Abstract
Breastfeeding is an unequalled way of providing ideal food for the infants. The benefits of breastfeeding practices to infants and mothers are well documented. However, information on breastfeeding practices and its effect on body mass index (BMI) of mothers are scarce, particularly in Ekiti State of Nigeria. Therefore, the present study is designed to assess breastfeeding practices and its association with BMI of mothers. A descriptive and cross-sectional study was conducted among breastfeeding mothers that attended postnatal clinic of the state specialist hospitals and maternity centers in the study location. The specialist hospital and two-third of the nine maternity centers were purposively selected because of their health facilities and personnel. The mother-child pairs (200 respondents) were randomly selected from the study locations. Information on demographic characteristic, socio-economic parameters, nutritional knowledge of breastfeeding and dietary intakes of mothers were collected using questionnaires. BMI of mothers was determined as described by World Health Organization. Age distribution of mothers was between 25-34 years; and almost half of respondents had good educational background and were engaged in different occupations. The respondent monthly income ranged between = N = 3500 - 26000 ($26.92 - $200); and their dietary intakes varied between starchy and protein-based food. The result also showed that the respondent consumed enough nutrients to meet up the recommended daily allowance for protein, carbohydrate, fat, zinc, magnesium, sodium and phosphorous requirements. The BMI classifications showed that over three-fifth of respondents were normal, while the remaining were underweight (6%) and overweight/obese (26.5%). Also, large proportion of respondents engaged in exclusive breastfeeding and with good knowledge of breastfeeding practices. Statistically, exclusive breastfeeding practices had no correlation between the BMI and frequency of breastfeeding. The study, therefore, concluded that mothers had good knowledge of breastfeeding practice; and that there was no association between breastfeeding practices and BMI.
Nutrition encompasses processes leading to and involved with the utilization of nutrients for growth, development, maintenance and activity. Therefore, good nutrition is the cornerstone for survival, health and development of current and succeeding generations. Well-nourished women face fewer risks during pregnancy and childbirth, and their children set off on firmer developmental paths, both physically and mentally. Recently, findings have showed that malnutrition is increasing in developing countries; and that women in the reproductive age group are the most vulnerable to malnutrition [1-3], due to poor feeding practices, low dietary intakes, inequitable distribution of food within the household and dietary taboos. The high prevalence of malnutrition in these countries is attributed to the present economic crisis and the adjustments being undertaken by many of these developing countries, Nigeria inclusive [4,5]. In developing countries, several studies have reported that the real income of a household is indeed an important determinant of its access to food which, in turn, is a major determinant of child and maternal nutritional wellbeing [6,7]. Epidemiological studies have reported on the relationship between diet and poverty; and the report established that the purchasing power of a family dictates the level of household food security and types of diets that are ultimately consumed by household members [8,9].
Infant and young children feeding are the cornerstone of care for childhood growth and cognitive development. The period of infancy is the most important stage in the developmental process of human life. During this period, growth is very rapid and demands of the body for nutrients are comparatively higher than any other period of life. The growing child therefore needs all the essential nutrients for growth and cognitive development. Recently, studies have shown that one of the means of making these essential nutrients available for the growing child during the first six months of life is through exclusive breastfeeding practices [10-12]. Exclusive breastfeeding is when an infant receives no other food or drink, or even water, besides breast milk (whether expressed or through breastfeeding) for the first six months of life [12]. The quantity of nutrients present in the volume of milk produced by healthy lactating mothers has been found to be adequate in meeting the baby's nutrient and energy requirement up to the age of six months [12,13].
Breastfeeding is an unequalled way of providing ideal food for the health growth and cognitive development of infants [14-16]; and it offers many advantages for children that cannot be duplicated by any other form of feeding. The benefits of breastfeeding begin from the first moments after childbirth and last for many years after breastfeeding ends. Extensive researches, especially in recent years, have reported on various advantages of breastfeeding practices to infants, mothers, families, and society [17-22]. These include health, nutritional, immunologic, developmental, psychological, social, economic, and environmental benefits. Studies have shown that breastfeeding provides ideal nutrition despite any social or economic disadvantages that may exist for the child; and that breastfed children are healthier, have fewer symptoms and shorter illnesses when they do get sick and well developed brain compared with formula-fed children [23-30]. For the mothers, it is evident that breastfeeding hasten recovery from pregnancy and childbirth episode; and it also provides lifelong health advantages, such as prevention of breast cancer, returning to pre-pregnancy weight [20,31].
