Abstract
To investigate the neuroprotective effects of bovine colostrums (BC), we evaluate the ability of consuming BC after focal brain ischemia/reperfusion injury rat model to reduce serum cytokine levels and infarct volume, and improve neurological outcome. Sprague-Dawley rats were randomly divided into 4 groups; one sham operation and three experimental groups. In the experimental groups, MCA occlusion (2 h) and subsequent reperfusion (O/R) were induced with regional cerebral blood flow monitoring. One hour after MCAO/R and once daily during the experiment, the experimental group received BC while the other groups received 0.9% saline or low fat milk (LFM) orally. Seven days later, serum pro-inflammatory cytokine (IL-1β, IL-6, and TNF-α) and anti-inflammatory cytokine (IL-10) levels were assessed. Also, the infarct volume was assessed by using a computerized image analysis system. Behavioral function was also assessed using a modified neurologic severity score and corner turn test during the experiment. Rats receiving BC after focal brain I/R showed a significant reduction (-26%/-22%) in infarct volume compared to LFM/saline rats, respectively (P < 0.05). Serum IL-1β, IL-6, and TNF-α levels were decreased significantly in rats receiving BC compared to LFM/saline rats (P < 0.05). In behavioral tests, daily BC intake showed consistent and significant improvement of neurological deficits for 7 days after MCAO/R. BC ingestion after focal brain ischemia/reperfusion injury may prevent brain injury by reducing serum pro-inflammatory cytokine levels and brain infarct volume in a rat model.
Ischemic stroke resulting from a major cerebral artery occlusion, especially the middle cerebral artery (MCA), by a thrombus or embolism comprise most stroke cases [1]. These strokes are a leading cause of death and severe disability, and place a large burden on healthcare and social service resources in most countries [2,3]. The most adequate treatment for acute stroke in humans is immediate canalization of occluded arteries [4]. Reperfusion of the ischemic region may paradoxically exacerbate brain damage via reperfusion injury [5,6]. Ischemia/reperfusion (I/R)-induced brain damage results from NMDA (N-methyl D-aspartate)-induced excitotoxicity and altered intracellular Ca2+ homeostasis [7]. Secondary injury can be result from reactive oxygen species (ROS) formation, inflammatory cytokine release, and failed energy metabolism [8-10]. Successful neuroprotective agents should interfere with inflammatory reactions in the ischemic brain tissue.
Bovine colostrum (BC, the first milk produced after birth) contains many biologically active substances with various functions, such as immunoglobulins, anti-bacterial peptides, and various growth substances [11]. BC is known to be effective in improving or preventing lapses in diseases such as short bowel syndrome, chemotherapy-induced mucositis, inflammatory bowel disease, necrotizing enterocolitis, non-steroidal anti-inflammatory drugs (NSAIDs) induced intestinal injury, liver disease, and infective diarrhea [12,13]. Recently, in vivo studies have reported that BC decreases serum tumor necrosis factor (TNF-α) and interleukin (IL-1β) levels following rat lung tissue intestinal ischemia/reperfusion injury [14]. This result indicates that BC may have anti-cytokine and anti-inflammatory effects. Few in vivo studies have examined the neuroprotective effect of BC on rat brains affected by I/R.
This study aimed to evaluate whether BC consumption after rat focal brain ischemia/reperfusion injury reduces serum cytokine levels and brain infarct volume, and improves neurological outcome.
The study was conducted in accordance with the Korean Academy of Medical Sciences. Animals were generally anesthetized and monitored following corresponding standard procedures (Laboratory Animal Manual 2000, Korean Academy of Medical Sciences, Seoul). All experimental procedures were approved by the Kyung Hee University Medical Center Institutional Animal Care and Use Committee, Seoul. Thirty seven Sprague-Dawley rats weighting 295 ± 8 g (mean ± standard deviation, 9 weeks old) were used. Animals were purchased from Samtako Bio Korea Co., Ltd. (Gyeonggi-do, Republic of Korea). A 1-week acclimation period to an inverse day and night rhythm (7 p.m.-7 a.m.) was used before animals were used in the experimental protocol. Rats were kept at a constant room temperature (24℃) and humidity (55-70%), and received standard rat chow and tap water ad libitum.
The rats were randomly assigned to four groups: (1) sham group (n = 9) received a sham operation, (2) saline group (n = 12) had middle cerebral artery occlusion/reperfusion (MCAO/R) operation and received 6 mL/kg saline perorally, (3) low fat milk (LFM) group (n = 8) had occlusion/reperfusion (MCAO/R) operation and received 12 mL/kg LFM perorally, (4) and BC group (n = 8) had occlusion/reperfusion (MCAO/R) operation and received 6 mL/kg defatted liquid BC (Percoba liquid, Immuno Dynamics, Ltd., Perry, IA, USA) perorally. Saline, FLM, and BC were administered once daily, perorally for seven days. The rat chow contained 19.5 g/100 g protein, no albumin, 60.6 g/100 g carbohydrate, 10 g/100 g fat, and 4.08 kcal/100 g calories. The BC diet had 6.0 g/dL protein, 2.0 g/dL albumin, 10 g/100 g carbohydrate, < 0.1 g/dL fat, and 64 kcal/dL calories. The LFM formulation had 3.0 g/dL protein, no albumin, 5 g/dL carbohydrate, 1.0 g/dL fat, and 40 kcal/dL calories, which was adjusted to have half the protein and approximately two-thirds the calories of BC.
