Abstract
Premenstrual syndrome is a common chronic disorder in most women of reproductive age. The main symptoms are depression, anxiety, tension, feeling out of control, and mastalgia. In premenstrual syndrome, the effects of aromatic edible Elsholtzia splendens and Cirsium japonicum were investigated for over 3 months in 30 women participants in their twenties. In the Elsholtzia splendens capsule treated group, scores of depression and anxiety were significantly lower than those in the Cirsium japonicum capsule treated group. Moreover, instability of the premenstrual assessment form was significantly decreased in the Elsholtzia splendens capsule treated group. Our results suggest that Elsholtzia splendens could be an effective plant material in relieving symptoms of premenstrual syndrome.
Premenstrual syndrome (PMS) is a common chronic disorder that can affect women's interpersonal relationships, social behavior, work absenteeism, and work productivity [1]. Most women in the reproductive age have one or more emotional or physical symptoms in the premenstrual phase of the menstrual cycle. The symptoms are often mild, but 5-8% has severe symptoms that are associated with substantial distress and functional impairment. Mood and behavioral symptoms, including irritability, tension, depressed mood, tearfulness, and mood swings are the most distressing, but somatic complaints such as breast tenderness and bloating can also be problematic [2-4]. In medical reports, clinically significant premenstrual symptoms were named premenstrual syndrome (PMS) or premenstrual tension (PMT). The World Health Organization's International Classification of Disease (ICD) includes "Premenstrual Tension Syndrome" under the heading of "disease of the genitourinary tract".
For managing premenstrual syndrome, various treatments were suggested: cognitive behavioral therapy, lifestyle change, dietary supplement (Vitamin B6, calcium), herbal/complementary therapies, estradiol patches, and oral progestogens therapy [5-10]. Patients who seek medical help for PMS symptoms have usually implemented lifestyle changes and tried most over-the-counter remedies. However, before any medical treatments are commenced, it is still important to confirm that all appropriate lifestyle changes have been made. Recently, traditional herbal medicine was evaluated for relieving premenstrual syndrome [10].
Elsholtzia splendens is a Korean perennial, aromatic, and medicinal plant which belongs to the Labiatae family. Because Elsholtzia splendens contains volatile oil and flavonoids, the edible flower and leaves of this plant are primarily used for perfume and medicinal purposes [11]. Previous studies reported that Elsholtzia splendens had effects on reducing inflammation and fever [12].
Cirsium japonicum, a plant grown world-widely, is a perennial and medicinal plant which belongs to the Compositae family. The compounds most often reported for Cirsium japonicum are apigenin, cirsimaritin, kaempferol, linarin, luteolin, pectolinarin, and quercetin. Among them, linarin and pectolinarin are known to have anti-inflammatory properties [13]. Recently, the antidepressant effect of Cirsium japonicum was reported using an open field test and a forced swimming test [14]. Among the different plant parts of Cirsium japonicum, the leaves had the highest level of total flavonoids and apigenin content followed by the flowers and stems [15].
Considering the aforementioned effects (reducing pain and antidepressants effects) of Cirsium japonicum and Elsholtzia splendens, it seemed appropriate to evaluate their effects on relieving premenstrual syndrome. Hence, the objective of this study was to evaluate the effects of aromatic edible Elsholtzia splendens and Cirsium japonicum on premenstrual syndrome.
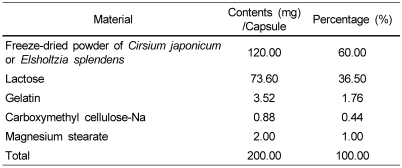
Samples of the aerial parts of Elsholtzia splendens and Cirsium japonicum were collected from Gyeonggi-do in the Republic of Korea. The plants were identified and authenticated by a botanist at the Korea National Arboretum. Samples were freeze-dried (FD5505, IlShin LabTech, Seoul, Korea) and the leafless woody stalks were discarded. The dried samples were subsequently crushed for 10 sec using a blender (HMC-400T; Hanil Electronics, Seoul, Korea), and then capsules were made as shown in Table 1. According to our previous experiment of total flavonoids and apigenin, the acceptable daily intake of both samples was 120 mg.