The objectives of the study were to assess the breastfeeding knowledge, practices and influence of breastfeeding practices on the nutritional status of nursing mothers from low-income families.
The study was conducted in Ekiti State of Nigeria. The state is one of the states in South Western Nigeria and the people in the state are predominantly Yoruba ethnic group. The main occupations of the people in the state are farming, in which more than 80% are involved. While the remaining people involved in different occupations like agro-allied business, petty trading, civil servant or vocational job (barbing, carpentry, vulcanize and automobile mechanics).
A cross-sectional study was conducted among nursing mother-child pair that attended postnatal clinic of the state specialist hospitals and maternity centers. Two of the six specialist hospital and three of the nine maternity centers were purposively selected because of their health facilities and health personnel. The sample size was calculated as described by Gahlinger and Abramson [32]. The estimated sample size was 200 mother-child pairs; and the subjects were randomly selected among the nursing mother-child pairs that attended postnatal clinic sections of the hospitals and maternity centers on every Monday and Thursday respectively.
The mother-child pairs, whose child age was within 0 - 12 months, were selected for the study. This age range was considered base on the information gathered during the preminary survey of the study that most of the mothers stopped child breastfeeding at aged 12 months.
Data were collected by trained health researchers using structured questionnaires designed in English and Yoruba languages for easier communication. The questionnaire was designed to collect information on the following:
This involved collection of personal data of the subject (mother and child), such as age, sex and religion.
The socio-economic status of the subjects was determined by considering items such as highest educational attainment (primary school, secondary school, tertiary institution, higher degree and no formal educational background), occupation (pensioners, farming, civil servants, vocational jobs, petty trading and no job) and daily/weekly/monthly income, was categorized into ≤ 7,500, 7,500 - 15,000, 15,000 - 25,000, 25,000 - 30,000 and ≥ 30,000 Naira.
Information on eating frequency before and during breastfeeding practices and the type of food consumed were obtained through questionnaire. This was further buttressed by a 24-hours dietary recall method. The quantity of food intakes by nursing mothers were estimated using household measurements. This method had been validated by several investigators [33-35]. The recipe of food intakes by the subjects were collected, prepared and 100 g of the food samples were analyzed for moisture, fat, protein (N × 6.25), crude fiber, ash and carbohydrate (estimated by difference) using AOAC [36] methods. The gross energy of the dried food sample was determined against thermocouple grade benzoic acid using a Gallenkamp ballistic bomb calorimeter (London, UK; model CBB -330-0104L). The sodium and potassium contents were determined by flame photometry. Other minerals (calcium, magnesium and zinc) were determined after wet digestion with a mixture of nitric, sulphuric and hydrochloric acid using Atomic Absorption Spectrophotometer (AAS Model SP9). The energy and nutrient intakes of the subjects were estimated using the results obtained from proximate and mineral analyses and the quantity measured through 24-hour dietary recall method.
The questionnaire consisted series of questions as related to the nutritional and health benefits of breastfeeding, such as, Do you breastfeed your child? Do you practices exclusive breastfeeding? How often do you breastfeed your child? What is your perception towards breastfeeding practices? Is breastfeeding only be enough for a child of aged 0-6 months? At what age do you think breast milk alone would no longer be enough to feed infant? Is breast milk nutritional composition better than infant formula? Do you aware that a breastfed child has immunity against diseases over non breastfed child? From your previous experience did your child prefer breast milk to infant formula on introduction?, and Based on your previous experience what did you do when your child preferred breast milk to weaning food? Each of the questions was allocated grade and the cumulative score of the respondents were used to determine their nutritional knowledge as related to breastfeeding benefits. This method had been validated by an investigator [37].
Anthropometric measurements (heights and weights) of the mothers were measured using the standard techniques described by World Health Organization [38]. Training for standardization of the measurements, followed by field practice and testing was performed prior to data collection. All measurement was carried out in the morning between 9 am and 12 noon. The nursing mother, wearing light clothing, was weighed to the nearest 0.1 kg with a Seca digital scale (Germany). Height was measure to the nearest 0.1 cm with a portable stadiometer. The body mass index (BMI = weight / height (m)2) (kg/m2) was calculated. The BMI reference of WHO (2004) was used to classify the mothers as underweight, normal, overweight and obese.
The study protocol was approved by the ethics committee of Federal University of Technology, Akure, Ondo Stae, Nigeria. The subjects were briefed on the details of the study. They were informed that their participation in the study was voluntary, the study would not cause them or their child any harm, and there was no penalty for those who declined.
