Abstract
Adequate nutrient intake during pregnancy is important to fetal and maternal health. The purpose of this study was to investigate the factors affecting birth weight and gestational age and to provide basic data to promote more favorable pregnancy outcomes. Data were collected from 234 pregnant women at two hospitals in Seoul. Demographic characteristics, anthropometric measurements and health related habits were obtained using a questionnaire at the hospital visit during the second trimester. Dietary intakes were estimated by 24 hour recall at the hospital visit during the second trimester. Data on pregnancy outcomes, including birth weights and gestational ages, were obtained from hospital records after delivery. Birth weights were divided into a low birth weight group (birth weight<3.1 kg), a normal birth weight group (3.1-3.6 kg) and a high birth weight group (>3.6 kg). Gestational ages were divided into tertiles according to the gestational age of the subjects: group 1 (<38.53 weeks), group 2 (38.53-40.00 weeks) and group 3 (>40.00 weeks). The number of family members was significantly lower in the low birth weight group than in the normal birth weight group (p<0.05). In the low birth weight group, pregnancy weight was significantly lower than in the high birth weight group (p<0.05). Health related habits were not significantly different among any of the groups. Intakes of fiber, phosphorous, iron, vitamin B6 and folic acid were significantly higher in the high birth weight group than the low birth weight group (p<0.05). Gestational age was not significantly affected by nutrient intakes, but birth weight was affected by nutrient intake in the results of this study. Therefore, the adequacy of nutrient intake is important for the improvement of pregnancy outcomes.
Maternal nutrition is an important factor responsible not only for the health of the baby, but also for the baby's long term growth (Jackson & Robinson, 2001). Pregnancy outcomes are affected by other factors as well as nutrient intake. These factors are age, occupation, family, pregnancy experiences and morning sickness (Freisling et al., 2006; Laraia et al., 2006). Maternal anthropometric measurements, smoking, alcohol consumption, coffee consumption, stress and physical activity are also factors affecting pregnancy outcome (Anahita et al., 1998; Haste et al., 1990; Kramer et al., 2000).
Previously, research was performed addressing fetal programming which results from the adaptive changes in gene expression patterns that occur in response to stressors such as poor maternal nutritional status, leading to the altered growth of specific organs and systems during their most critical time of development (Barker, 1998). Indeed, the prenatal environment exerts profound influences on the development of an organism, and stressful events during pregnancy can induce alterations in the fetal environment resulting in early and long-term structural and functional consequences (Maccari et al., 2003; Wadhwa et al., 2001; Weinstock, 1997).
Therefore, nutrition is an important health determinant that can affect the course of pregnancy and its outcomes. Optimal nutritional status during pregnancy is reflected not only in the improved health of the mother but also in the improved health of the baby (Rush, 2004; Siega-Riz et al., 2001).
In Korea, the available information on pregnancy outcomes related to nutrient intake is not sufficient.
The purpose of this study was to investigate the factors affecting birth weight and gestational age and to provide basic data to promote more favorable pregnancy outcomes.
Four hundred and three pregnant women in second trimester (20-36 week) participated in this follow-up study, but only 234 pregnant women who could provide information on birth weight and gestational age were included in the analyses. The data collection was initiated in April 2006 and was completed in August 2008. Women who consented to participate were recruited from their visits to the Ewha Women's University Hospital and the Miz-Medi Hospital in Seoul, Korea.