To recruit female participants for this study, in November 2006 we advertised to students at Duksung Women's University in Seoul, Korea, entitling the study, "PMS Management Program". All applicants were obliged to participate in an interview with this being the psychological assessment tool for screening. Thereafter, a total of 30 participants with PMS were selected from the interview and screening tests with the exception of those who 1) had missed menstruation cycles for more than 3 terms 2) had taken the contraceptive pill, or 3) were evaluated as unsuitable participants for this program because of serious mental illness as per SCL-90-R (Symptom Checklist-90-Revision).
Thirty participants were assigned to 3 groups, Elsholtzia splendens group (n = 10), Cirsium japonicum group (n = 10), and placebo group (n = 10) according to 1) age 2) Premenstrual Assessment Form (PAF) score 3) Beck Depression Inventory (BDI) score and 4) State-Trait Anxiety Inventory (STAI) score.
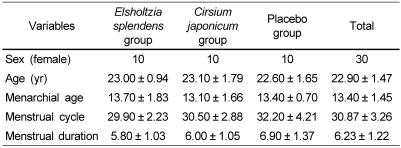
In addition, participants were asked to quit taking anesthetic alleviative or contraceptive pills during this program, and to record their daily PMS symptoms in a diary for monitoring and assessment purposes. The capsules for two weeks were put in a sanitary bag and provided to the participants. The participants had to present once every two weeks with their PMS 'Symptoms Diary' and discuss any changes in symptoms. In total, the participants were to take 1 capsule per day, every morning 30 minutes after waking up for 3 months. After an experimental period of 3 months, they were asked to submit their PMS 'Symptoms Diary' and to be re-tested using the same methodology conducted previously. The participants' mean age was 22.9 and the mean of the PAF score was 257.57 as shown in Table 2.
The BDI was utilized to assess depressive symptoms of the participants [16]. The BDI has 21 questions that measure the types and the severity of depression. The questions include emotional, cognitive, and motivational changes related to depression experienced in daily life. The higher score means the more serious depression. The Cronbach's α (reinstability coefficient) of the BDI in our study was 0.70.
To assess state anxiety, the STAI was assessed [4,17,18]. This inventory is useful for measuring state of anxiety of normal adults and distinguishing between clinically anxious people and the anxiety of psychiatric patients as well. Score ranges from 20 to 80, with the higher score indicating more serious anxiety. The Cronbach's α of the STAI in this study was 0.61.
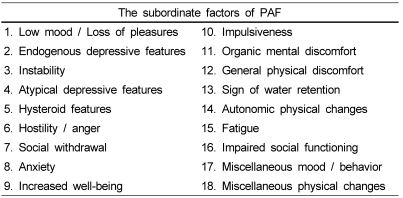
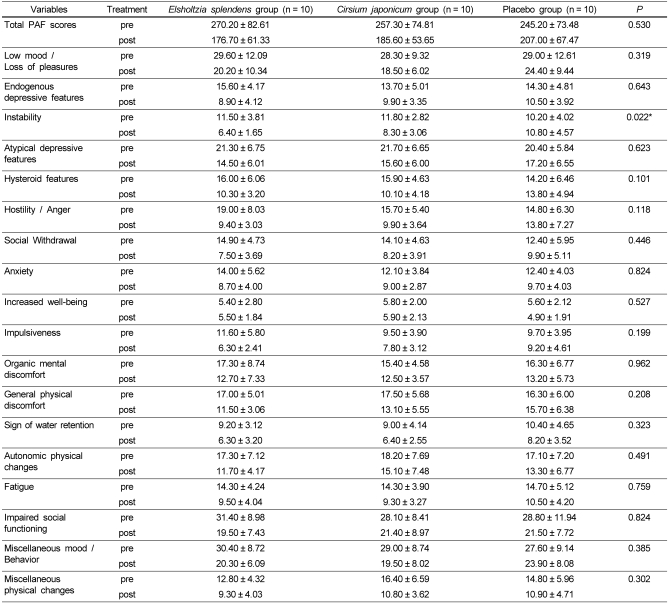
In this study, the PAF and Unipolar Summary Scales of the PAF-PCV were utilized to assess changes of emotional, behavioral and physical conditions for premenstrual duration [6,19]. The PAF is a measure for retrospectively evaluating the PMS symptoms of menstrual duration during the previous 3 cycles and the PAF-PCV is a retrospective measure for evaluating PMS symptoms of menstrual duration in the past 1 cycle after the treatment. This scale is a 95-item self-report measure and the total score ranges from 95 to 570 with the highest score indicating more serious symptoms. The PAF emphasized the variations of symptoms from 14~17 days before menstruation to the next period of menstruation. This scale in our study consisted of 18 subordinate symptoms (Table 3). The Cronbach's α was 0.94.