Data were analysed using SPSS for windows (Version 11.0 SPSS, Chicago, Illinois, USA). Discrete variables were expressed as mean (X) and standard error of mean (SEM). The demographic characteristics and BMI were expressed as the percentage of the population. Correlation analysis was calculated to determine the relationship between breastfeeding frequency of infant, eating frequency and BMI.
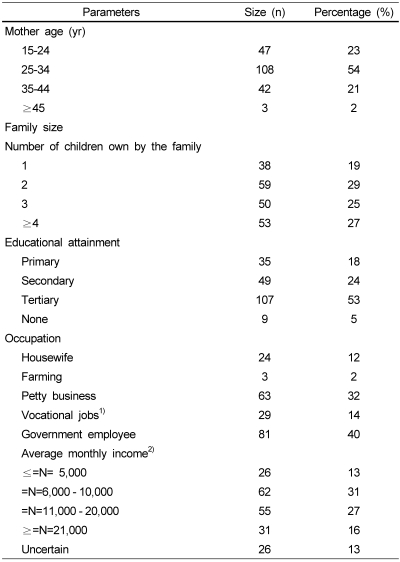
The demographic and socio-economic characteristics of the nursing mothers are presented in Table 1. The age distribution of the nursing mothers showed that 23.5% belonged to the age range of 15-24 years, 54% were within 25-34 years of age, 21% fell within 34-44 years of age and 1.5% was 45 years and above. The family size of the subjects showed that 19.0% had one child, 29.5% two children, 25.0% three children and 26.5% four children and above. The educational attainment of the subjects showed that 17.55 had primary school education, 24.5% secondary education, 53.5% tertiary education ranging from national certificate of education, ordinary diploma, higher national diploma and university graduates. 4.5% of the subjects did not have formal education. The occupation of the subjects were as follows: housewife (12%), farming (1.5%) and petty traders (31.5%); while the remaining subjects engaged in vocational jobs, like hair dressers, tailoring, etc., and 40.5% of the subjects were government employees, that is, civil servants. The average monthly income distributions of the subjects were as follows: 13% earned less five thousand Naira ($ 38.49 USD), 31% earned between 6,000 and 10,000 Naira ($ 46.15 - 76.92); while 43% earned 11,000 Naira ($ 84.62) and above.
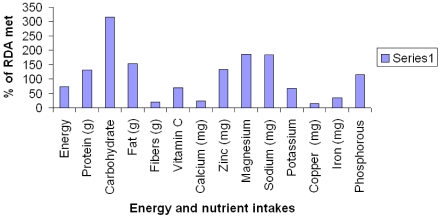
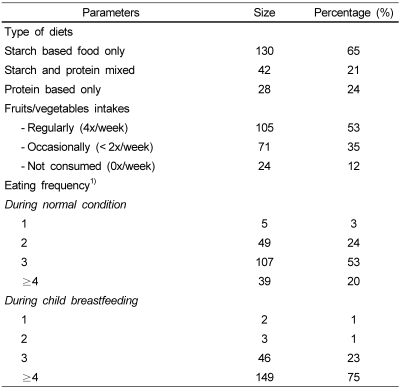
Table 2 shows the dietary intake and frequency of eaten by the nursing mothers. The result showed that larger proportion of mothers (65%) ate starch based diets, 21% ate mixed diets (starch and protein-based foods) and 24% ate protein based food like moimoi, akara, and cooked beans within the last 24 hours of the study. Also, 52.5% of the nursing mothers agreed that they consumed fruits and vegetables regularly, 35.5% occasionally and 12% did not. The eaten frequencies of the nursing mothers before breastfeeding practices showed that large proportion of the subjects (80.5%) ate three times or less per day, while large proportion of the mothers (74.5%) ate more than three times during the breastfeeding period. The estimated energy and nutrient intakes and percentage of recommended daily allowances (RDA) met by the mothers is presented in Fig. 1. The result showed that nursing mothers consumed adequate foods to meet up with the essential nutrients requirements like protein, carbohydrate, fat, zinc, magnesium, sodium and phosphorous requirements, while for the energy, fiber and micronutrients like vitamin C, calcium, potassium, copper and iron were low.
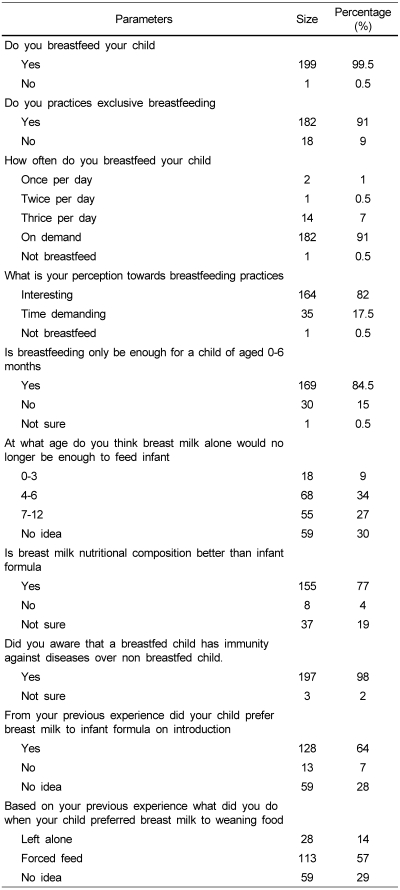
The response of nursing mothers to breastfeeding practices and health knowledge is presented in Table 3. The result showed that 91% of the mothers practiced exclusive breastfeeding for five months at least and 9% did not; and the breastfeeding patterns showed that 91% breastfed their babies on demand; while the remaining mothers rationed their babies with exception of a mother who did not breastfed at all due to her illness. Large proportion of the mothers (82%) had good perception towards breastfeeding practices and 17.5% agreed that breastfeeding practices are time demanding and very strenuous. The nutritional knowledge of the mothers towards breastfeeding showed that 84.5% agreed that breast milk alone is enough for infant at aged 0-6months, while 15% did not agreed. Also, 9% agreed that breast milk alone would not be enough for a babe of aged 0-3 months, 34% agreed on aged 4-6 months and 27.5% aged 7-12 months; while 29.5% were not sure of a particular age when breast milk alone would no longer be enough for the babe. For the nutritional composition of breast milk compared to commercial formula; 77.5% of the nursing mothers agreed that breast milk was better than commercial formula. Similarly, 98.5% agreed that human breast milk contains some substances that boost the immunity of infant, while the remaining subjects (1.5%) did not sure of this. Amongst the mothers that had weaned a child before or had started to wean their child, 64% agreed that their babe preferred breast milk to commercial formula upon introduction, 6.5% responded that their babies did not discriminate between breast milk and commercial formula. Also, upon rejection of introduced commercial formula 56.5% of the mothers forced feed their babies, while 14% did not take any further action to force feed.
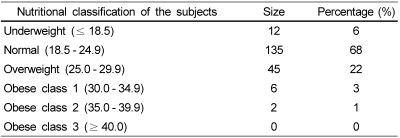
The nutritional status of the nursing mothers is showed in Table 4. The results showed that 6% of nursing mothers were underweight, 67.5% were normal (well nourished) and 22.5% were overweight; while remaining subjects (4%) were obese. For the children 91.4% were normal (i.e., well nourished) and 8.6% mildly malnourished.
Statistically there were no relationship between breastfeeding frequency and body mass index (BMI) (r = 0.03057) and eaten frequency of the nursing mothers (r = 0.094903 (P = 0.5).