Rats were treated between 10:00 and 12:00 to avoid non-specific effects due to the circadian rhythm. Behavioral functions were evaluated at 1, 3, and 7 days after operation. Seven days following the operation, rats were anesthetized by 5% isoflurane inhalation and blood samples were withdrawn by cardiocentesis. Rats were then sacrificed by decapitation and brains were removed to measure infarct volume.
Each rat was anesthetized with isoflurane (initiated at 5% and maintained at 2%) in 30% oxygen and 70% nitrous oxide using a vaporizer and face mask. The rat was mounted in the prone position on a dual small animal stereotaxic instrument (David Kopf Instruments, Los Angeles, CA, USA). After cranial midline incision, a 1-mm burr hole was made with microdrill on both sides, 2-mm-posterior and 5-mm-lateral to bregma [15], and the rat was placed in the supine position. A laser Doppler probe was placed on the burr hole under the rat skull, nearly contacting the dura mater and avoiding large vessels, and measured the parietal cortical perfusion in the MCA territory. The laser Doppler probe was connected to BLF21D laser Doppler flowmeter (Transonic systems Inc., Ithaca, NY, USA), and values were obtained beginning 10 minutes before the ischemic event until 15 min after reperfusion [16]. The changes in regional cerebral blood flow (rCBF) were expressed as percentages of baseline values. Signals were digitized for recording, storage and analysis.
After the laser Doppler probe was placed on the skull, left middle cerebral artery occlusion (MCAO) was induced as described by Zea Longa et al. (1989) and revised by Lourbopoulos (2008) [17,18]. The left common carotid artery (CCA) and external carotid artery (ECA) were exposed under an operation microscope followed by electrical coagulation of ECA branches. The internal carotid artery (ICA) was dissected to the level of the pterygopalatine artery. After the distal ECA was ligated permanently, a silk thread (6-0) was placed loosely around the ECA stump. The CCA and ICA were occluded temporarily using microvascular clips. A small incision was made on the ECA, and a 25-mm nylon thread (4-0), with a rounded tip and silicon rubber cylinder (300-340 µm in diameter) was inserted. The silk thread was held around the ECA stump to prevent bleeding, and the microvascular clip on the ICA was removed. The nylon thread in the ECA was gently advanced through the ICA until Laser Doppler Flowmetry showed a sharp decrease in regional blood flow in the MCA to approximately 20% of baseline, as determined by monitoring [19]. The microvascular clip on the CCA was removed and the incision closed. Two hours after inducing ischemia, reperfusion was performed by removing the nylon thread from the ICA under enflurane anesthesia as described above. Restoration of blood flow was identified in the operation field and confirmed by laser Doppler flowmetry. Animals in the sham operation group were subjected to the same operation without inserting the nylon filament. Rectal temperature was monitored continuously and maintained at 37.0 ± 0.5℃ using an electrical blanket and heating lamp throughout the experiment.
Extracted brains from sacrificed rats were chilled in ice-cold saline for 5 min, and sectioned coronally into six 2-mm slices using a rat brain matrix (RBM-4000C, ASI® Instruments Inc., Warren, MI, USA). The slices were then immersed in saline solution containing 2% 2,3,5-triphenyltetrazolium chloride (TTC; Sigma, St. Louis, MO, USA) for 30 min at 37℃ in the dark, followed by 10% buffered formalin fixation [16]. Brain slices were photographed using a digital camera (Camedia C-5060WZ, Olympus Corporation, Tokyo, Japan) and infarct areas were quantified using an image analysis system (Optimas 6.5 Media Cybermetics, Silver Springs, MD, USA). The infarct area in each slice was calculated by subtracting the normal (ipsilateral) area from the contralateral hemisphere to reduce errors due to cerebral edema, and was presented as a percentage of normal [20].
Serum IL-1β, TNF-α, IL-6, and IL-10 concentrations were measured with commercially available quantitative sandwich enzyme-linked immunosorbent assay (ELISA) kits (Quantikine M, R&D Systems Inc. Minneapolis, MN, USA). The change in absorbance in each well at 450 nm was measured with a microplate reader (model ELx800; Bio-Tek Instruments Inc., Winooski, VT, USA) and levels were expressed as picograms per milliliter.
Tests were performed by a blinded investigator at predetermined times to exclude behavioral changes associated with the circadian rhythm.
The modified neurologic severity scores (mNSS) is a composite of motor, sensory (visual, tactile and proprioceptive), and reflex tests. Neurological function was graded on a scale of 0-18 (normal score 0; maximal deficit score 18). One point is awarded for the inability to perform a test or the lack of a tested reflex; thus, a higher score denotes a more severe injury [21].
