Abstract
This study examines the combined effects of caloric restriction on body composition, blood lipid, and satiety in slightly overweight women by varying food density and aerobic exercise. Twenty-three women were randomly assigned to one of two groups for a four-week weight management program: the high-energy density diet plus exercise (HDE: n = 12, 22 ± 2 yrs, 65 ± 7 kg, 164 ± 5 cm, 35 ± 4 % fat) and low-energy density diet plus exercise (LDE: n = 11, 22 ± 1 yrs, 67 ± 7 kg, 161 ± 2 cm, 35 ± 4 % fat) groups. Subjects maintained a low-calorie diet (1,500 kcal/day) during the program. Isocaloric (483 ± 26 for HDE, 487 ± 27 kcal for LDE) but different weight (365 ± 68 for HDE, 814 ± 202 g for LDE) of lunch was provided. After lunch, they biked at 60% of maximum capacity for 40 minutes, five times per week. The hunger level was scaled (1: extremely hungry; 9: extremely full) at 17:30 each day. Before and after the program, the subjects' physical characteristics were measured, and fasting blood samples were drawn. The daily energy intake was 1,551 ± 259 for HDE and 1,404 ± 150 kcal for LDE (P > 0.05). After four weeks, the subjects' weights and % fat decreased for both LDE (-1.9 kg and -1.5%, P < 0.05) and HDE (-1.6 kg and -1.4%, respectively, P < 0.05). The hunger level was significantly higher for HDE (2.46 ± 0.28) than for LDE (3.10 ± 0.26) (P < 0.05). The results suggest that a low-energy density diet is more likely to be tolerated than a high-energy density diet for a weight management program combining a low-calorie diet and exercise, mainly because of a reduced hunger sensation.
The obesity epidemic has been widely recognized as a major public concern, and thus, a number of researchers and public agencies have advocated the urgent need for weight management strategies [1,2]. Although many studies have surveyed and examined acute and long-term weight loss programs, it has been widely acknowledged that a long-term weight management program is difficult to achieve [3,4].
Previous studies have found that weight loss and maintenance are closely associated with changes in dietary intake, including (but not limited to) decreases in total energy intake [5-7] as well as in dietary fat intake [8,9]. However, most of the previous studies have found that decreasing energy intake and the amount of food (and food choices) can increase the sensation of hunger and the level of dissatisfaction and thus increase the likelihood of weight loss failure or weight regain [10,11]. Exercise and physical activity have been associated with effective long-term weight management because they can increase energy expenditure [3,12]. However, previous research has found considerable differences in individuals' responses to physical activity for maintaining and losing weight [3]. Restricting dietary intake and engaging in physical activity have been suggested as the key to achieving a desired weight management goal [1,13].
The energy deficit from only caloric restriction and that from caloric restriction with physical activity have been found to be similar, and their effects on the magnitude of weight change have also been found to be similar [14-16]. However, the effect of a negative energy balance on weight loss may depend on the magnitude of energy restriction. For instance, if energy restriction is not severe, weight loss from a negative energy balance with caloric restriction and physical activity can be significantly greater than that from a negative energy balance with only caloric restriction [17]. Thus, increasing daily physical activity and restricting dietary intake may be an efficient method of weight loss when caloric restriction is moderate.
A dietary strategy for reducing energy density has recently been proposed. This strategy can minimize the sensation of hunger resulting from caloric restriction and thus can enhance the likelihood of the individual continuing his or her weight management program [18,19]. By selecting low-energy density foods, a greater amount of food can be consumed for the same number of calories. Further, it has been demonstrated that feeling full is more likely to make a person stop eating than the total caloric content of the food consumed [6]. Previous studies have shown that the energy density of food can affect energy intake, satiety, and body weight [20-22] and indicated that a decrease in dietary energy density can reduce energy intake [6,23,24]. Some studies lasting more than six months have found that weight loss can be three times greater for individuals consuming low-energy density foods (low in fat) than for those simply consuming low-fat foods [22]. It has been widely known that regular exercise can reduce body weight for most individuals [1,3]. When implementing weight management programs, modifying the energy balance is essential, and this can be achieved by manipulating the diet and/or increasing energy expenditure (e.g., exercise). However, no study has examined the combined effects of dietary energy density with exercise on weight change.
Thus, the present study investigates the effects of dietary energy density with moderate aerobic exercise on weight change and satiety by using a sustainable weight management program that allows individuals to experience moderate levels of energy restriction and exercise intensity.