It was observed in this study that large proportion of the mothers fell within the age group of 25-34 years; this showed that the average reproductive age of Nigerian women was within this aged group. This observation had been similarly reported by Awoyinka et al. [39]. In this present study, it was observed that large proportion of mothers consumed varieties of foods like tuber, cereal, legumes, fruits and vegetables. However, it could also be deduced from the study that the main dietary intakes of the study population is starch-based with limited consumption of fruits and vegetables. The poor dietary intakes observed in this study could be attributed to the present economic crisis and the adjustments being undertaken in Nigeria [4,5,40]. In developing countries, several studies have reported that the real income of a household is indeed an important determinant of its access to food which, in turn, is a major determinant of child and maternal nutritional wellbeing [40] (Cornia, 1994); and that purchasing power of a family dictates the level of household food security and types of diets that are ultimately consumed by household members [8,9].
The breastfeeding practices of mothers influenced their eating frequencies. The eaten frequency during breastfeeding practices was significantly higher (P < 0.0001) when compared to eaten frequency before breastfeeding practices commenced. The increased in dietary intakes of mothers during breastfeeding could be attributed to the high demand of nutrients for the production of breast milk and other metabolic activities of the lactating mother. The body mass index (an index of present nutritional status) of respondents showed that large proportions of the subjects were either normal or obese. This may be attributed to eaten frequency of the subjects or as a result of weight gained during pregnancy periods.
The response of nursing mothers to the practices, nutritional and health knowledge of breastfeeding was quite encouraged. This observation could be attributed to the nutrition education concerning benefits of breastfeeding practices given to the mothers during their antenatal and postnatal clinic or it could also be attributed to the nature of the mothers' occupation, that is, housewife, farming, petty trading and vocational jobs, which give more rooms for closeness of the mother and child. Al-Shoshan [41] reported that family income and mothers' occupation and level of education were significantly associated with infant feeding practices, particularly breastfeeding. Mothers from better economic status had higher chance of not practice exclusive breastfeeding for the first 6 months of life compared to mothers from a poor family [42]. Similarly, working outside the home, particularly government employee, had higher chance of not breastfeeding exclusively or early weaning of their child before six months of age compared to housewives [42].
The nutritional knowledge of mothers towards breastfeeding practices was quite encouraged, because high proportions of the mothers agreed that breast milk alone was enough to meet nutritional requirements of infants before aged six months; and that human breast milk is better than any of the commercial weaning formula in terms of nutritional composition and health benefits. Similarly, Al-Shoshan [41] also reported that large proportion of Saudi women practiced exclusive breastfeeding and also had better knowledge of nutritional and health benefits that associated with infant breastfeeding practices. Scientifically, it has been proven that breast milk is a complete food, and that breast milk alone is sufficient to nourish a child for at least the first six months of life [14-16,43,44]. Also, quite a numbers of study have reported on various advantages of breastfeeding practices, like health, economic, environmental etc, to infants, mothers, families, and society [18-22,45].
The body mass index of mother showed that large proportion of the respondents was normal. This could be deduced that exclusive breastfeeding practice has beneficial effect on the nutritional well-being; hence, it does not have any negative effect to the nutritional and health status of the nursing mothers apart from increasing their appetite and eating frequency. It has been proven that breastfeeding practices hasten recovery from pregnancy and childbirth episode; and it also provides lifelong health advantages, such as prevention of breast cancer, returning to pre-pregnancy weight [19,20,31]. Similarly, investigations showed that breastfeeding provides ideal nutrition to infants despite any social or economic disadvantages that may exist for the child; and that breastfed children are healthier, have fewer symptoms and shorter illnesses when they do get sick and well developed brain compared with formula-fed children [23-25,27-30].
The relationships between frequency of breastfeeding practices and nutritional status of mothers were established in this study. It was observed that there were weak negative relationships between the frequency of breastfeeding and BMI (r = 0.0306, P < 0.05) of the mothers. This further indicates that exclusive breastfeeding practices do not affect the health and nutritional wellbeing of nursing mothers [46].
In conclusion, the study showed that large proportion of mothers practiced exclusive breastfeeding with good knowledge of breastfeeding benefits to infants; and breastfeeding practices did not influence body mass index of nursing mothers. Hence, nursing mothers should endeavor to practice exclusive breastfeeding.
References
1. ACC/SCN. Administration Committee on Coordination-Sub-Committee on Nutrition (ACC/SCN). Fourth report on the world nutrition situation. 2000. Geneva:
2. Yimer G. Malnutrition among children in southern Ethiopia: Levels and risk factors. Ethiopian Journal of Health Development. 2000; 14:283–292.