In the corner test, a rat was placed between two 30 cm×20 cm×1 cm boards. The edges of the boards were attached at a 30° angle with a small opening between the boards to encourage entry into the corner. The rat was placed between the two angled boards facing the corner and halfway to the corner. When the rat reached the corner, both sides of the body were simultaneously stimulated. Then the animal usually reared and turned either right or left. Each animal was tested in 10 trials, and the chosen sides for turning were noted. In the case of ventral turning (i.e., when the animal turned without rearing), the trial was discarded and repeated at the end of the session. The laterality index was calculated according to the formula: Laterality index = (number of left turns-number of right turns) / total number of turns [22].
All data were given as mean ± SE values. Differences between groups were evaluated by analysis of variance (ANOVA) followed by Student-Newman-Keuls multiple comparison test. Statistical analyses were performed with SPSS for Windows 13.0 software (SPSS Inc., Chicago, IL). Differences between two groups were compared by Student's t-test. A P value < 0.05 was considered statistically significant.
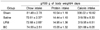
Average body weights were increased to approximately 285-330 g during the experimental period. Rat chow intake was decreased significantly in saline and LFM groups compared to the sham group (P < 0.05), but there was no significant difference between sham and BC groups. Protein and calorie intakes were similar among all groups (Table 1).
The regional cerebral blood flow (rCBF) was decreased during MCAO and showed the same basic patterns in all three operation groups. The rCBF reduction during MCAO tended to be slightly less severe in the LFM group compared with the saline or BC groups (LFM, 24.5 ± 4.5% of baseline; Saline, 20.5 ± 2.5% of baseline; BC, 20.3 ± 2.6% of baseline), but there were no significant differences among the MCAO/R groups (P > 0.05). rCBF was also increased following the same basic pattern for after 10 minutes MCAR with no significant differences among groups (P > 0.05) (Fig. 1).
MCAO/R made large infarct in the saline group (40.863 ± 4.907%). LFM (37.073 ± 6.604%) did not reduce the infarct volume significantly compared with the saline group (P = 0.625). BC rats (15.003 ± 3.672%) showed a significant reduction of brain infarct volume compared with saline (P < 0.005) and LFM rats (P < 0.05) (Fig. 2A and B).
The saline and LFM groups showed significantly elevated serum TNF-α levels compared to the sham group (P < 0.005 vs. saline; P < 0.001 vs. LFM). The BC group had significantly lower serum TNF-α than the saline/LFM groups (P < 0.05 vs. saline; P < 0.01 vs. LFM) (Fig. 3A). The saline and LFM groups showed significantly elevated serum IL-1β levels compared to the sham group (P < 0.001). The BC group had significantly lower IL-1β than the saline group (P < 0.001). The BC group had lower IL-1β than the LFM group, but the difference was not significant (P = 0.072) (Fig. 3B). The saline and LFM groups showed significantly elevated serum IL-6 levels compared to the sham group (P < 0.001 vs. Saline; P < 0.005 vs. LFM). The BC group had significantly lower IL-6 than the saline/LFM groups (P < 0.01 vs. saline; P < 0.05 vs. LFM) (Fig. 3C). The saline and LFM groups showed significantly elevated Serum IL-10 levels compared to the sham group (P < 0.01). The BC group had less IL-10 than the saline and LFM groups, but the difference was not significant (P = 0.105 vs. saline; P = 0.088 vs. LFM) (Fig. 3D).
mNSS: One day after MCAO/R injury, all rats in operation groups showed neurologic deficits (saline 10.1 ± 1.02, LFM 10.2 ± 1.33, and BC 10.1 ± 1.60), but there were no significant differences among the groups till 3 days after the operation. Seven days after operation, the BC group (5.4 ± 0.71) scored significantly lower than the saline (9.1 ± 0.97) and LFM (8.4 ± 0.99) groups (P < 0.01 vs. saline group, P < 0.05 vs. LFM group) (Fig. 4A).
Corner test: All rats in operation groups showed higher percentages of right turns (saline 96.5 ± 1.09, LFM 96.4 ± 1.41, and BC 98.1 ± 0.64) at one day after MCAO/R injury, but there were no significant differences among the groups. Three days after the operation, the BC group (82.0 ± 3.32) made significantly fewer right turns compared to the LFM group (92.0 ± 2.61) (P < 0.05). The BC group (76.1 ± 2.72) made significantly fewer right turns than both the saline (88.9 ± 2.54) and LFM (87.6 ± 2.70) groups (P < 0.005 vs. saline group; P < 0.01 vs. LFM group) at 7 days (Fig. 4B).
Inflammation plays a critical role in ischemic brain injury, and anti-inflammatory measures reduce injury and enhance stroke recovery. Moreover, reperfusion after focal brain ischemia increases the inflammatory reactions [6,23-25]. The major players in initiating and modulating the post-ischemic inflammatory response are inflammatory cytokines. Proinflammatory cytokines, such as tissue necrosis factor-α (TNF-α), interleukin (IL)-1β, and IL-6 contribute to pathogenesis, exacerbating ischemic-reperfusion brain tissue damage [26,27]. If ischemia activates these cytokines, there will be increments of inducible NO synthase, cyclooxygenase-2 (COX-2), endothelial adhesion molecules and various chemokine productions. This process induces neutrophil adhesion, migration, and activation that raise brain tissue inflammation and destruction [28]. On the contrary, anti-inflammatory cytokines, such as IL-10, can provide neuroprotection and tissue repair in ischemic stroke [26]. IL-10 also seems to prevent elevated TNF-α, IL-6, and IL-18 levels induced by lipopolysaccharide [29], but the IL-10 concentration correlates with the SIRS magnitude and elevated systemic levels are associated with poor outcome [30].