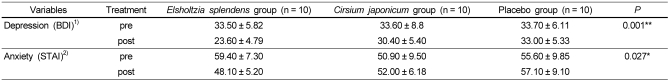
Effect of Elsholtzia splendens and Cirsium japonicum on premenstrual syndrome was studied via three experimental groups of thirty women with an average age of 22.9 years: 1) the Elsholtzia splendens group 2) the Cirsium japonicum group and 3) the placebo group. Participants of the experiment were, in mean menarchial age, 13.40 ± 1.45 years old. In addition, their menstrual cycle was 30.87 ± 3.26 days and the menstrual duration was 6.23 ± 1.22 days (Table 2). According to our previous experiment of total flavonoids and apigenin, the acceptable daily intake of Elsholtzia splendens and Cirsium japonicum sample was 120 mg. The Elsholtzia splendens group and the Cirsium japonicum group were instructed to take 1 capsule per day (which contained 120 mg of Elsholtzia splendens or Cirsium japonicum respectively), every morning 30 minutes after waking up. As for the placebo group, participants took capsules which were exactly the same, except for the absence of the plant material. This experiment was conducted for 3 consecutive months. Before a statistical demonstration, this study conducted the test about the equality of variances. As a result, the dispersion of the 3 groups was equal. In addition, ANOVA was analyzed to examine if there were significant differences of the pre-post scores on depression and anxiety among the 3 groups. The results showed that three groups significantly differed from the pre-post score of depression and anxiety. The pre-post scores of depression (BDI) were decreased from 33.50 to 23.60 in the Elsholtzia splendens group, from 33.60 to 30.40 in the Cirsium japonicum group, and from 33.70 to 33.00 in the placebo group. Finally, we discovered a greater decrease in the pre-post scores in the Elsholtzia splendens group than in other groups (P < 0.01). The pre-post scores of anxiety were decreased from 59.40 to 48.10 in the Elsholtzia splendens group, but there were increases from 50.90 to 52.00 in the Cirsium japonicum group and from 55.60 to 57.10 in the placebo group. Finally, there were greater decreases of anxiety scores in the Elsholtzia splendens group than in other two groups (P < 0.05). Moreover, the result of the Scheffe test showed that the post scores of depression and anxiety in the Elsholtzia splendens group were decreased more than in other groups (Table 4).
The significant differences between the three groups on the pre-post scores of the PAF were presented in Table 5. Although statistically significant differences of the total PAF scores were not found, the total scores of the PAF were decreased from 270.20 to 176.70 in the Elsholtzia splendens group, from 257.30 to 185.60 in the Cirsium japonicum group, and from 245.20 to 207.00 in the placebo group. As a result, the total scores of the PAF in the Elsholtzia splendens group were not statistically significant, but presented greater decreases compare to other groups. However, the instability in subordinate factors showed a significant difference (P < 0.05). The pre-post scores of the instability were decreased from 11.50 to 6.40 in the Elsholtzia splendens group and from 11.80 to 8.30 in the Cirsium japonicum group, but there was an increase from 10.20 to 10.80 in the placebo group. Last but not least, the instability scores in the subordinate scales of the PAF in the Elsholtzia splendens group showed statistically more significant differences than other groups. In addition, although significant differences were not shown statistically in all scales (except for the instability), it was found out that there were changes of the mean score between the pre-post in all scales. In particular, the Elsholtzia splendens group revealed greater changes between the pre-post scores than other two groups.