3. Zewditu G, Kelbessa U, Timotewos G, Ayele N. Review the status of malnutrition and trend in Ethiopia. Ethiopian Journal of Health Development. 2001; 15:55–74.
4. Ijarotimi OS, Oyeneyin OO. Effect of economic restructuring on household food security and nutritional status of Nigerian children. Journal of Food, Agriculture and Environment. 2005; 3:27–32.
5. Osmani SR. Poverty and nutrition in South Asia. Abraham Horwitz lecture delivered at the Symposium on Nutrition and Poverty held on the occasion of UN ACC/SCN 24th Session, Kathmandu. 1997. Nepal: p. 17–21.
6. Lisa CS, Lawrence H. Explaining child malnutrition in developing countries: A cross-country analysis. Research Report. 2000; 111:4.
7. Müller O, Krawinkel M. Malnutrition and health in developing countries. CMAJ. 2005; 173:279–286. PMID: 16076825.
8. Kinra S, Nelder RP, Lewendon GJ. 'Deprivation and childhood obesity: a cross sectional study of 20 973 children in Plymouth, United Kingdom'. J Epidemiol Community Health. 2000; 54:456–460. PMID: 10818122.

9. Coakley A. Healthy eating: food and diet in low income households. Administration. 2001; 49:87–103.
10. Read M, Catteneo A. The optimal duration of exclusive breast feeding. IBFAN Breastfeeding Briefs. 2001; 31-32:1–10.
11. Kramer M, Kakuma R. Optimal duration of exclusive breastfeeding. Cochrane Database Syst Rev. 2002; CD003517. PMID 11869667. PMID: 11869667.