BC is a source of immune components and nutrients for neonatal calves and contains large amounts of protein, immunoglobulins, growth factors, non-protein nitrogen, fat, ash, vitamins, and minerals [31,32]. Protein-energy nutrition after acute stroke is a risk factor for poor outcome [33]. An LFM group was included in this study to prevent confounding BC and nutrition effects due to protein and calorie intake. The results showed that the total protein and calorie intake among MCAO/R groups were not significantly different. Several cytokines also have been found in BC, including both pro-inflammatory cytokines such as IL-1β, IL-6, TNF-α, IFN-γ [34,35] as well as anti-inflammatory components, such as IL-1ra, sIL-1RII and sCD14 [35-37]. This suggests that BC may provide the infant both with cytokines to promote activation/inflammation and the means to reduce it.
In vitro, BC is known to modulate cytokine secretion from lymphocytes and monocytes [38], and inhibit cyclooxygenase-2 (COX-2) expression induced by IL-1β in HT-29 cells [39]. Therefore, this in vivo study analyzed three pro-inflammatory (TNF-α, IL-1β, and IL-6) and one anti-inflammatory (IL-10) cytokines to evaluate the influence of BC on cytokines in the rat MCAO/R model. Serum TNF-α, IL-1β, and IL-6 concentrations were increased significantly in MCAO/R groups and decreased remarkably after BC administration. Therefore, BC might regulate pro-inflammatory cytokine activation during inflammatory responses after reperfusion in vivo. The IL-10 serum concentration was also increased significantly in the MCAO/R groups and decreased marginally after BC administration. These results correspond with earlier studies that reported that IL-10 increases during early stage after post-ischemia and might inhibit proinflammatory cytokine release via negative feedback [27,40,41].
MCAO/R may cause cerebral cell death, resulting in local infarction. The infarct area represents the degree of brain injury. In the present study, rats administered 6 mL/kg BC perorally for 7 days after MCAO/R showed a 25.86% and 22.07% reduction in infarction volume versus saline and LFM administered rats, respectively. These findings show that BC reduces the MCAO-induced cerebral infarct, demonstrating that BC protects against cerebral ischemia/reperfusion injury. This efficacy may be attributed to the many anti-inflammatory substances in BC, such as lactoferrin [42].
The brain injury induced by MCAO/R leads to neurobehavioral impairment. We performed the modified neurologic severity score (mNSS) and corner turn tests to measure neurobehavioral changes. The mNSS is sensitive to unilateral cortical injury because it reflects multiple asymmetries, including postural, sensory, and limb use [43,44]. The corner turn test detects sensorimotor and postural asymmetries [22]. The non-ischemic rats turned either left or right, but the ischemic rats preferentially turned toward the unimpaired, ipsilateral (right) side [45]. In this study, all rats in the operation (MCAO/R) groups showed a neurologic deficit after MCAO/R injury. The mNSS and corner tests showed that MCAO/R-induced impaired neurologic function was maximal 24 h after reperfusion and progressively improved until 7 days post-MCAO/R. At 7 days the BC group was improved remarkably compared to the saline and LFM groups. These results were likely in association with the infarct volume, which was decreased in BC-feeding rats.
In the present study, we examined the neuroprotective effects of BC on a MCAO/R rat model. This is the first report, to our knowledge, describing the effects of BC on a rat brain injured by transient ischemia. Although this study does not include a human model, these results suggest that BC ingestion after brain ischemia/reperfusion injury may prevent secondary brain injury and promote recovery from the insult. Supplementary studies evaluating oxidative stress and/or neurotransmitter release are expected to compensate for the limitations found here. This study demonstrates that BC consumption inhibits proinflammatory cytokine release (TNF-α, IL-1β, and IL-6) and may promote anti-inflammatory cytokine release (IL-10) in rat serum 7 days after MCAO/R injury. These effects are likely to contribute to reducing the infarct lesion volume and degree of neurobehavioral change.
Figures and Tables
Fig. 1
Representative changes in regional cerebral blood flow (rCBF) during MCAO/R among saline (SAG), low fat milk (LFMG), and bovine colostrum groups (BCG). The rCBF decreased similarly in SAG, LFMG, and BCG during MCAO and increased similarly in all groups after MCAR (P > 0.05, n = 8 to 12). Values are mean ± SEM ; n = 8 to 12.