A four-week weight management program was developed. All of the subjects took part in the program, which modified the diet to reduce energy intake and incorporated an aerobic exercise session to elevate energy expenditure. The subjects were divided into two groups and given instructions on how they could maintain a low-calorie diet (1,500 kcal/day) during the study. For their lunch, both groups were provided an isocaloric diet (500 kcal). However, one group consumed low-energy density meals, whereas the other consumed high-energy density ones. Their blood lipid profiles and satiety were compared both before and after the program. The study spanned from September to November.
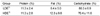
A total of 23 young women considered to be slightly overweight (> 30% body fat) were recruited for the study. They had not participated in any diet or regular exercise program for at least three months prior to the study. They were instructed to report any problems that could affect their participation in the study (e.g., metabolic, cardiovascular, orthopedic, or eating problems). All the procedures and requirements were explained, and they voluntarily signed an informed consent form. They were randomly divided into two groups: the low-energy density diet plus exercise (LDE: n = 11) and high-energy density diet plus exercise (HDE: n = 12) groups. However, they were not informed about the group to which they were assigned. Table 1 shows the subjects' morphological characteristics.
A preliminary dietary intake assessment using three-day dietary recall was conducted, and their dietary behavior was evaluated. Based on their records, they were told to restrict their energy intake to 1,500 kcal/day by consuming approximately 500 kcal per meal. Low-energy density food was defined as 0.6 kcal/g, whereas high-energy density food was 1.4 kcal/g. Each group was provided with some sample foods. For LDE, reducing fat intake and choosing carbohydrate- and/or water-rich foods (e.g., boiled eggs, tomatoes, low-fat yogurt, fruits, and vegetables) were encouraged. Cookies, rice cakes, and fat-rich items were recommended to HDE. To verify their energy intake and food weight, the subjects were instructed to keep dietary records indicating types of foods consumed, portions, the location at which each meal was consumed, and time spent eating, among others. In addition, they recorded the level of their perceived hunger before dinner at 17:30 [18]. This information was obtained through communication between the subjects and the investigator by mobile phone messages on a real-time basis.
Lunch was provided to the subjects during weekdays (i.e., five days a week). For both groups, an isocaloric diet (487 ± 27 kcal for LDE and 483 ± 26 kcal for HDE) was provided. However, the amounts of food differed: 814 ± 202 g for LDE and 365 ± 68 g for HDE (P < 0.05). For example, a lunch for LDE was composed of sweet potato 200 g, apple 200 g, cucumber 100 g, cherry tomato 250 g, and low fat milk 200 ml which was equivalent of 485 kcal, while that for HDE was composed of cereal 60 g, whole milk 200 ml, and apple 100 g, equivalent of 483 kcal. The energy density for the lunch program was approximately 0.6 kcal/g for LDE and 1.3 kcal/g for HDE. Each lunch meal was weighed (Tanita, Japan), and its caloric value was calculated. The subjects were encouraged to consume all the food provided. If they did not finish, the leftover was weighed and calculated for the energy intake. Their lunch was supplied in blind, and each group was unaware of the composition of the other's lunch.
After each lunch, all the subjects took part in aerobic exercise sessions in which they exercised on a stationary bike at 60% of their estimated maximal heart rate for 40 minutes. The target heart rate was calculated as [(220-age)-resting heart rate] × 0.6 + resting heart rate. This protocol was selected because this intensity was assumed to be a moderate to vigorous activity and that the duration could be greater than 200 minutes per week [3]. The subjects maintained the cadence of 60 rpm following an electric metronome. Both before and after each session, the subjects warmed up and cooled down for 10 minutes each. In the first week, the workload was adjusted to match the individual's exercise intensity and readjusted in Week 3. This readjustment was done because of changes in the fitness level as a result of the physical training. Exercise intensity was monitored throughout the sessions by the investigators. The subjects were instructed not to engage to any other exercise programs or vigorous activities beyond the daily routine over the course of the study.
Both before and after the program, the subjects' physical characteristics such as their height, weight (DS-102, Dong Sahn Jenix, Korea), body fat content (using a bioelectrical impedance method, InBody 3.0, Biospace, Korea), and waist/hip girth were measured. The body mass index was calculated as kg/m2. Blood samples were collected twice from antecubital veins after 12 hours of overnight fasting both before and after the program. The 5 ml sample of whole blood was centrifuged at 3,000 rpm for 10 minutes. The serum was separated and stored at -36℃ for later analysis. The samples were analyzed for triglycerides (TG), total cholesterol (TC), and high-density lipoprotein cholesterol (HDL-C) by enzymatic colorimetric methods (Vistalab Selectra, Merck, Germany). Low-density lipoprotein cholesterol (LDL-C) was calculated using Friedewald et al. [25]'s formula. Blood glucose before and two hours after each lunch was measured (Ektachem DT60 II, Kodak, USA). The dietary records were analyzed to confirm the energy value and weight of food consumed each week by using CAN-pro 3.0 (Korean Nutrition Society, Korea). A nine-point Likert scale was used for perceived satiety; 1: extremely hungry, 9: extremely full.