Demographic characteristics, anthropometric measurements and health related habits were collected by individual interviews using a questionnaire at the hospitals visit during the second trimester. The demographic characteristics were age, occupation status, number of family members, pregnancy experiences and morning sickness. Weight-gain during pregnancy was calculated by subtracting the pre-pregnancy weight from the pregnancy weight at the second trimester. The pre-pregnancy BMI was calculated using the measured height and self reported pre-pregnancy weight. The health related habits surveyed were smoking, alcohol consumption, coffee consumption, stress, and level of physical activity. The level of stress was measured with a questionnaire developed by Holemes and Rache (1967). Out of a total score of 41, scores above 12 were classified as the high stress group and scores below 12 were classified as the low stress group (Choi et al., 2001; Kim & Lee, 2008).
Dietary intakes were estimated by the 24-hour recall method for 1 day and were conducted by trained field workers with the help of food models to estimate portion size at the second trimester. Nutrient intakes were calculated using CAN-PRO version 3.0 (Korean Nutrition Society, Seoul, Korea). The consumption of dietary supplements was not investigated.
Information on birth weight and gestational age was obtained from hospital records after delivery. The birth weights were divided into three groups according to the WHO standard (Bulletin of the World Health Organization, 1995): a low birth weight group (birth weight<3.1 kg), a normal birth weight group (3.1-3.6 kg), and a high birth weight group (>3.6 kg). Gestational age was divided into tertiles according to the gestational age of the subjects: group 1 (<38.53 week), group 2 (38.53-40.00 week) and group 3 (>40.00 week).
The statistical analysis of data was conducted using SPSS for Windows version 12.0. The statistical differences among the three groups were analyzed by ANOVA, and when significant, they were verified through the Scheffe's test. The results presented are the mean with standard deviations. The Chi-square test was used to test the significance of the distribution rate within the groups and the results presented are the percentages. Results were considered significant if p<0.05.
Based on the WHO standards (3.1-3.6 kg), birth weight was divided into three groups: the low birth weight group (birth weight <3.1 kg), the normal birth weight group (3.1-3.6 kg) and the high birth weight group (>3.6 kg) (Bulletin of the World Health Organization, 1995). The subjects' ages were between 24 and 38 years. No significant differences were found in age, occupation status, morning sickness and pregnancy experiences among the groups (Table 1). The number of family members were 2.6 ± 0.7 persons in the low birth weight group, 2.9 ± 1.0 persons in the normal birth weight group and 2.9 ± 0.9 persons in the high birth weight group. The low birth weight group had significantly fewer family members than the normal birth weight group (p<0.05).
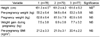
The results of the anthropometric measurements are listed in Table 2. Height and pre-pregnancy weight were not significantly different among the groups. The pregnancy weight of the low birth weight group, normal birth weight group and high birth weight group was 60.0 ± 7.6 kg, 62.4 ± 7.4 kg and 63.5 ± 6.6 kg, respectively. The pregnancy weight was significantly higher in the high birth weight group than the low birth weight group (p<0.05). No significant differences were found in weight gain during pregnancy and pre-pregnancy BMI.
Health related habits such as smoking, alcohol consumption, coffee consumption, stress, level of physical activity and regular exercise were not significantly different among the groups (Table 3).
The nutrient intakes of each group are shown in Table 4. No significant difference was found in nutrient intake except for fiber, phosphorous, iron, vitamin B6 and folic acid. The fiber intake of the low birth weight group, normal birth weight group and high birth weight group were 19.7 ± 6.6 g, 21.2 ± 6.3 g and 23.0 ± 7.3 g, respectively. The fiber intake was significantly higher in the high birth weight group than in the low birth weight group (p<0.05). The phosphorous intake was 1027.1 ± 324.9 mg, 1123.2 ± 292.9 mg and 1207.5 ± 322.5 mg, in the low, normal and high birth weight groups, respectively. Thus the phosphorous intake was significantly higher in the high birth weight group than the low birth weight group (p<0.05). Iron intake was 12.8 ± 3.1 mg, 14.7 ± 5.1 mg and 15.3 ± 5.0 mg in the low, normal and high birth weight groups, respectively. Iron intake was significantly higher in the high birth weight group than the low birth weight group (p<0.05). Vitamin B6 intake was 2.1 ± 0.7 mg, 2.3 ± 0.7 mg and 2.5 ± 0.9 mg in the low, normal and high birth weight groups, respectively. Thus the vitamin B6 intake was significantly higher in the high birth weight group than the low birth weight group (p<0.05). Folic acid intake was 236.9 ± 96.7 µgDFE, 289.2 ± 108.4 µgDFE and 307.5 ± 139.5 µgDFE in the low, normal and high birth weight groups, respectively. The folic acid intake of the high birth weight group was significantly higher than the low birth weight group (p<0.05).
Normal gestational age is 38-42 week (Park et al., 2004). Because most of the subject's gestational age was within the normal range, the subjects were divided into tertiles according to gestational age: group 1 (<38.53 weeks), group 2 (38.53-40.00 weeks) and group 3 (>40.00 weeks). The three gestational age groups showed no significant difference in demographic characteristics (Table 5), anthropometric measurements (Table 6), health related habits (Table 7) and nutrient intakes (Table 8).
Birth weight and gestational age (especially pre-term birth) cause prenatal mortality. Some studies have reported that age, occupation, family, pregnancy experiences and morning sickness, maternal anthropometric measurements, smoking, alcohol consumption, coffee consumption, stress and physical activity, nutrient intake are risk factors for both birth weight and gestational age (Anahita et al., 1998; Freisling et al., 2006; Haste et al., 1990; Kramer et al., 2000; Laraia et al., 2006). The goal of this study was to investigate the demographic, anthropometric, health related habits and nutrient intake of pregnant women and find factors affecting pregnancy outcomes such as birth weight and gestational age.
We found that one demographic characteristic and the number of family members affected birth weight. We thought that the greater number of family members might increase maternal stress, but instead, it seems that pregnant women benefit from their family members' assistance.
Morning sickness did not affect pregnancy outcomes. Yu and Yoon (2007) reported that nutrient intakes in early pregnancy are reduced as a result of morning sickness. Coad et al. (2005) found significantly lower energy and fat intakes in women who suffered from morning sickness, and women who experienced morning sickness during pregnancy had significantly lower intakes of protein, carbohydrates, fiber, vitamin E and D, B vitamins (excluding folic acid), iron and zinc. They suggest, therefore, that interventions are needed to alleviate the symptoms in pregnant women who suffer from morning sickness.
One of the anthropometric measurements, pregnancy weight, also affected birth weight. In most studies, being overweight is an important risk factor indicating possible pregnancy complications (Galtier-Dereure & Boulot, 1994; Galtier-Dereure et al., 2000), the greater the weight gain, the greater the risks (Kajantie, 2005). Women who are underweight may also be at risk for adverse pregnancy outcomes (Conti et al., 1998; Micali et al., 2007; Stewart et al., 1987; Treasure, 1988). Thus, it is especially important to follow the weight gain recommendations. Pregnant women should seek counseling and extra support to ensure appropriate weight gain.
Health related habits play an important role in food choice (Saba & Di Natale, 1999). Fortunately, there were no current smokers or alcohol drinkers in this study. About 10% of the subjects were ex-smokers and about 35% were ex-drinkers. Maternal smoking reduces birth weight and fertility, and it increases the risk of abnormal placentation, spontaneous abortion, preterm delivery and perinatal mortality. Smoking during pregnancy is also known to be strongly associated with sudden infant death syndrome (SIDS) (Mitchell et al., 1993). Alcohol use during pregnancy can cause fetal alcohol syndrome (FAS) or fetal alcohol effects (FAE), characterized by both pre- and post-natal growth retardation, facial deformity, and central nervous system abnormalities (Chiriboga, 2003). Longitudinal research suggests that prenatal alcohol exposure is associated with alcohol disorders in early adulthood (Alati et al., 2006). In this study, about 10% of the subjects consumed more than five cups of coffee per day. Some studies have found high caffeine intake (6-8 cups of coffee per day) to be associated with decreased fertility, increased incidence of spontaneous abortion and low birth weight (Lechat et al., 1980). It was reported that intravillous placental blood flow decreased but fetal umbilical blood flow was unchanged by maternal coffee consumption (Kirkinen et al., 1983). We thought that women who are pregnant, or may become pregnant, should be advised to avoid smoking, alcohol drinking and coffee consumption.