Fig. 2
Effects of treatment with saline, LFM, and BC on brain infarct volume in rats. (A) Representative photographs of TTC staining 7 days after MCAO/R. Infarct volume in sham operation (SHG), saline (SAG), low fat milk (LFMG), and bovine colostrum groups (BCG). (B) Brain infarct volume in BCG was smaller than SAG and LFMG. Values are mean ± SEM ; n = 8 to 12 (*P < 0.001 vs SAG; †P < 0.01 vs LFMG).

Fig. 3
Cytokine responses following MCAO/R injury. Serum levels of (A) TNF-α, (B) IL-1β, (C) IL-6, and (D) IL-10 in each rat group were measured from blood samples withdrawn 7 days after MCAO/R. Serum cytokine levels in the sham operation (SHG), saline (SAG), low fat milk (LFMG), and bovine colostrum groups (BCG). Values are mean ± SEM ; n = 8 to 12 (*P < 0.01, **P < 0.005, ***P < 0.001 vs SHG; †P < 0.05, ††P < 0.01 vs SAG; ‡P < 0.05, ‡‡P < 0.01 vs LFMG).

Fig. 4
Behavioral function tests. Neurological deficit was evaluated in the sham operation (SHG), saline (SAG), low fat milk (LFMG), and bovine colostrum groups (BCG) just before and 1, 3, and 7 days after MCAO/R using modified neurological severity scores (mNSS) graded on a 0 to 18 scale (0, no neurologic deficit; 18, maximal deficit) (A) and corner turn test (B). Values are mean ± SEM ; n = 8 to 12 (*P < 0.01, **P < 0.005 vs SAG; †P < 0.05, ††P < 0.01 vs LFMG).