Premenstrual syndrome is the consequence of fluctuations in the ovarian sex steroids leading to physical and behavioral symptoms. Many symptoms of premenstrual syndrome have been described: irritability, aggregation, depression, tension, anxiety, feeling out of control, bloatedness, and mastalgia are well-known symptoms [2-4,19]. In this study, depression and anxiety of the Elsholtzia splendens group were significantly decreased at the P < 0.01 and P < 0.05 respectively. As shown in Table 5, instability demonstrated significant decreases in the Elsholtzia splendens group after the intake of the capsules (P < 0.05). Although there were no statistical significances, the total PAF scores indicated a decrease in the Elsholtzia splendens group after the intake. Our results revealed that Elsholtzia splendens is effective for decreasing depression, anxiety, and instability which are common symptoms of premenstrual syndrome. Therefore, Elsholtzia splendens is thought to be a useful plant material for relieving premenstrual syndrome.
Recent investigation into the relief of premenstrual syndrome has employed hormone and antidepressant drugs, whereas treatment using plant materials was not studied extensively. One randomized placebo controlled study has shown that Agnus castus is an effective treatment for women with premenstrual syndrome. The effects were confirmed by the women's selfassessment and the investigator's evaluation [7]. The extensive treatment for St. John's wort as an antidepressant in women with severe premenstrual syndrome resulted in a significant relief of symptoms [7]. It was reported that evening primrose oil is of little value in treating premenstrual syndrome, except for the management of cyclical premenstrual mastalgia for which it is effective [2]. By utilizing Kampo which is Japan's traditional herbal medicine used to treat premenstrual syndrome, women who participated in the experiment reported improvements in their condition. In these studies, however, it was not revealed which compound of the herbal medicine was dedicated to the relief of premenstrual syndrome symptoms. As for the effect of carbohydrates on premenstrual syndrome symptoms, relatively, there are detailed explanations. In a study about whether mild to moderate premenstrual syndrome could be improved with a commercial, carbohydrate-rich beverage, the profile of mood states (tension & anxiety factors) showed a significant effect (P < 0.05). The carbohydrate beverage probably acts by increasing the availability of tryptophan. This, in turn, may increase serotonin synthesis which reduces the mood and appetite disturbances accompanying PMS [6].
As mentioned above, our results strongly suggest that Elsholtzia splendens is effective for decreasing depression, anxiety, and instability which are common symptoms of premenstrual syndrome. According to our previous experiments, the amount of total flavonoid of flower and leaf of Elsholtzia splendens was 2.52 mg/g and 1.99 mg/g, respectively. And the content of apigenin of flower and leaf was 18 ug/ml and 1.35 ug/ml, respectively [20]. In Cirsium japonicum, the amount of total flavonoid of flower and leaf was 1.54 mg/g and 2.58 mg/g, respectively. In addition, the content of apigenin of flower and leaf was 0.33 ug/ml and 2.73 ug/ml, respectively [15]. From the above data, the amount of total flavonoids for Elsholtzia splendens and Cirsium japonicum is similar, but the content of apigenin of Elsholtzia splendens is comparatively higher than those of Cirsium japonicum. We expect that, based on our previous research, biologically active compounds which had these effects are presumed to be flavonoid and apigenin from Elsholtzia splendens. Therefore, further study should clarify if flavonoid and apigenin extracted from Elsholtzia splendens decrease depression, anxiety, and instability. In addition, further experiments should be done to reveal its action mechanisms.
In conclusion, effects of Elsholtzia splendens and Cirsium japonicum on premenstrual syndrome were studied through three experimental groups: 1) the Elsholtzia splendens group 2) the Cirsium japonicum group and 3) the placebo group. Elsholtzia splendens is significantly effective for decreasing depression, anxiety, and instability which are common symptoms of premenstrual syndrome. Therefore, Elsholtzia splendens may be a useful plant material for relieving premenstrual syndrome.