Prenatal stress is associated with a number of adult diseases, including cardiovascular and related disorders. The mechanism underlying this relationship is thought to be exposure of the fetus to components of the stress response (Gale & Martyn, 2004; Kajantie et al., 2005). According to Kim and Lee (2008), stress management is important for pregnant women because stress may lead to reduced nutrient intakes.
Women who exercise during pregnancy have reduced risks of gestational diabetes, hypertensive disease, preeclampsia and preterm birth (Chasan-Taber et al., 2004; Weissgerber et al., 2004), and no study has found any negative effects of moderate exercise on pregnancy outcomes in a healthy pregnancy (Bell et al., 1995; Lokey et al., 1991; Sternfeld et al., 1995). In the results of this study, stress and physical activity did not affect pregnancy outcomes. We think, however, that increasing physical activity levels and finding ways to eliminate stress are important for pregnant women. This may increase the consumption of foods.
Regarding nutrient intake, our results show that fiber and phosphorous intake influenced birth weight. A comparison of fiber and phosphorous in our study with the Korean DRIs (The Korean Nutrition Society, 2005) show that fiber intake was below the Korean DRIs of 29 g and phosphorous intake was above the Korean DRIs of 700 mg. The higher fiber intake of pregnant women is explained by the higher fruit and vegetable consumption. In order to reduce phosphorous intake, we would suggest limiting the amount of processed foods and restaurant foods (Choi et al., 2006).
Comparison of nutrient intakes in our study with the Korean DRIs show that intakes of iron and folic acid in almost all subjects were below their respective Korean DRIs of 24 mg and 600µgDFE. The total intakes of iron and folic acid were not determined because the dietary supplements consumed by the subjects were not investigated in this study. Iron and folic acid affected birth weight in this and other studies. These micronutrients are particularly important to the normal outcome of pregnancy (Caulfield et al., 1998; Green, 2002; Gulson et al., 2001; Steer, 2000). These results lead to the conclusion that the supplementary intake of iron and folic acid should be recommended to pregnant women. It should be remembered, however, that excessive intake of micronutrient supplements causes side effects, and often these supplements interact with specific nutritious elements (Kafatos et al., 1991).
In this study, most of the subjects were included in normal gestational age (38-42 week), so the gestational age was divided into tertiles according to the gestational age of the subjects. As a result, we thought that gestational age was not affected by all factors, however, several studies have reported that preterm delivery (before 37 weeks gestation) is a major contributor to infant morbidity and mortality (Dietz et al., 2006; Wilcox & Skjaerven, 1992).
This study has several limitations. First, respondents were not randomly selected, and were taken from a limited number of geographical areas. Second, dietary intake was analyzed for only one day, which may not reflect the ordinary diet of the subjects.
In conclusion, the present results indicate that adequacy of weight gain and nutrient intake, especially dietary fiber, iron, vitamin B6, and folic acid, are important for the improvement of pregnancy outcomes. The results also suggest that dietary intervention or education should be provided for pregnant women.
Figures and Tables
References
1. Alati R, Al MA, Williams GM, O'Callaghan M, Najman JM, Bor W. In utero alcohol exposure and prediction of alcohol disorders in early adulthood: a birth cohort study. Arch Gen Psychiatry. 2006. 63:1009–1016.