References
1. Green AR, Shuaib A. Therapeutic strategies for the treatment of stroke. Drug Discov Today. 2006. 11:681–693.

2. Feigin VL, Lawes CM, Bennett DA, Anderson CS. Stroke epidemiology: a review of population-based studies of incidence, prevalence, and case-fatality in the late 20th century. Lancet Neurol. 2003. 2:43–53.

3. Plaisier F, Bastide M, Ouk T, Pétrault O, Laprais M, Stolc S, Bordet R. Stobadine-induced hastening of sensorimotor recovery after focal ischemia/reperfusion is associated with cerebrovascular protection. Brain Res. 2008. 1208:240–249.

4. The National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995. 333:1581–1587.
5. Hallenbeck JM, Dutka AJ. Background review and current concepts of reperfusion injury. Arch Neurol. 1990. 47:1245–1254.

7. Xiao ZY, Sun CK, Xiao XW, Lin YZ, Li S, Ma H, Song GR, Cheng R. Effects of Ginkgo biloba extract against excitotoxicity induced by NMDA receptors and mechanism thereof. Zhonghua Yi Xue Za Zhi. 2006. 86:2479–2484.
8. Saleem S, Zhuang H, Biswal S, Christen Y, Doré S. Ginkgo Biloba extract neuroprotective action is dependent on heme oxygenase 1 in ischemic reperfusion brain injury. Stroke. 2008. 39:3389–3396.

