK. Estimation of vitamin B6 intake and major dietary sources of vitamin B6 in elderly Koreans in the Seoul area. J Food Sci Nutr. 2004. 9:85–91.

20. Kant AK, Block G. Dietary vitamin B-6 intake and food sources in the US population: NHANES II, 1976-1980. Am J Clin Nutr. 1990. 52:707–716.

21. Brachet P, Chanson A, Demigné C, Batifoulier F, Alexandre-Gouabau MC, Tyssandier V, Rock E. Age-associated B vitamin deficiency as a determinant of chronic diseases. Nutr Res Rev. 2004. 17:55–68.

22. Baker EM, Canham JE, Nunes WT, Sauberlich HE, McDowell ME. Vitamin B6 requirement for adult men. Am J Clin Nutr. 1964. 15:59–66.
23. Miller LT, Leklem JE, Shultz TD. The effect of dietary protein on the metabolism of vitamin B-6 in humans. J Nutr. 1985. 115:1663–1672.

24. Hansen CM, Leklem JE, Miller LT. Vitamin B-6 status of women with a constant intake of vitamin B-6 changes with three levels of dietary protein. J Nutr. 1996. 126:1891–1901.
25. Rogers KS, Mohan C. Vitamin B6 metabolism and diabetes. Biochem Med Metab Biol. 1994. 52:10–17.
26. Nanbara S, Tanaka K, Koide H, Tanaka T, Hayashi T. Changes on levels of B6 vitamin and aminotransferase in the liver of diabetic animals. Diabetes Res Clin Pract. 1990. 9:109–114.

27. Akarte N, Shastri N. Studies on niacin biosynthesis from 3-hydroxyanthranilic acid in streptozotocin diabetic rats in vivo and in vitro. J Nutr Sci Vitaminol (Tokyo). 1976. 22:175–179.

28. Kok FJ, Schrijver J, Hofman A, Witteman JC, Kruyssen DA, Remme WJ, Valkenburg HA. Low vitamin B6 status in patients with acute myocardial infarction. Am J Cardiol. 1989. 63:513–516.
29. Vermaak WJ, Barnard HC, Potgieter GM, Theron HD. Vitamin B6 and coronary artery disease. Epidemiological observations and case studies. Atherosclerosis. 1987. 63:235–238.
30. Selhub J, Jacques PF, Wilson PW, Rush D, Rosenberg IH. Vitamin status and intake as primary determinants of homocysteinemia in an elderly population. JAMA. 1993. 270:2693–2698.

31. Verhoef P, Stampfer MJ, Buring JE, Gaziano JM, Allen RH, Stabler SP, Reynolds RD, Kok FJ, Hennekens CH, Willett WC. Homocysteine metabolism and risk of myocardial infarction: relation with vitamins B6, B12, and folate. Am J Epidemiol. 1996. 143:845–859.





 PDF
PDF ePub
ePub Citation
Citation Print
Print





 XML Download
XML Download