2. Anahita HR, Nasrin O, Mahmood M, Fariba K, Maryam A. Dietary intake, anthropometry and birth outcome of rural pregnant women in two Iranian districts. Nutr Res. 1998. 18:1469–1482.

4. Bell R, Palma S, Lumley J. The effect of vigorous exercise during pregnancy on birthweight. Aust NZ J Obstet Gynaecol. 1995. 35:46–51.

5. Bulletin of the World Health Organization. Maternal Anthropometry and Pregnancy Outcomes: A WHO Collaborative Study. Bull World Health Organ. 1995. 73:1–98.
6. Caulfield LE, Zavaleta N, Shankar AH, Merialdi M. Potential contribution of maternal zinc supplementation during pregnancy to maternal and child survival. Am J Clin Nutr. 1998. 68:499–508.

7. Chasan-Taber L, Schmidt MD, Roberts DE, Hosmer D, Markenson G, Freedson PS. Development and validation of a pregnancy physical activity questionnaire. Med Sci Sports Exerc. 2004. 36:1750–1760.

9. Choi BS, Lee IS, Shin JJ, Park MH. Factors affecting dietary & nutrients intake during the first, second, and third trimesters and pregnancy outcome (2001). Korean Journal of Food Culture. 2001. 16:203–214.
10. Choi HM, Kim JH, Lee JH, Kim CI, Song KH, Jang KJ, Min HS. 21C Nutrition. 2006. Republic of Korea: Kyomunsa.
11. Coad J, Al-Rasasi B, Vassia Morgan JB. Nausea and vomiting in pregnancy is associated with reduced fat intake and altered patterns of maternal fat deposition. Proceedings of the Nutrition Society of New Zealand. 2005. 30:182.
12. Conti J, Abraham S, Taylor A. Eating behavior and pregnancy outcome. J Psychosom Res. 1998. 44:465–477.

13. Dietz PM, Callaghan WM, Cogswell ME, Morrow B, Ferre C, Schieve LA. Combined effects of pre-pregnancy body mass index and weight gain during pregnancy on the risk of preterm delivery. Epidemiology. 2006. 17:170–177.

14. Freisling H, Elmadfa I, Gall I. The effect of socioeconomic status on dietary intake, physical activity and Body Mass Index in Austrian pregnant women. J Hum Nutr Diet. 2006. 19:437–445.

15. Galtier-Dereure F, Boegner C, Bringer J. Obesity and pregnancy: complications and cost. Am J Clin Nutr. 2000. 71:1242–1248.

16. Galtier-Dereure F, Boulot P. Obstetrical complications at maternal overweight. Contracept Fertil Sex. 1994. 22:113–116.
17. Gale CR, Martyn CN. Birth weight and later risk of depression in a national birth cohort. Br J Psychiatry. 2004. 184:28–33.

18. Green N. Folic acid supplementation and prevention of birth defects. J Nutr. 2002. 132:2356–2360.

19. Gulson BL, Mizon KJ, Korsch MJ, Mahaffey KR, Taylor AJ. Dietary intakes of selected elements from longitudinal 6-day duplicate diets for pregnant and nonpregnant subjects and elemental concentrations of breast milk and infant formula. Environ Res Sec. 2001. 87:160–174.

20. Haste FM, Brooke OG, Anderson HR, Bland JM, Shaw A, Griffin Peacock JL. Nutrient intakes during pregnancy: Observations on the influence of smoking and social class. Am J Clin Nutr. 1990. 51:29–36.

22. Jackson AA, Robinson SM. Dietary guidelines for pregnancy: a review of current evidence. Public Health Nutr. 2001. 4:625–630.

23. Kafatos AG, Tsitoura S, Pantelakis SN, Doxiadis SA. Maternal and infant health education in a rural Greek community. Hygie. 1991. 10:32–37.
24. Kajantie E, Osmond C, Barker DJ, Forsen T, Phillips DI, Eriksson JG. Size at birth as a predictor of mortality in adulthood: a follow-up of 350,000 person-years relief of stress. Int J Epidemiol. 2005. 34:655–663.

25. Kim YJ, Lee SS. The relation of maternal stress with nutrients intake and pregnancy outcome in pregnant women. The Korean Journal of Nutrition. 2008. 41:776–785.
26. Kirkinen P, Jouppila P, Koivula A, Vuori J, Puukka M. The effect of caffeine on placental and fetal blood flow in human pregnancy. Am J Obstet Gynecol. 1983. 147:939–942.