The data were analyzed using SPSS 14.0 for Windows. All the values were expressed as means and standard deviations. The pre- and post-testing results for each group were compared using the paired t-test, and the differences between the groups were compared using the independent t-test. The results were examined for their statistical significance (P < 0.05).
All the subjects complied with the study requirements, that is, they followed the required dietary and exercise program. The changes in the morphological variables are shown in Table 1. Both groups showed decreases in their weight, body mass index, fat content, and waist girth (P < 0.05) after four weeks. Their weight and body fat decreased by 1.9 kg and 1.6 kg and by 1.5% and 1.4% for LDE and HDE, respectively. There were no changes in the waist-to-hip ratio for both groups. There were no group differences in these morphological variables after the program.
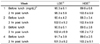
The energy value of lunch for both groups was slightly below 500 kcal, whereas the weight of the meal for LDE was two times greater than that for HDE (P < 0.05) (Table 2). There was no difference in the recorded total daily energy intake between the groups. The composition of nutrients they consumed during the program was similar for both groups (Table 3). Table 4 shows the estimated average fiber intake and the selected vitamin and mineral intake.
Table 5 shows the fasting blood lipid level both before and after the program. There were no differences in the measured parameters except for HDL-C, which decreased for both groups after the program (P < 0.05). There was no change in blood glucose levels before and after their lunch for both groups, and the levels were within the normal range (Table 6).
The sensation of hunger before dinner was relatively stronger for HDE than for LDE (P < 0.05), and this was clear except for Week 2 (Table 7).
In this randomized study, restricting daily energy intake and engaging in a regular exercise program led to decreases in the subjects' body weights and body fat, and the decreases were clear for both groups. Nonetheless, the perception of fullness was higher for LDE than for HDE before dinner, indicating that the subjects in the HDE group were more likely suffered from the sensation of hunger. Previous studies have suggested that a decrease in dietary energy intake is associated with weight loss [6,7,23] and that this is more pronounced with a diet reflecting low-energy density food [6,23,24]. Because previous research has shown that weight management is more effective if a diet program is combined with an exercise regimen [1,13], the present study investigates whether combining energy restriction by low-energy density food consumption with elevated energy expenditure by an exercise program is effective for weight management. The present study not only provides further evidence of the effect of dietary energy restriction on weight loss but also demonstrates the efficacy of a strategy combining a low-energy density diet with an exercise program for weight management.
The rough estimation of the daily energy balance indicates that both groups exhibited energy deficits. If an individual's resting metabolic rate (RMR) is assumed to be 1 kcal·kg body weight-1·hr-1 [26], the average energy deficit per day as a result of dietary restriction was approximately 193 kcal and -3 kcal for LDE and HDE, respectively. If bicycling at 60% of the maximum capacity represents 6 metabolic equivalent, then for this study, the metabolic cost during the exercise can be calculated as (6 kcal·kg body weight-1·hr-1 × individual body weight) × (40 min/60 min) [26]. Accordingly, the exercise energy expenditure were 266 kcal and 258 kcal and total energy deficit per day for the LDE and HDE groups were 459 kcal and 255 kcal, respectively. The magnitude of weight loss was determined for both groups based on differences in their energy balance, but those did not match. For example, the difference in weight loss was approximately 19% (1.9 kg vs. 1.6 kg), whereas that in the energy balance was approximately 80% (459 kcal vs. 255 kcal). The subjects' energy deficits per day (459 vs. 255 kcal) were calculated by weight; they were 2.17 kg for LDE and 1.20 kg for HDE (assuming a non-protein respiratory quotient of 8.0, 33.3% of carbohydrate, 66.7% of fat metabolism, the caloric equivalent of 4 kcal·g-1 for carbohydrate and 9 kcal·g-1 for fat, and a 30-day study period), showing higher and lower calculated values than those actually measured for LDE and HDE, respectively. The results have a practical implication: the difference in the negative energy balance between LDE and HDE can be magnified if the duration of study is prolonged. Also, the difference is more likely to be accentuated by differences in the sensation of hunger.