12. WHO. Child and Adolescent Health and Development. Exclusive Breastfeeding. 2006.
14. American Academy of Pediatrics . Breastfeeding and the use of human milk. Pediatrics. 1997; 100:1035–1039. PMID: 9411381.
15. Institute of Medicine. Nutrition during lactation. 1991. Washington, DC: National Academy Press.
16. The optimal duration of exclusive breastfeeding: results of a WHO Systematic Review. WHO [Internet]. cited 2002 January 11. Available from: http://www.who.int/inf-pr-2001/en/note2001-07.html.
17. Atkinson S, Lönnerdal BO. Proteins and non-protein nitrogens in human milk. 1989. CRC Press.
18. Weaver L, Arthur H, Bunn J, Thomas J. Human milk IgA concentrations during the first year of lactation. Arch Dis Child. 1998; 78:235–239. PMID: 9613353.

19. Heinig MJ, Dewey KG. Health advantages of breastfeeding for mothers: a critical review. Nutr Res Rev. 1997; 10:35–56. PMID: 19094257.
20. Labbok MH. Effects of breastfeeding on the mother. Pediatr Clin North Am. 2001; 48:143–158. PMID: 11236722.

21. Ball TM, Wright AL. Health care costs of formula feeding in the first year of life. Pediatrics. 1999; 103:870–876. PMID: 10103324.
22. Gartner LM, Morton J, Lawrence RA, Naylor AJ, O'Hare D, Schanler RJ, Eidelman AI. Breastfeeding and the use of human milk. Pediatrics. 2005; 115:496–506. PMID: 15687461.
23. Anderson JW, Johnstone BM, Remley DT. Breastfeeding and cognitive development: a meta-analysis. Am J Clin Nutr. 1999; 70:525–535. PMID: 10500022.

24. Drane DL, Logemann JA. A critical evaluation of the evidence on the association between type of infant feeding and cognitive development. Paediatr Epidemiol. 2000; 14:349–356.

25. Lykke Mortensen E, Fleischer Michaelsen K, Sanders SA, Reinisch JM. The association between duration of breastfeeding and adult intelligence. JAMA. 2002; 287:2365–2371. PMID: 11988057.