Notes
This study was funded by Agriculture R&D Promotion Center, Ministry of Agriculture and Forestry, Republic of Korea (204024-03-3-SB010) and Priority Research Centers Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology (2009-0094018).
References
1. Ekholm UB, Bäckström T. Influence of premenstrual syndrome on family, social life, and work performance. Int J Health Serv. 1994; 24:629–647. PMID: 7896466.

2. Yonkers KA, O'Brien S, Eriksson E. Premenstrual syndrome. Lancet. 2008; 371:1200–1210. PMID: 18395582.

3. Indusekhar R, Usman SB, O'Brien S. Psychological aspects of premenstrual syndrome. Best Pract Res Clin Obstet Gynaecol. 2007; 21:207–220. PMID: 17175199.

5. Winther K, Hedman C. Assessment of the effects of the herbal remedy female on the symptoms of premenstrual syndrome: a randomized, double-blind, placebo-controlled Study. Current Therapeutic Research. 2002; 63:344–353.
6. Freeman EW, Stout AL, Endicot J, Spiers P. Treatment of premenstrual syndrome with a carbohydrate-rich beverage. Int J Gynaecol Obstet. 2002; 77:253–254. PMID: 12065140.

8. De Souza MC, Walker AF, Robinson PA, Bolland K. A synergistic effect of a daily supplement for 1 month of 200mg magnesium plus 50mg vitamin B6 for the relief of anxiety-related premenstrual symptoms: A randomized, double-blind, crossover study. J Womens Health Gend Based Med. 2000; 9:131–139. PMID: 10746516.
9. Chou PB, Morse CA. Understanding premenstrual syndrome from a Chinese medicine perspective. J Altern Complement Med. 2005; 11:355–361. PMID: 15865504.

10. Gepshtein Y, Plotnikoff GA, Watanabe K. Kampo in women's health: Japan's traditional approach to premenstrual symptoms. J Altern Complement Med. 2008; 14:427–435. PMID: 18466067.
11. Lee CB. Illustrated flora of Korea. 1999. Seoul: Hyangmunsa;p. 660–767.
12. Youn JS. Comparison study on the beneficial effect of Elsholtzia splendens and Elsholtzia ciliata. Journal of Herbology. 1992; 7:33–45.
13. Jordon-Thaden IE, Louda SM. Chemistry of Cirsium and Carduus: a role in ecological risk assessment for biological control of weeds? Biochem Syst Ecol. 2003; 31:1353–1396.
14. Park HK, Yoon SY, Choi JH, Ko HS, Suh YW, Lee YS, Kim GH, Chung MS, Cheong JH. The antidepressant effects of in Cirsium japonicum ICR mice. Yakhak Hoeji. 2006; 50:429–435.
15. Chung MS, Um HJ, Kim CK, Kim GH. Development of functional tea product using Cirsium japonicum. Journal of the Korean Society of Food Culture. 2007; 22:261–265.
16. Beck AT, Ward CH, Mendelson M, Mock J, Erbaugh J. An inventory for measuring depression. Arch Gen Psychiatry. 1961; 4:561–571. PMID: 13688369.

17. Spielberger CD, Gorsuch RL, Lushene RE. STAI Manual for the State-Trait Anxiety Inventory. 1970. Palo Alto, CA: Consulting Psychologists Press;p. 123.
18. Hahn DW, Lee CH, Chon KK. Korean adaptation of Spielberger's STAI (K-STAI). The Korean Journal of Health Psychology. 1996; 1:1–14.
19. Halbreich U, Endicott J. Relationship of dysphoric premenstrual change to depressive disorder. Acta Psychiatr Scand. 1985; 7:331–338. PMID: 4039877.
20. Kim GH. Report on development of food materials for premenstrual syndrome and antidepressant effect using Cirsium and Elsholtzia plants containing flavonoids. 2007. Seoul: ARPC;p. 9–17.




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download