An important finding is the effectiveness of a low-density dietary strategy incorporating exercise in controlling the sensation of hunger. The subjects who had more food felt more full before dinner. Many studies have demonstrated that the energy density and amount of food were important environmental determinants of energy intake [20,27]. Further, it has been postulated that combining cognitive and orosensory factors with physiological responses related to gastric distention and emptying is a possible mechanism of fullness control [20]. However, such studies have only considered the efficacy of dietary volume or energy density and not considered the role of exercise in the control of hunger sensation. If both exercise and caloric restriction are recommended for controlling body weight, there is no reason for not considering both the modification of food density and the inclusion of exercise in weight management programs. Nevertheless, it remains unclear whether exercise alone could accentuate or blunt the sensation of fullness. The present study provides evidence that exercise programs involving changes in dietary food density can influence the sensation of hunger. The present results, together with the findings of previous research, suggest that combining the dietary intake of low-density food with an exercise program may be a feasible strategy for reducing both body weight and the sensation of hunger. Further, such a strategy is likely to induce individuals to continue participating in their weight management programs.
Many studies have demonstrated that weight loss after a decrease in dietary fat is associated with concomitant total energy intake reduction [28]. Strategies to reduce dietary energy density, such as varying the types of foods or diets either by fat content reduction or by consuming more quantity of fruits and vegetables, have been found to be effective for reducing energy intake [5,18,19,29]. Both restricting fat intake and reducing fat by increasing fruit and vegetable intake have been shown to result in marginal weight loss [18,24,28]. Ello-Martin et al. [18] suggested that water-rich foods can help reduce not only dietary energy density but also fat intake. A strategy combining dietary energy density with fat reduction has been found to be more effective in controlling hunger and reducing body weight than that involving only fat reduction. Increasing the intake of water-rich food foods such as fruits and vegetables has been shown to lead not only to effective weight management but also to a wide range of other health benefits [30,31]. In the present study, similar levels of dietary fat intake (in terms of dietary composition) led to similar amounts of weight loss for both groups. To the authors' knowledge, the present study is the first to demonstrate the weight loss patterns by combining changes in food density and exercise intensity.
Previous studies have suggested that self-reported dietary records may lead to underreporting and thus underestimated dietary intake results [32] and compliance bias [33]. However, because such findings are likely applicable to obese subjects, it is unlikely that the subjects in the present study reported less than what they consumed. In addition, because they were closely supervised within a relatively short period, it is likely that the results reflect no compliance bias. Previous studies have reported that subjects adhere better to study programs when they interact frequently with the program supervisor [34]. It is important to determine whether the prolonged adherence to both a low-energy density diet and an exercise program is possible. Previous studies have examined whether programs involving a low-energy density diet for weight loss can be maintained for more than two years [35], but no study has included exercise in such a program [18,36]. Thus, future research should examine the effectiveness of long-term programs that combine a low-energy density diet with exercise.
The present research study is limited by the length of the study. It is likely that that the subjects in the LDE group adhered better to the program because they consumed a greater amount of food and felt less hungry. Thus, it is likely that these subjects would have lost more weight if the study was conducted over a longer period [37]. In addition, from a practical point of view, future research should examine the effects of programs combining a low-energy density diet with exercise by using a wider range of subject groups.
Overall, the results suggest that a strategy combining a low-energy density diet with exercise for weight loss is more effective for slightly overweight young females. Both the LDE and HDE groups showed a similar pattern of weight loss, but those in the LDE group felt less hunger than those in the HDE group. Because both a low-energy density diet and exercise have been found to be effective for controlling and maintaining body weight, diet strategies that combine a low-energy density diet with a moderate-intensity exercise program may be effective for weight management. In addition, such a strategy may encourage individuals to participate in the weight management program longer because it can reduce the sensation of hunger.
Figures and Tables
References
1. Haskell WL, Lee IM, Pate RR, Powell KE, Blair SN, Franklin BA, Macera CA, Heath GW, Thompson PD, Bauman A. Physical activity and public health: updated recommendation for adults from the American College of Sports Medicine and the American Heart Association. Med Sci Sports Exerc. 2007. 39:1423–1434.
2. Ogden CL, Carroll MD, Curtin LR, McDowell MA, Tabak CJ, Flegal KM. Prevalence of overweight and obesity in the United States, 1999-2004. JAMA. 2006. 295:1549–1555.