9. Chan PH. Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cereb Blood Flow Metab. 2001. 21:2–14.

11. Chun S, Nam M, Goh J, Kim W, Han Y, Kim P. Kinetics and biological function of transforming growth factor-β isoforms in bovine and human colostrum. J Microbiol Biotechnol. 2004. 14:1267–1274.
12. Playford RJ. Peptide therapy and the gastroenterologist: colostrum and milk-derived growth factors. Clin Nutr. 2001. 20:101–106.

13. Playford RJ, Floyd DN, Macdonald CE, Calnan DP, Adenekan RO, Johnson W, Goodlad RA, Marchbank T. Bovine colostrum is a health food supplement which prevents NSAID induced gut damage. Gut. 1999. 44:653–658.

14. Choi HS, Jung KH, Lee SC, Yim SV, Chung JH, Kim YW, Jeon WK, Hong HP, Ko YG, Kim CH, Jang KH, Kang SA. Bovine colostrum prevents bacterial translocation in an intestinal ischemia/ reperfusion-injured rat model. J Med Food. 2009. 12:37–46.

15. Sun H, Zhao H, Sharpe GM, Arrick DM, Mayhan WG. Effect of chronic alcohol consumption on brain damage following transient focal ischemia. Brain Res. 2008. 1194:73–80.

16. Zhang Y, Wang L, Li J, Wang XL. 2-(1-Hydroxypentyl)-benzoate increases cerebral blood flow and reduces infarct volume in rats model of transient focal cerebral ischemia. J Pharmacol Exp Ther. 2006. 317:973–979.

17. Longa EZ, Weinstein PR, Carlson S, Cummins R. Reversible middle cerebral artery occlusion without craniectomy in rats. Stroke. 1989. 20:84–91.

18. Lourbopoulos A, Karacostas D, Artemis N, Milonas I, Grigoriadis N. Effectiveness of a new modified intraluminal suture for temporary middle cerebral artery occlusion in rats of various weight. J Neurosci Methods. 2008. 173:225–234.

19. Chen H, Song YS, Chan PH. Inhibition of NADPH oxidase is neuroprotective after ischemia-reperfusion. J Cereb Blood Flow Metab. 2009. 29:1262–1272.

20. Swanson RA, Morton MT, Tsao-Wu G, Savalos RA, Davidson C, Sharp FR. A semiautomated method for measuring brain infarct volume. J Cereb Blood Flow Metab. 1990. 10:290–293.

21. Chen J, Li Y, Wang L, Zhang Z, Lu D, Lu M, Chopp M. Therapeutic benefit of intravenous administration of bone marrow stromal cells after cerebral ischemia in rats. Stroke. 2001. 32:1005–1011.

22. Haelewyn B, Freret T, Pacary E, Schumann-Bard P, Boulouard M, Bernaudin M, Bouët V. Long-term evaluation of sensorimotor and mnesic behaviour following striatal NMDA-induced unilateral excitotoxic lesion in the mouse. Behav Brain Res. 2007. 178:235–243.

23. Lee DH, Ha N, Bu YM, Choi HI, Park YG, Kim YB, Kim MY, Kim H. Neuroprotective effect of Buddleja officinalis extract on transient middle cerebral artery occlusion in rats. Biol Pharm Bull. 2006. 29:1608–1612.

24. del Zoppo G, Ginis I, Hallenbeck JM, Iadecola C, Wang X, Feuerstein GZ. Inflammation and stroke: putative role for cytokines, adhesion molecules and iNOS in brain response to ischemia. Brain Pathol. 2000. 10:95–112.

25. Allan SM, Rothwell NJ. Cytokines and acute neurodegeneration. Nat Rev Neurosci. 2001. 2:734–744.

26. Li TJ, Qiu Y, Mao JQ, Yang PY, Rui YC, Chen WS. Protective effects of Guizhi-Fuling-Capsules on rat brain ischemia/ reperfusion injury. J Pharmacol Sci. 2007. 105:34–40.