27. Kramer MS, Sequin L, Lydon J, Goulet L. Socioeconomic disparities in pregnancy outcome: Why do the poor fare so poorly? Paediatr Perinat Epidemiol. 2000. 14:194–210.

28. Laraia BA, Siega-Riz AM, Gunderson C, Dole N. Psychosocial factors and socioeconomic indicators are associated with household food insecurity among pregnant women. J Nutr. 2006. 136:177–182.

30. Lokey EA, Tran ZV, Wells CL, Myers BM, Tran AC. Effects of physical exercise on pregnancy outcomes: a meta-analytic review. Med Sci Sports Exerc. 1991. 23:1234–1249.
31. Maccari S, Darnaudery M, Morley-Fletcher S, Zuena AR, Cinque C, Van Reeth O. Prenatal stress and long-term consequences: implications of glucocorticoid hormones. Neurosci Biobehav Rev. 2003. 27:119–127.

32. Micali N, Treasure J, Simonoff E. Eating disorders symptoms in pregnancy: A longitudinal study of women with recent and past eating disorders and obesity. J Psychosom Res. 2007. 63:297–303.

33. Mitchell EA, Ford RP, Stewart AW, Taylor BJ, Becroft DM, Thompson JM. Smoking and the sudden infant death syndrome. Pediatrics. 1993. 91:893–896.

34. Park JH, Lee JY, Park SW, Park SJ. Effect of delayed first childbearing on low birth weight and pre-term Birth. The Korean Society of Maternal and Child Health. 2004. 8:7–15.
36. Saba A, Di Natale R. A study on the mediating role of intention in the impact of habit and attitude on meat consumption. Food Qual Prefer. 1999. 10:69–77.

37. Siega-Riz AM, Herrmann TS, Savitz DA, Thorp JM. Frequency of eating during pregnancy and its effect on preterm delivery. Am J Epidemiol. 2001. 153:647–652.

38. Steer PJ. Maternal hemoglobin concentration and birth weight. Am J Clin Nutr. 2000. 71:1285–1287.

39. Sternfeld B, Quesenberry C, Eskenazi B, Newman LA. Exercise during pregnancy and pregnancy outcome. Med Sci Sports Exerc. 1995. 27:634–640.

40. Stewart DE, Raskin J, Garfinkel PE, MacDonald OL, Robinson GE. Anorexia nervosa, bulimia, and pregnancy. Am J Obstet Gynecol. 1987. 157:1194–1198.

41. The Korean Nutrition Society. Dietary reference intakes for Koreans. 2005. Seoul. Republic of Korea: The Korean Nutrition Society.
42. Treasure JL. The ultrasonographic features in anorexia nervosa and bulimia nervosa: A simplified method of monitoring hormonal states during weight gain. J Psychosom Res. 1988. 32:623–634.

43. Wadhwa PD, Sandman CA, Garite TJ. The neurobiology of stress in human pregnancy: implications for prematurity and development of the fetal central nervous system. Prog Brain Res. 2001. 133:131–142.
44. Weinstock M. Does prenatal stress impair coping and regulation of hypothalamic-pituitary-adrenal axis? Neurosci Biobehav Rev. 1997. 21:1–10.

45. Weissgerber TL, Wolfe LA, Davies GAL. The role of regular physical activity in preeclampsia prevention. Med Sci Sports Exerc. 2004. 36:2024–2031.

46. Wilcox AJ, Skjaerven R. Birth weight and perinatal mortality: the effect of gestational age. Am J Public Health. 1992. 82:378–382.

47. Yu KH, Yoon JS. A cross-sectional study of nutrient intakes by gestational age and pregnancy outcome (I). The Korean Journal of Nutrition. 1999. 32:877–886.




 PDF
PDF ePub
ePub Citation
Citation Print
Print









 XML Download
XML Download