3. American College of Sports Medicine Position Stand. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc. 2009. 41:459–471.
4. Makris AP, Foster GD. Dietary approaches to the treatment of obesity. Psychiatr Clin North Am. 2005. 28:117–139.

5. Bell EA, Rolls BJ. Energy density of foods affects energy intake across multiple levels of fat content in lean and obese women. Am J Clin Nutr. 2001. 73:1010–1018.

6. Duncan KH, Bacon JA, Weinsier RL. The effects of high and low energy density diets on satiety, energy intake, and eating time of obese and nonobese subjects. Am J Clin Nutr. 1983. 37:763–767.

7. Rolls BJ, Bell EA, Castellanos VH, Chow M, Pelkman CL, Thorwart ML. Energy density but not fat content of foods affected energy intake in lean and obese women. Am J Clin Nutr. 1999. 69:863–871.

8. Leser MS, Yanovski SZ, Yanovski JA. A low-fat intake and greater activity level are associated with lower weight regain 3 years after completing a very-low-calorie diet. J Am Diet Assoc. 2002. 102:1252–1256.

10. Elfhag K, Rossner S. Who succeeds in maintaining weight loss? A conceptual review of factors associated with weight loss maintenance and weight regain. Obes Rev. 2005. 6:67–85.

11. Pasman WJ, Saris WH, Westerterp-Plantenga MS. Predictors of weight maintenance. Obes Res. 1999. 7:43–50.

12. Schoeller DA, Shay K, Kushner RF. How much physical activity is needed to minimize weight gain in previously obese women? Am J Clin Nutr. 1997. 66:551–556.

13. Pate RR, Pratt M, Blair SN, Haskell WL, Macera CA, Bouchard C, Buchner D, Ettinger W, Heath GW, King AC, et al. Physical activity and public health. A recommendation from the Centers for Disease Control and Prevention and the American College of Sports Medicine. JAMA. 1995. 273:402–407.

14. Christ M, Iannello C, Iannello PG, Grimm W. Effects of a weight reduction program with and without aerobic exercise in the metabolic syndrome. Int J Cardiol. 2004. 97:115–122.

15. Evans EM, Saunders MJ, Spano MA, Arngrimsson SA, Lewis RD, Cureton KJ. Effects of diet and exercise on the density and composition of the fat-free mass in obese women. Med Sci Sports Exerc. 1999. 31:1778–1787.

16. Janssen I, Fortier A, Hudson R, Ross R. Effects of an energy-restrictive diet with or without exercise on abdominal fat, intermuscular fat, and metabolic risk factors in obese women. Diabetes Care. 2002. 25:431–438.

17. Curioni CC, Lourenco PM. Long-term weight loss after diet and exercise: a systematic review. Int J Obes (Lond). 2005. 29:1168–1174.

18. Ello-Martin JA, Roe LS, Ledikwe JH, Beach AM, Rolls BJ. Dietary energy density in the treatment of obesity: a year-long trial comparing 2 weight-loss diets. Am J Clin Nutr. 2007. 85:1465–1477.