29. Pajkrt D, van der Poll T, Levi M, Cutler DL, Affrime MB, van den Ende A, ten Cate JW, van Deventer SJ. Interleukin-10 inhibits activation of coagulation and fibrinolysis during human endotoxemia. Blood. 1997. 89:2701–2705.

30. Scumpia PO, Moldawer LL. Biology of interleukin-10 and its regulatory roles in sepsis syndromes. Crit Care Med. 2005. 33:S468–S471.

31. Quigley JD 3rd, Drewry JJ. Nutrient and immunity transfer from cow to calf pre- and post-calving. J Dairy Sci. 1998. 81:2779–2790.

32. Kelly GS. Bovine colostrums: a review of clinical uses. Altern Med Rev. 2003. 8:378–394.
33. Dávalos A, Ricart W, Gonzalez-Huix F, Soler S, Marrugat J, Molins A, Suñer R, Genís D. Effect of malnutrition after acute stroke on clinical outcome. Stroke. 1996. 27:1028–1032.

34. Goto M, Maruyama M, Kitadate K, Kirisawa R, Obata Y, Koiwa M, Iwai H. Detection of nterleukin-1 beta in sera and colostrum of dairy cattle and in sera of neonates. J Vet Med Sci. 1997. 59:437–441.

35. Hagiwara K, Kataoka S, Yamanaka H, Kirisawa R, Iwai H. Detection of cytokines in bovine colostrum. Vet Immunol Immunopathol. 2000. 76:183–190.

36. Filipp D, Alizadeh-Khiavi K, Richardson C, Palma A, Paredes N, Takeuchi O, Akira S, Julius M. Soluble CD14 enriched in colostrum and milk induces B cell growth and differentiation. Proc Natl Acad Sci U S A. 2001. 98:603–608.

37. Hagiwara K, Kitajima K, Yamanaka H, Kirisawa R, Iwai H. Development of a sandwich ELISA assay for measuring bovine soluble type II IL-1 receptor (IL1R2) concentration in serum and milk. Cytokine. 2005. 32:132–136.

38. Shing CM, Peake JM, Suzuki K, Jenkins DG, Coombes JS. Bovine colostrum modulates cytokine production in human peripheral blood mononuclear cells stimulated with lipopolysaccharide and phytohemagglutinin. J Interferon Cytokine Res. 2009. 29:37–44.

39. An MJ, Cheon JH, Kim SW, Park JJ, Moon CM, Han SY, Kim ES, Kim TI, Kim WH. Bovine colostrum inhibits nuclear factor κB-mediated proinflammatory cytokine expression in intestinal epithelial cells. Nutr Res. 2009. 29:275–280.

40. Peroulis N, Kourounakis AP, Yiangou M, Paramythiotis D, Kotzampassi K, Hadjipetrou L. Effects of the novel non-steroidal anti-inflammatory compound [N-(2-Thiolethyl)-2-{2-[N'-(2,6-dichlorophenyl) amino]phenyl}acetamide on cytokines and apoptosis in ischaemic rat brain. Arzneimittelforschung. 2006. 56:688–694.

41. Kim KY, Kim MY, Choi HS, Jin BK, Kim SU, Lee YB. Thrombin induces IL-10 production in microglia as a negative feedback regulator of TNF-α release. Neuroreport. 2002. 13:849–852.

42. Hayashida K, Kaneko T, Takeuchi T, Shimizu H, Ando K, Harada E. Oral administration of lactoferrin inhibits inflammation and nociception in rat adjuvant-induced arthritis. J Vet Med Sci. 2004. 66:149–154.

43. Li Y, Chen J, Chen XG, Wang L, Gautam SC, Xu YX, Katakowski M, Zhang LJ, Lu M, Janakiraman N, Chopp M. Human marrow stromal cell therapy for stroke in rat: neurotrophins and functional recovery. Neurology. 2002. 59:514–523.





 PDF
PDF ePub
ePub Citation
Citation Print
Print


 XML Download
XML Download