26. Heinig MJ, Dewey KG. Health advantages of breastfeeding for infants: a critical review. Nutr Res Rev. 1996; 9:89–110. PMID: 19094266.
27. Heinig MJ. Host defense benefits of breastfeeding for the infant: effect of breastfeeding duration and exclusivity. Pediatr Clin North Am. 2001; 48:105–123. PMID: 11236719.
28. Gdalevich M, Mimouni D, David M, Mimouni M. Breast-feeding and the onset of atopic dermatitis in childhood: a systematic review and meta-analysis of prospective studies. J Am Acad Dermatol. 2001; 45:520–527. PMID: 11568741.

29. Gdalevich M, Mimouni D, Mimouni M. Breast-feeding and the risk of bronchial asthma in childhood: a systematic review with meta-analysis of prospective studies. J Pediatr. 2001; 139:261–266. PMID: 11487754.

30. Uhari M, Matysaari K, Niemela M. A meta-analytic review of the risk factors for acute otitis media. Clin Infect Dis. 1996; 22:1079–1083. PMID: 8783714.
31. Lawrence RA, Lawrence RM. Breastfeeding: a guide for the medical profession. 1999. 5th edition. St. Louis: Mosby.
32. Gahlinger PM, Abramson JH. Computer programs for epidemiologic analysis (CPEA). 1993. Honolulu, Hawaii: Makapuu Medical Press.
33. Farvid MS, Jalali M, Siassi F, Navid S, Hosseini M. The impact of vitamins and/or mineral supplementation on blood pressure in type 2 diabetes. J Am Coll Nutr. 2004; 23:272–279. PMID: 15190052.

34. Biró G, Hulshof KFAM, Ovesen L. Amorim Cruz JA for the EFCOSUM Group. Selection of methodology to assess food intake. Eur J Clin Nutr. 2002; 56:25–32.

35. Bingham SA, Nelson M, Paul AA, Haraldsdóttir J, Løken EB, van Staveren WA. Cameron ME, van Staveren WA, editors. Methods for data collection at an individual level. Manual on methodology for food consumption studies. 1988. New York: Oxford University Press;p. 53–106.
36. AOAC. Official Methods of Analysis. 1990. 16th edition. Arlington V.A: association of official analytical chemist.
37. Temple NJ. Survey of nutrition knowledge of Canadian physicians. J Am Coll Nutr. 1999; 18:26–29. PMID: 10067655.

38. WHO. Physical status: the use and interpretation of anthropometry, Report of a WHO Expert Committee. 1995. Geneva:
39. Awoyinka A, Adeyemi IA, Ojolo BO. Infant feeding in Nigeria: a case study of practices in Ile-Ife community. Early Child Dev Care. 1992; 80:21–29.

40. Cornia Giovanni Andrea. Poverty, food consumption, and nutrition during the transition to the market economy in Eastern Europe. American Economic Review. 1994; 84:297–302.
41. Al-Shoshan AA. Factors affecting mother's choices and decisions related to breast feeding practices and weaning habits. Pakistan Journal of Nutrition. 2007; 6:318–322.
42. Aregai WG. Determinants of weaning practices. Ethiopian Journal of health development. 2000; 14:183–189.

43. Sachdev PHS, Krishna J, Puri RK, Satyanarayana L, Kumar S. Water supplementation in exclusively breastfed infants during summer in the tropics. Lancet. 1992; 337:929–933. PMID: 1678028.

44. WHO/UNICEF. Innocenti Declaration on the protection, promotion and support of breastfeeding. 1990. Geneva:
45. Achidi E, Perlmann H, Salimonu L, Perlmann P, Walker O, Asuzu M. A longitudinal study of seroreactivities to Plasmodium falciparum antigens in Nigerian infants during their first year of life. Acta Trop. 1995; 59:173–183. PMID: 7676908.

46. Cohen RJ, Brown KH, Canahauti J, Rvera L, Dewey KG. Effects of age of introduction of complementary foods on infant breast milk intake, total energy intake and growth: a randomized intervention study in Honduras. Lancet. 1994; 344:288–293. PMID: 7914260.
Fig. 1
Estimated average energy and nutrient intakes of the nursing mothers. Sources of RDA: National Academy of Sciences [47-50]




 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download