19. Rolls BJ, Drewnowski A, Ledikwe JH. Changing the energy density of the diet as a strategy for weight management. J Am Diet Assoc. 2005. 105:S98–S103.

20. Kral TV, Rolls BJ. Energy density and portion size: their independent and combined effects on energy intake. Physiol Behav. 2004. 82:131–138.

21. Poppitt SD, Prentice AM. Energy density and its role in the control of food intake: evidence from metabolic and community studies. Appetite. 1996. 26:153–174.

23. Bell EA, Castellanos VH, Pelkman CL, Thorwart ML, Rolls BJ. Energy density of foods affects energy intake in normal-weight women. Am J Clin Nutr. 1998. 67:412–420.

24. Lanza E, Schatzkin A, Daston C, Corle D, Freedman L, Ballard-Barbash R, Caan B, Lance P, Marshall J, Iber F, Shike M, Weissfeld J, Slattery M, Paskett E, Mateski D, Albert P. Implementation of a 4-y, high-fiber, high-fruit-and-vegetable, low-fat dietary intervention: results of dietary changes in the Polyp Prevention Trial. Am J Clin Nutr. 2001. 74:387–401.

25. Friedewald WT, Levy RI, Fredrickson DS. Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin Chem. 1972. 18:499–502.

26. Ainsworth BE, Haskell WL, Leon AS, Jacobs DR Jr, Montoye HJ, Sallis JF, Paffenbarger RS Jr. Compendium of physical activities: classification of energy costs of human physical activities. Med Sci Sports Exerc. 1993. 25:71–80.

27. Du H, van der A DL, Ginder V, Jebb SA, Forouhi NG, Wareham NJ, Halkjaer J, Tjønneland A, Overvad K, Jakobsen MU, Buijsse B, Steffen A, Palli D, Masala G, Saris WH, Sørensen TI, Feskens EJ. Dietary energy density in relation to subsequent changes of weight and waist circumference in European men and women. PLoS One. 2009. 4:e5339.

28. Astrup A, Grunwald GK, Melanson EL, Saris WH, Hill JO. The role of low-fat diets in body weight control: a meta-analysis of ad libitum dietary intervention studies. Int J Obes Relat Metab Disord. 2000. 24:1545–1552.

29. Stubbs RJ, Johnstone AM, O'Reilly LM, Barton K, Reid C. The effect of covertly manipulating the energy density of mixed diets on ad libitum food intake in 'pseudo free-living' humans. Int J Obes Relat Metab Disord. 1998. 22:980–987.

30. Hung HC, Joshipura KJ, Jiang R, Hu FB, Hunter D, Smith-Warner SA, Colditz GA, Rosner B, Spiegelman D, Willett WC. Fruit and vegetable intake and risk of major chronic disease. J Natl Cancer Inst. 2004. 96:1577–1584.

31. Liu S, Manson JE, Lee IM, Cole SR, Hennekens CH, Willett WC, Buring JE. Fruit and vegetable intake and risk of cardiovascular disease: the Women's Health Study. Am J Clin Nutr. 2000. 72:922–928.

32. Trabulsi J, Schoeller DA. Evaluation of dietary assessment instruments against doubly labeled water, a biomarker of habitual energy intake. Am J Physiol Endocrinol Metab. 2001. 281:E891–E899.

33. Kristal AR, Andrilla CH, Koepsell TD, Diehr PH, Cheadle A. Dietary assessment instruments are susceptible to intervention-associated response set bias. J Am Diet Assoc. 1998. 98:40–43.

34. Maskarinec G, Robbins C, Riola B, Kane-Sample L, Franke AA, Murphy S. Three measures show high compliance in a soy intervention among premenopausal women. J Am Diet Assoc. 2003. 103:861–866.

35. Fitzwater SL, Weinsier RL, Wooldridge NH, Birch R, Liu C, Bartolucci AA. Evaluation of long-term weight changes after a multidisciplinary weight control program. J Am Diet Assoc. 1991. 91:421–429.





 PDF
PDF ePub
ePub Citation
Citation Print
Print







 XML Download
XML Download